Any head injury that leads to the appearance of signs of damage to the central nervous system poses a danger to the health and life of the victim. For some diseases, short-term conservative therapy is sufficient, while others require surgical intervention. Experts distinguish two forms of closed-type TBI, which follow a similar scenario, but at the same time have important differences. These are brain contusion and concussion - conditions that just a few years ago were considered different degrees of injury of the same type. The speed and correctness of diagnosis in such cases determines the patient’s prognosis and chances of recovery.
Any head injury threatens the life of the victim.
Symptoms and signs of brain contusion
By brain contusion we mean a closed-type TBI, which entails damage to organ structures. The pathology is a consequence of domestic, criminal, industrial, road transport sports or childhood injuries.
The condition is characterized by the formation of areas of necrosis in the tissues of the central nervous system.
The stimulator of negative processes is a change in the position of brain formations, a hydrodynamic shock to tissues, and displacement of an organ.
Symptoms of brain contusion depending on the severity:
- mild degree – loss of consciousness, which occurs in 100% of cases and lasts at least 2 minutes. Also, a mild bruise is accompanied by headache, amnesia, vomiting, dizziness, and a slight increase in temperature. Upon examination, a slight disturbance in cardiac and respiratory rhythm, nystagmus, and different pupil sizes become apparent. Often the picture is supplemented by meningeal symptoms in the form of stiff neck and failure of a number of reflexes;
- moderate degree - loss of consciousness for at least 10 minutes, signs of deep stupor and lethargy, deeper amnesia, headache, repeated vomiting. Respiratory and heart rhythm disturbances are pronounced, but may have a different clinical picture. Depending on the characteristics of the case, tachycardia and a noticeable increase in blood pressure or slowing of the pulse are possible. Neurological symptoms are pronounced and are accompanied by low-grade fever;
- severe degree - loss of consciousness lasts for hours and even days. Coma gives way to stupor. This degree of brain damage is accompanied by damage to the cardiovascular center, which is manifested by a serious disturbance in heart rhythm. Obviously pathological breathing, temperature rise to critical levels. The basic neurological picture is accompanied by a bilateral change in the shape of the pupils, signs of impaired sensitivity, motor activity, and reflexes.
In severe cases, loss of consciousness lasts for hours or even days.
Early diagnosis of brain contusion is the key to a favorable outcome of the injury. Even with a blurred clinical picture, pathology can be accompanied by phenomena that are dangerous to the health and life of the patient. TBIs of this type often occur with cerebral edema, focal hemorrhages, damage to the meninges, and the initiation of inflammatory and destructive processes in tissues.
Pathophysiological changes and intensive care in traumatic brain injury
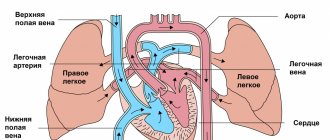
- Autoregulation of cerebral blood flow is one of the most important systems for maintaining the balance of intracerebral pressure. Small vessels of the brain respond to hydrostatic pressure and regulate their tone to maintain constant cerebral blood flow within the range of mean arterial pressure from 60 to 160 mm Hg. Art. Once the pressure regulation curve shifts to the right in severe brain injury, random changes in systemic blood pressure can lead to severe and linear changes in cerebral blood flow that lead to pathological and irreversible conditions such as cerebral hypoperfusion (cerebral ischemia) or hyperperfusion (cerebral hyperemia).
- Changes in cerebral blood flow volume and systemic blood pressure lead to dilation (vasodilation) or narrowing (vasoconstriction) of cerebral vessels. Cerebral vasodilation (dilation of the lumen of blood vessels) can lead to a decrease in systemic blood pressure. This causes an increase in cerebral blood volume and a rise in intracranial pressure. This vascular response can also be initiated by hypoxemia, dehydration, or hypocapnia (due to hyperventilation therapy).
- A decrease in cerebral perfusion pressure causes vasodilation (dilation) of cerebral vessels and a subsequent increase in cerebral blood volume. A decrease in cerebral perfusion pressure is often associated with a decrease in systemic blood pressure. By exceeding the capacity of autoregulation, hyperperfusion may increase the risk of brain congestion. Conversely, when systemic blood pressure falls below the limit of the body’s ability to correct it, a decrease in cerebral perfusion pressure and the occurrence of cerebral ischemia are possible.
- Excessive hyperventilation causes vasoconstriction (vasoconstriction) and decreased cerebral blood flow, leading to cerebral ischemia. As a result of cerebrovascular sensitivity to blood CO2 levels, dilatation (widening) of blood vessels in the brain caused by increased partial pressure of carbon dioxide (PaCO2) can increase intracranial pressure and contribute to an increase in blood volume in the brain (cerebral edema). If this occurs, the outcome for patients with severe traumatic brain injury may be poor. On the other hand, when the partial pressure of carbon dioxide (PaCO2) in the blood falls, the blood vessels in the brain constrict (vasoconstriction), leading to a decrease in blood volume and ultimately a decrease in intracranial pressure.
- An increase in endogenous catecholamines (sympathetic system-induced catecholamine release) causes peripheral vasoconstriction (vasoconstriction), which increases systemic blood pressure (neurogenic hypertension) after traumatic brain injury. As a result, systemic blood pressure will be maintained despite the presence of hypovolemia. Mannitol, as an osmotic diuretic, has historically been used in patients with increased intracranial pressure. When used off-label, however, mannitol causes excessive intravascular dehydration (dehydration). As a result of dehydration and hemodynamic disturbances, an unstable state of cerebral blood flow is formed with episodes of sudden hypotension. To prevent sudden catastrophic drops in blood pressure (hypotension) after traumatic brain injury (TBI), routine use of mannitol and intravascular dehydration should be avoided.
- Hyperglycemia also often develops after severe brain injury or a similar stressful event. High blood glucose levels after traumatic brain injury (TBI) appear to be associated with higher severity of brain injury and poorer neurological patient outcome. Until now, little is known about the role of blood glucose in the formation of secondary mechanisms of neuronal damage after brain injury. The best time to initiate glucose-containing fluids for nutritional maintenance is also questionable, as acute hyperglycemia (increased blood glucose levels) can alter the patient's neurological outcome. It remains to be seen whether hyperglycemia alone is capable of causing inflammation of brain tissue in acute critical conditions involving the accumulation of neutrophils.
Symptoms and manifestations of concussion
The brain, placed in the cranial cavity, is suspended in the cerebrospinal fluid. This protects it from collision with surrounding bones and prevents tissue irritation. A concussion that occurs as a result of an impact or a sharp displacement of the head relative to the axis of the body is accompanied by a hydrodynamic shock to the brain matter. In severe cases, this is complemented by a mechanical effect on the central nervous system due to its collision with the bones of the skull. In any case, this form of TBI occurs without damage to the structures of nervous tissues; everything is limited to a transient disruption of connections between neurons. Symptoms characteristic of a concussion:
- loss of consciousness – does not always develop, lasts from 5 seconds to several hours;
- intense headache;
- nausea, possible single vomiting;
- dizziness, problems with coordination and orientation in space, lethargy;
- memory loss is short-term or affects a short period of time, often the gaps are filled thanks to specialized therapy;
- slight change in heart rate, breathing;
- pallor or redness of the skin;
- slight increase in temperature in rare cases;
- ringing or buzzing in the ears, transient blurred vision;
- trembling of the eyeballs, changes in the size of the pupils or their asymmetry.
Nausea often occurs with BGM.
The clinical picture that occurs as a result of a concussion is in many ways reminiscent of a mild organ bruise. This complicates the process of diagnosing the condition for people not related to medicine. For this reason, the appearance of symptoms of damage to the central nervous system after a head injury is an indication for immediate seeking professional help.
What are the signs to distinguish a bruise from a concussion?
Technically, a bruise and a concussion are two completely different conditions.
In the first case, macrostructural damage is obligatory and obvious, and there is also a high probability of violating the integrity of the skull bones. A concussion leads to a transient disruption of intercellular connections in the nervous tissue, so the clinical picture is not so bright. Most often, its most severe consequence is a hematoma, and a bruise can cause traumatic swelling, hemorrhage, tissue crushing and massive death of neurons. The differences between a concussion and a bruise are given in the comparative table:
| Symptom | Brain concussion | Brain contusion |
| Loss of consciousness | Usually just a few minutes | Can last for hours, days, weeks |
| State of consciousness | Clear, although with signs of inhibition | From moderate stun to deep coma |
| Amnesia | Short term | May be long lasting |
| Vomit | One-time | Usually multiple |
| Cephalgia | Obsessive, moderate | Intense, persistent |
| Hyperthermia | Temperature is normal or low-grade | The rise in temperature dominates in all cases, the indicator can reach extreme levels |
| Heart rate disturbance | Within 60-90 beats per minute | From minor deviations to severe tachycardia or bradycardia |
| Breathing problems | Missing or not obvious | Obvious dysfunction of the respiratory system |
| Neurological signs | Nystagmus, skin and tendon reflexes are slightly impaired | Marked changes in muscle tone, reflexes, signs of meningeal syndrome, limb dysfunction |
The statistics of traumatic brain injuries are characterized by the predominance of concussion. Despite this, when symptoms characteristic of this form of TBI appear, doctors insist on conducting a full diagnosis in order to exclude contusion of a central nervous system organ.
With a bruise, severe tachycardia or bradycardia may appear.
Glasgow Coma Scale (GCS)
When assessing the severity of a patient’s brain injury, specialists take into account the level of neurological deficit (loss of function) and the level of clarity of consciousness. For ease of assessment in clinical practice, all these indicators (focal neurological symptoms, level of consciousness) were compiled into a Glasgow Coma Scale (GCS) by neurosurgeons from the University of Glasgow in 1974 (Professors Graham Teasdale and Bryan J. Jennett).
Glasgow Coma Scale (GCS) for traumatic brain injury:
Index | Responsiveness | Point |
Movement (D) | Performing spontaneous movements on command | 6 |
| Purposeful pushing away in response to pain | 5 | |
| Withdrawal of a limb in response to pain | 4 | |
| Pathological flexion in response to pain (decortication) | 3 | |
| Abnormal extension in response to pain (decerebration) | 2 | |
| No motor response | 1 | |
Speech (R) | Orientation in space and time | 5 |
| Confused speech, disorientation | 4 | |
| Says incomprehensible words | 3 | |
| Makes strange sounds | 2 | |
| No voice response | 1 | |
Eye opening (D) | Spontaneous | 4 |
| To the command, addressed speech | 3 | |
| To the pain | 2 | |
| Doesn't open his eyes | 1 | |
General value | 3-15 |
Note: Coma points = D + R + G. Patients scoring 3 or 4 on the Glasgow Coma Scale have an 85% chance of dying or entering a residual vegetative state. Patients who score more than 11 on the Glasgow Coma Scale have only a 5–10% chance of death or a residual vegetative state and an 85% chance of moderate disability or full recovery. Mean Glasgow Coma Scale scores correlate with the proportional odds of recovery.
The classification of traumatic brain injury is based on many factors. An alternative traumatic brain injury severity scale.
| Severity | Structural changes (MRI, ) | Loss of consciousness | Confusion | Post-traumatic (retrograde) amnesia | Glasgow Coma Scale (GCS), points |
| Light | Norm | 0–30 min (<20 min – 1 h) | Time of injury <24 h | <24 h | 13–15 |
| Average | Norm or pathology | >30 min but <24 h | >24 h | 1–7 days | 9–12 |
| Heavy | Norm or pathology | >24 h | >24 h | >7 days | 3–8 |
Doctors' advice
Basic first aid for closed head injury is universal, but diagnosis and further treatment must be entrusted to professionals. The specialist, independently or using special approaches, will determine exactly whether you are dealing with a concussion or bruise and will draw up a suitable treatment regimen. Only in this case will the victim’s recovery be as fast as possible, and the negative consequences after the injury will be minimal.
Knowing the signs, symptoms, and distinctive features of a bruise and concussion, you can independently understand the situation. In any case, the actions of the victim, his relatives or eyewitnesses must be the same - it is necessary to urgently call an ambulance so that professionals can take care of the patient.