Today we will talk about Her Majesty Migraine - how to live in relative harmony with it, how to relieve the excruciating headaches caused by this disease, and how you can reduce the frequency of attacks.
Dmitry Gonchar February 22, 20215 min read 915
Hemicrania or migraine is primarily a hereditary neurological disease associated with pathologically high sensitivity of cerebral vessels. Unfavorable external and/or internal factors periodically cause dilation and inflammation of these vessels, which results in attacks of severe headaches and other “signature” symptoms of migraine – sound and photophobia, nausea, etc.
The term “migraine” itself comes from a New Latin word that passed into the French language - hemicrania, which means “half of the head.” The symptoms of migraine were described in ancient Greek medical works, and the ancient Greeks considered evil forces to be the culprits of the disease (and it was proposed to drive out the evil spirit from the head by drilling a hole in the skull, but these are details :)).
Migraine as such does not pose a threat to the health and life of the person suffering from it. During migraine, the blood vessels of the brain do not undergo any lasting changes - they dilate and become inflamed only during an attack, and then return to normal. By the way, people suffering from migraines, in most cases, are characterized by a clear mind, good memory, high cognitive abilities - all this persists for many years. True, painful migraine attacks nullify all these positive aspects.
How to distinguish migraine from other types of headaches?
The signs of a migraine usually cannot be confused with anything, since its main and most common symptom is a strong, no, VERY STRONG headache, of a pulsating or bursting nature, most often localized in one half of the head (although sometimes the pain takes over the entire head). It can be concentrated both in the frontal or temporal regions, and in other areas. Movement, light, sounds, any physical activity and other factors aggravate migraine headaches.
A migraine attack or migraine attack often occurs in four stages:
1. Prodrome - a feeling of anxiety, a premonition of an impending attack. Occurs in just over 50% of migraine patients. Prodrome can manifest itself as irritability, depression, fatigue or, conversely, unhealthy activity, increased appetite, or simply a feeling of “knowing” that an attack is coming soon. The prodrome occurs in different ways: for some, a couple of hours before the attack, and for others, several days before.
2. Aura , which is manifested by various visual, tactile, gustatory, olfactory and other disturbances. We will tell you more about the aura below.
3. The headache itself is usually very severe. Its duration can vary from half an hour to 2-3 days, depending on the type and severity of migraine.
4. The postdromal period is a kind of “recovery” after an attack, usually accompanied by a feeling of weakness and apathy.
Severe migraine attacks may be accompanied by vomiting, dizziness, darkness in the eyes and other related symptoms. Many patients note that vomiting provides some relief from both the headache and the general serious condition during an attack.
What is migraine with aura?
Migraine can be with or without aura. Migraine aura is a whole symptomatic complex that appears either before or simultaneously with a headache attack. Aura with migraine occurs:
1. Visual , with flashes before the eyes, “fog”, glare, visual distortions and even loss of individual visual fields.
2. Auditory , accompanied by ringing or noise in the ears, and in severe cases, auditory hallucinations.
3. Sensory , in which taste and smell change.
4. Aphasic , when speech is impaired.
5. Motor , which is accompanied by difficulties in moving the arms and legs, up to the inability to walk.
6. Vestibular , with dizziness, loss of balance and even falls.
Several types of migraine aura can be combined at the same time, but they are all associated with vascular spasm that occurs in the brain at the beginning of the attack.
There is also a migraine without an aura - it manifests itself only as episodic headaches, without the symptoms described above.
Other types of migraines
There are also other types of migraine, which are much less common than “classical” migraine with or without aura. For example:
- cervical , with very severe headaches - it is usually associated with disturbances in blood flow in the vertebral artery;
- ocular migraine is necessarily accompanied by the symptoms described above for visual migraine aura (flashes, flickering, glare, loss of visual fields). Headache attacks with this form of migraine are short (maximum half an hour), and it is associated with pathology of blood flow in the occipital region of the cerebral cortex;
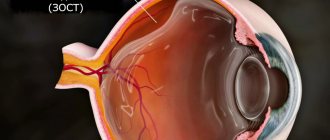
- retinal migraine – in which headaches are accompanied by short-term blindness, which is associated with spasms of retinal vessels;
- paroxysmal chronic - it is characterized by short attacks that repeat several times during the day;
- hemiplegic , with a feeling of severe weakness throughout the body and impaired sensitivity (paresthesia) on the half of the body opposite the side of the headaches. Develops against the background of circulatory disorders in the brain, attacks are short-lived (maximum hour);
- abdominal – usually occurs in children. It causes stomach pain, nausea, vomiting, and diarrhea;
- aphasic , in which speech disturbances begin at the very peak of pain.
By the way, there is another, extremely rare type of migraine, which has been called “ decapitated migraine ”. This type of disease is expressed only by a migraine aura, and the head does not hurt.
Definition of migraine
Migraines involve attacks of moderate to severe, often unilateral, throbbing, throbbing headaches that are worsened by exercise. A third of patients suffer from holocranial headache. Individual attacks are accompanied by lack of appetite (almost always), nausea (80%), vomiting (40–50%), photophobia (60%), sensitivity to noise (50%) and increased sensitivity to certain odors (10%) Signs of parasympathetic activation systems are observed in 82% of patients, most often with mild watery eyes.
When headaches are unilateral, they may switch sides during an attack or from one attack to another. The intensity of attacks can vary markedly from attack to attack. The duration of attacks, as defined by the International Headache Society (IHS), ranges from 4 to 72 hours.
In children, attacks are shorter and may occur without headache, only with severe nausea, vomiting and dizziness. The localization of headaches is often bilateral.
Causes of migraine
As already mentioned, migraine is a hereditary disease. Moreover, according to statistics, women suffer from it three times more often than men. Some modern researchers tend to see this as a connection with the hormones of the menstrual cycle, in the last phase of which the levels of certain hormones (progesterone, estrogen) drop in the female body - they say, this can provoke attacks. However, there is also a theory that women simply visit doctors more often for headaches, and therefore are more often diagnosed with migraine.
According to WHO, migraine usually begins simultaneously with puberty, causing the most severe suffering in 35-45 year old people. In any case, the disease recedes with age - due to both hormonal changes and a decrease in the elasticity of blood vessels.
In principle, migraine began to be studied in detail relatively recently - only in 1960. Before that, it was considered the lot of anxious people, a kind of mental disorder. Methysergide entered the pharmaceutical market, the disease was transferred to the category of physiological and began to be studied in more detail.
At the moment, it is known that migraine is directly related to mutations of certain genes - they provoke hyperactivity of brain neurons and excessive excitation in its areas responsible for processing sensory information (light, sound). Seizures can be caused by external stimuli - triggers , for example:
- lack of sleep (or excess);
- stress (and sometimes relaxation after stress);
- hunger, thirst;
- certain foods: chocolate, sugar, cheese, meat, salty foods, sometimes coffee (although in some cases coffee, on the contrary, helps relieve a migraine attack);
- alcoholic drinks;
- strong smells, sounds, light;
- excessive physical activity;
- climate and/or weather changes, etc.
It has also been proven that the development of chronic migraine can be associated with excess weight, depression, anxiety, certain diseases (for example, hypothyroidism), as well as uncontrolled and too frequent use of headache medications .
Therapeutic diet for migraines
Basic principles of therapeutic nutrition for migraine: regularity and moderation. As a rule, an attack can be provoked by both lack of nutrition (fasting, a sharp decrease in the nutritional value of the diet, long breaks between meals) and excess (overeating, excessive consumption of fats and carbohydrates), as well as the inclusion of unusual foods in the menu (during tourist trips , meals in national restaurants, etc.).
The diet should be selected individually. The same foods can cause an attack in one person and stop it in another person.
How to treat migraine?
No way. It is impossible to completely cure any disease caused by genetic defects. But there is good news! Nowadays medicine, unlike ancient Greek, no longer offers drilling holes in the skull to expel the evil spirits of migraines, but now there are medications that can:
- alleviate the condition during an attack;
- slightly reduce the intensity and frequency of attacks.
Since it is impossible to completely get rid of migraines, you need to strive to bring them into “perfect balance.” That means:
- no more than 2 attacks per month;
- The duration of each attack is no longer than 2 hours.
What can be done for this?
1. Identify your triggers (factors that provoke an attack) and, if possible, avoid them.
2. Talk to your doctor about medications that can help make attacks less painful, and start taking them. What kind of drugs are these?
Drug prevention of migraine
This type of therapy is prescribed by a doctor according to strict indications, as it requires daily medication, which is associated with the development of side effects and complications. However, drug prevention of migraine is the only option for those people who:
- does not feel a significant effect from the treatment of migraine attacks with analgesics and specific anti-migraine drugs;
- has contraindications for taking these drugs;
- suffers from too frequent attacks (more than twice a month), attacks deprive one of his ability to work for two to three days;
- forced to take medications more than twice a week.
Drug prevention in these cases allows you to avoid complications such as chronic migraine, status migraine, and abuse headache (pain as a result of medication abuse).
Among the drugs used for the medicinal prevention of migraine, the most commonly used drugs are from the group of beta-blockers, calcium channel blockers, antidepressants, anticonvulsants, MAO inhibitors, antiserotonin drugs and others.
Expert: Natalya Dolgopolova, general practitioner Author: Tamara Mutnovskaya
The material uses photographs belonging to shutterstock.com
Medicines for migraines and other headaches
For headaches (with migraine and not associated with migraine), the doctor may prescribe any drugs from the group of NSAIDs - non-steroidal anti-inflammatory drugs. All medications in this group relieve headaches by stopping inflammation of the vascular wall. Moreover, some NSAIDs contain not only an analgesic component (painkiller), but also additional substances - for example, sedatives or antispasmodics (relieving spasms).
Based on the presence or absence of these additional substances, these drugs are divided into:
- one-component
- multicomponent (combined).
Single-component include drugs containing only the NSAID itself, for example:
- acetylsalicylic acid - Aspirin, Upsarin, etc. To relieve an attack, a single dose of 500 mg or more is usually prescribed.
IMPORTANT! Effervescent tablets are absorbed faster, so if you have a migraine, it is better to take them, especially if the attack is accompanied by nausea.
IMPORTANT! Drugs for the prevention of strokes and heart attacks containing acetylsalicylic acid (Trombo ACC, Cardiomagnyl, Aspirin Cardio, etc.) are not suitable for our purposes, since the dosage of the active substance in them is very low.
- acetaminophen (paracetamol) - Paracetamol, Efferalgan, Panadol, etc. It must be said that in order to combat migraines, paracetamol itself is not very effective, so it is better to pay attention to combination drugs containing it;
- ibuprofen - Ibuprofen, Nurofen, Brufen, etc. - as in the case of acetylsalicylic acid, the doctor may prescribe 500 mg or more of ibuprofen per dose to relieve migraine headaches;
- metamizole sodium - Baralgin, Analgin. IMPORTANT! It is undesirable to constantly take metamizole sodium preparations, since this substance can change the composition of the blood and also negatively affects the liver and kidneys;
- naproxen – Nalgesin, Naproxen. A popular remedy among people suffering from migraines, naproxen preparations are available both single-component and combined, and the average dosage for attacks is usually 500–750 mg;
- diclofenac – Diclofenac, Voltaren, etc.
- ketorolac (Ketanov) and lornoxicam (Xefocam) are very powerful analgesics. They, like some of the above drugs (for example, Baralgin), can be prescribed by a doctor for migraines not only in tablet form, but also in the form of injections.
In addition, if during a migraine attack the patient experiences severe nausea, an anesthetic drug from the NSAID group can also be prescribed in the form of suppositories used rectally - for example, Cefekon D with paracetamol, Indomethacin with indomethacin, Voltaren with diclofenac, etc.).
* * *
Among the multicomponent (combined) painkillers that are often used to relieve migraine attacks and headaches of other origins are:
- Askofen, Citramon - drugs with approximately the same content of acetylsalicylic acid, paracetamol and caffeine. IMPORTANT! To relieve migraine attacks, the doctor prescribes these medications only to those patients who do not have a tendency to vascular spasms and increased blood pressure (this is due to the caffeine content in both drugs).
- Pentalgin - however, it can be used for migraines only in consultation with a doctor. The fact is that different types of this medicine have different compositions and if, for example, Pentalgin ICN can alleviate an attack, then “ordinary” Pentalgin will not bring any benefit for migraines. By the way, the drugs Sedal-M and Sedalgin Neo have a composition similar to Pentalgin ICN.
- Tempalgin, which contains metamizole sodium (which we already discussed above and recommended not to take it regularly due to dangerous side effects).
- Spazmalgon - like Tempalgin, it also contains metamizole sodium, so the precautions should be identical.
- Andipal - in addition to metamizole sodium, contains phenobarbital - a substance that quickly becomes addictive.
Triptans for migraines
In addition to the listed “broad-spectrum” painkillers, special analgesics specifically against migraine are also available on the pharmaceutical market.
It is known that many people suffering from migraines, even with the help of a qualified specialist, cannot choose for themselves a truly effective painkiller from the NSAID group. But in the late 80s of the last century, the first special medicine against migraine, Sumatriptan, was developed in Germany. Under its influence, the vessels dilated during a migraine attack narrow, and therefore it is sumatriptan that still acts as the “gold standard” in the treatment of migraine. It belongs to the triptan , which was later replenished with several more similar substances, each of which can significantly make life easier for people suffering from migraines.
Preparations containing sumatriptan - Imigran, Sumamigren, Amigren, Antimigren, etc. Preparations containing other triptans - Rizamigren (active ingredient - rizatriptan), Zolmigren (zolmitriptan), Relpax (eletriptan), etc. There is a whole section on the Liki24.com website, which presents migraine medications from licensed pharmacies in Ukraine.
IMPORTANT! None of these drugs should be taken on your own initiative, without the consent of your doctor . The fact is that they all have a number of serious contraindications for use (primarily arterial hypertension, ischemia, varicose veins, thrombophlebitis, etc.), as well as many possible negative side effects.
Before you start using triptans, you must undergo a medical examination with an electrocardiogram and some tests.
When taking triptans should also be discussed with your doctor. These drugs cannot be taken during an aura, in order to “anticipate” the pain - in this case, the effect will be the opposite: the aura will last, and the headache during the attack will be more intense.
Ergotamine derivatives for migraine
Another class of anti-migraine drugs are ergotamine derivatives (Nomigren, Caffetamine, etc.). These are “older” medications; in many countries, doctors do not prescribe them for continuous use, but use them only for emergency cases - for example, if the patient has been suffering from an attack for several days, and ordinary analgesics do not help (status migraine).
IMPORTANT! You cannot combine the use of triptans and ergotamine derivatives - they must be “spaced” apart by at least 24 hours.
IMPORTANT! Ergotamine derivatives have many contraindications for use, including pregnancy and lactation, ischemia, arterial hypertension, glaucoma, vascular diseases, etc.
How to understand that the chosen analgesic is effective?
A properly selected migraine medicine must meet the following conditions:
- completely relieve the headache no later than 4 hours from the moment of administration;
- relieve nausea and photophobia in the first 2 hours after administration (during the same period, the headache should stop “pulsating” and gradually subside);
- effectively stop every or almost every attack;
- the attack should not be repeated the next day;
- During an attack, a single dose of the drug is sufficient (there is no need to take it additionally or any additional medicine).
If the analgesic does not meet these requirements, you should consult your doctor about choosing another drug that is more effective for you.
Medicines for nausea during a migraine attack
Nausea and/or vomiting during a migraine attack is not only unpleasant, but also harmful, since it does not allow the analgesics taken to be absorbed normally. Therefore, if nausea sets in, it is advisable to take an antiemetic drug - Ondansetron, Cerucal or others. They can even be taken simultaneously with an anesthetic, unless otherwise indicated in the instructions for these drugs (see the section “Interaction with other drugs”).
IMPORTANT! At the beginning of the attack, even before the onset of nausea and headaches, the function of the stomach is already impaired - contents are retained in it. To prevent the same fate from befalling the taken analgesic, which will remain in the stomach in an undigested form, corroding the mucous membrane and leading to even greater nausea, you can take any peristalsis stimulant (Motilium, Motorix, Domrid, etc.) as prescribed by a doctor.
Biofeedback for Migraine
The biofeedback technique has proven itself not only for the treatment of migraines, but also for relieving other types of headaches, muscle tension, chronic pain, as well as for correcting blood pressure and some types of cardiac arrhythmias, and insomnia.
The essence of the method is to train the ability to control various functions of the body: change the blood supply to organs and tissues, relax deep muscles. For this purpose, as a rule, special sensors and devices are used to visually track the effectiveness of exercises.
Preventing migraine attacks
To reduce the frequency and intensity of migraine attacks, doctors recommend:
- avoid stressful situations if possible;
- maintain a healthy sleep schedule, sleep in a dark and quiet room;
- give up foods that can provoke an attack (or at least reduce their quantity) - chocolate, baked goods, red wine, large amounts of coffee;
- follow a diet and drinking regime - try not to go hungry and drink enough clean, still water;
- add ginger and cayenne pepper to food in moderation;
- use medicinal plants - lavender (lotions) and mint (lotions, decoctions for oral administration).
Many people suffering from migraines are helped to reduce the frequency and intensity of attacks by compresses from ice packs, cold hand baths, massages (acupressure or collar area and head) - but all these measures must be selected purely individually.
In addition, it is recommended to take magnesium and vitamins B6 and B2 - they can be taken both as mono supplements and as part of mineral-multivitamin complexes. Of course, you should take any dietary supplements for migraines only after consulting your doctor.
Liki24.com targeted medicine delivery service wishes you good health!
Prevention
Most often, people suffering from migraines take medications to relieve pain
. This, of course, does not cure migraines, but it significantly improves the quality of life.
There are cases when migraine pain does not respond to painkillers. Then it is better to aim at preventing the development of a headache attack, i.e. prevention
. With its help, you can alleviate attacks of pain or completely eliminate them.
The first and simplest thing you can do is to identify the irritant and try to avoid it. The set of preventive measures includes:
- meditation;
- cold and hot shower;
- physical exercise;
- adhere to a sleep schedule;
- shoulder and neck massage;
- take vitamin B2, magnesium, fish oil and ginger;
- try to remain calm and less nervous;
- proper nutrition and diet (limit foods rich in tyramine).
There are also several proven folk methods for relieving migraine pain.
- Drink a herbal infusion (chamomile + willow root + raspberry leaves + lavender + peppermint).
- Oregano infusion (drink a glass 3 times a day).
- Mumiyo solution (drink before bed for 14 days).
- Cold compresses (or apply a cabbage leaf) and a contrast shower.
A distracting stimulus
may also help . This could be a piece of lemon peel without zest on the sore side of the temple or mustard plasters on the calves.
Definition and epidemiology
Migraine (M) is the primary form of headache (HT), manifested by repeated attacks of intense unilateral headache, as well as various combinations of neurological, gastrointestinal and autonomic manifestations. According to the Global Burden of Disease Study (GBD 2013), M ranks 6th among the leading causes of decreased quality of life in the world [1].
The prevalence of M in the world averages 14% and is more common in women [2]. According to a Russian population study, the prevalence of M in the Russian Federation in one year was 20.8%, which significantly exceeds global indicators [3]. In a study conducted in the Ural region in three social groups, the prevalence of M during the year was 15.9% (13.5% for M without aura and 2.4% for M with aura) [4]. The costs associated with M in the Russian Federation amount to about 1 trillion rubles. per year and are mainly determined by indirect costs due to decreased labor productivity and temporary disability [5].
Typically, M first appears between the ages of 10 and 20; at 30–45 years, the frequency and intensity of M attacks reaches a maximum; after 55–60 M, it usually stops. In some patients, typical attacks of M persist even after 50 years [6–9].
Classification
In accordance with the International Classification of Disorders Accompanied by Headache and Facial Pain (International Classification of Headache, ICHD-3 beta, 2013)1, M refers to primary (benign) cephalgia, which is not associated with organic damage to the brain or cerebral vessels and other structures located in the head and neck region [10].
ICHD-3 distinguishes three main forms of M: M without aura, M with aura, chronic M (CM), as well as complications of M, possible M and episodic syndromes that can be combined with M (Table 1).
Table 1. Classification of migraine according to ICHD-3 beta, 2013 [10]
In an attack of M, 4 stages are distinguished, which develop in a characteristic sequence: prodrome (harbingers of headache), aura (if present), headache stage, postdrome (resolution stage) [11]. It should be noted that not all M attacks manifest all stages [12].
Prodrome
(harbingers of headache), which is noted by approximately 50% of patients, occurs before an attack of headache (several hours or 1-2 days before) and is manifested by irritability, worsening mood, general weakness or, on the contrary, increased activity and appetite, thirst and fluid retention, muscle tension in the back of the head and neck, etc.
Migraine aura
- a complex of local completely reversible neurological symptoms that occurs immediately before an attack of headache or at its onset, manifests itself more often as visual (loss of areas of vision, bright flashes or colored zigzag lines), sensitive (tingling, numbness with a characteristic spread, “march” from the fingers up the hand and up to the face), less often motor and speech disorders, which gradually increase over 5-20 minutes and persist for no more than 60 minutes. The headache begins at the end of the aura, or within 1 hour after its end. Based on this feature, they distinguish between M without an aura and M with an aura. A migraine aura should not be confused with a prodrome.
GB stage
manifests itself as an intense pulsating unilateral (usually in the frontotemporal region or half of the head, but can be bilateral) headache, aggravated by normal physical activity, accompanied by nausea, less often vomiting, increased sensitivity to light and sounds; the duration of the pain phase without treatment or with ineffective treatment - from 4 to 72 hours.
Postdrome
occurs after headache subsides, manifests itself as fatigue, pale skin, yawning, difficulty concentrating, often irritability and can last up to 2 days.
The most common are M without aura
(up to 80% of cases) and
M with aura
(up to 20% of cases), the diagnostic criteria of which in accordance with ICHD-3 beta are given in Table. 2a and 2b.
Table 2.
1.1. M without aura
(formerly simple M) manifests itself as recurrent attacks with the typical characteristics of headache and associated symptoms described above.
1.2. M with aura
(formerly classical M) is characterized by the presence of an aura followed by a G.B. phase. Aura is often represented by unilateral, completely reversible visual, less often sensitive and other cerebral symptoms (for example, speech impairment), which develop gradually on average 10-30 minutes before the headache phase and/or accompany it. In this case, headache and accompanying symptoms meet the criteria of M without aura (items B, C, D of Table 2a). ICHD-3 beta identifies four subtypes of M with aura: M with typical aura, M with brainstem aura, hemiplegic and retinal M.
1.2.1. M with typical aura
2
.
Aura is represented by visual and/or sensory and/or speech disturbances, but without muscle weakness; with gradual development and duration of each symptom for no more than 1 hour.
1.2.2. M with stem aura
(formerly M basilar type, basilar M). It is distinguished by brainstem aura symptoms (dysarthria, dizziness, tinnitus, hypoacusia, diplopia, ataxia, decreased level of consciousness), but without muscle weakness. In this case, symptoms of a typical aura are almost always present.
1.2.3. Hemiplegic M.
The aura is characterized by completely reversible muscle weakness and typical aura symptoms; stem symptoms are possible. There are sporadic and familial hemiplegic M (4 types - depending on the type of gene in which the mutation CACNA1A, ATP1A2, SCN1A and with mutations in other genes was found).
1.2.4. Retinal M
. Aura manifests itself as a monocular visual disorder in the form of scintillations (flickering), scotoma, and blindness.
1.3. Chronic M
(previously transformed M). Manifests itself as daily or almost daily headache (more than 15 days per month for more than 3 months), of which migraine headache (see Table 2a) corresponds to at least 8 days per month; can develop both in patients with M without aura and with aura (Table 3a). An important auxiliary criterion for the diagnosis of CM is the presence of typical attacks of episodic M at the onset of the disease (criterion B).
Table 3a.
Diagnostic criteria for chronic M [10] Table 3b. Factors provoking an attack of M XM and drug abuse.
With uncontrolled and frequent use of analgesics, ergotamine drugs and triptans in patients with M, the formation of
drug-induced headache
(LIHB, or abusive headache) is possible [13-15]. LIHB is characterized by the occurrence of headache for 15 or more days per month for more than 3 months with excessive use of any means to relieve headache and is usually relieved by pain medication. Hypertension has the greatest clinical significance in Russia with excessive use of simple analgesics/NSAIDs and combined analgesics [13, 14, 16, 17].
For the diagnosis of LIHB, the main diagnostic criterion is “number of days per month using pain medications” (≥15 days per month for simple analgesics/NSAIDs and ≥10 days for triptans, combination analgesics, ergotamine derivatives and opiates). One of the characteristic symptoms of LIH is the patient awakening from headache at night and the need to take another dose of an analgesic. If the criteria for LIHB are met in a patient with CM, a dual diagnosis should be established, for example: “Chronic M. Drug-induced HD associated with the use of combined analgesics and triptans.”
1.4. Complications of M.
There are four complications of M [10].
1.4.1. Migrainous status.
A debilitating attack of M, lasting more than 72 hours, occurring in a patient with M without aura and/or M with aura, when prolonged headache and/or accompanying symptoms weaken the patient.
1.4.2. Persistent aura without infarction
. In a patient with M with aura, aura symptoms persist for one week or more without neuroimaging studies revealing an infarction.
1.4.3. Migraine infarction
. In a patient with M with aura during a migraine attack, one or more aura symptoms persist for more than 60 minutes, and neuroimaging studies reveal ischemic infarction in the area corresponding to the clinical symptoms of aura.
1.4.4. Epileptic attack caused by migraine aura
. A patient with M with aura has an epileptic seizure during or within 1 hour after an attack of M with aura. In the literature it is sometimes referred to as migraine-epilepsy (migralepsy).
1.5. Possible M.
An attack of headache meets all diagnostic criteria for M without aura (see Table 2a) or M with aura (Table 2b), except one. In such a situation, additional examinations should be carried out to exclude the symptomatic nature of M.
1.6. Episodic syndromes that can be combined with M
(formerly childhood periodic syndromes, periodic syndromes of childhood). The section includes three groups of syndromes.
1.6.1. Recurrent gastrointestinal disorders
, which include 1.6.1.1. Cyclic vomiting syndrome (episodes of stereotypical attacks of intense nausea and repeated vomiting repeated with predictable frequency) and 1.6.1.2. Abdominal M (repeated attacks of moderate or severe abdominal pain in combination with vasomotor symptoms (pallor), nausea and vomiting, with complete absence of symptoms in the interictal period (IAP)).
1.6.2. Benign paroxysmal vertigo
. Repeated short-term, sudden onset and spontaneously regressing attacks of dizziness; Children at MPP are healthy.
1.6.3. Benign paroxysmal torticollis
. Recurrent episodes of head tilt to one side with slight or no rotation and regress spontaneously; occur in children of the first year of life; normal neurological status in the MPP.
Provoking factors
An attack of M can be provoked by a number of endogenous and exogenous factors, possibly a combination of several triggers [18-24] (Table 3b).
Diagnostics
Diagnosis of M is exclusively clinical and is based on anamnesis data, a thorough analysis of the characteristics of headache and their compliance with the diagnostic criteria of the ICHD. A headache diary has diagnostic value, which allows you to distinguish an attack of M from an attack of tension-type headache and other headaches; to clarify the frequency of M (GB≤15 days/month - episodic migraine/episodic attacks M without aura or M with aura; GB≥15 days/month - chronic migraine), and also to identify the abuse of painkillers (drug abuse) [25-30]
When questioning patients with M, attention should be paid to possible comorbid disorders that significantly interfere with the quality of life of patients in the interictal period, contribute to the chronicity of M and require treatment. The most common comorbid disorders: depression, anxiety-phobic disorders (including panic attacks), night sleep disturbances, episodic tension-type headaches, drug abuse, and other pain syndromes [12, 17, 30, 31, 32. 33]. Severe mental disorders and drug abuse are indications for redirecting the patient to a cephalgologist (a specialist in the diagnosis and treatment of hypertension).
Objective examination.
As a rule, no organic changes are detected in the somatic and neurological status. If they are detected, additional examinations should be carried out to exclude the symptomatic nature of headache (Tables 4, 5).
Table 4. List of warning symptoms (“danger signals”) in patients with hypertension [26, 34, 37—39]
Table 5. List of diseases with which it is necessary to differentiate M [18, 22, 26, 33, 34]
Additional studies.
In patients with M, as in other primary headaches, most research methods (EEG, ultrasound and DS of the vessels of the head and neck, radiography of the skull, MRI/CT3, fundus examination) are uninformative; their implementation is impractical, since none of the methods reveals changes specific to M.
Laboratory and instrumental studies should be carried out only if symptomatic headache is suspected in the following cases: an atypical clinical picture, changes in neurological status, or the presence of “danger signals” [26, 34-38] (Table 4).
The diagnostic algorithm for patients with a complaint of hypertension is shown in the figure. In typical cases, if the clinical picture meets the diagnostic criteria of M and in the absence of suspicion of the symptomatic nature of headache, a diagnosis of one of the forms of M should be made, if necessary, current comorbid disorders should be included in the diagnosis and immediately, without additional examinations, the patient should be treated [36, 38, 45 -47].
Algorithm for diagnosing and managing a patient complaining of headache. Note: CI - comorbid disorders.
When making a diagnosis, one should rely on the diagnostic criteria M and use the ICHD-3 beta terminology [10, 48]. Establishing false “organic” diagnoses instead of the diagnosis “migraine” (dyscirculatory encephalopathy, spinal osteochondrosis, vegetative-vascular dystonia with cephalgic syndrome, hypertensive-hydrocephalic syndrome, headache associated with arterial hypertension, post-traumatic headache, etc.) is a mistake and leads to incorrect treatment and progression (chronization) of M [18, 49].
Concomitant forms of hypertension and significant comorbid disorders are also included in the diagnosis, for example: 1. Migraine without aura. Episodic tension headache. 2. Migraine with brainstem aura. Chronic cerebral ischemia. 3. Migraine with aura. Mixed anxiety-depressive disorder.
Differential diagnosis M
An attack of M often has to be differentiated with an attack of episodic headache, less often with an attack of cluster headache, chronic paroxysmal hemicrania, cervicogenic headache and episodes of headache in cerebrovascular diseases (stroke, arteriovenous malformations, dissection of the internal carotid and vertebral arteries, cerebral venous thrombosis, MELAS and CADASIL syndromes ); migraine aura - with transient ischemic attack (see Table 5). It must be emphasized that at the slightest suspicion of the symptomatic nature of headache (atypical course of M, the presence of neurological disorders in the status, deviations in laboratory parameters and other “danger signals”), it is necessary to conduct a thorough examination of the patient in order to clarify the cause of migraine-like cephalgia [30, 37, 39] .
In patients with CM, differential diagnosis should be made from chronic tension headache, as well as new daily persistent headache and hemicrania continua.
The differential diagnosis of CM and chronic tension-type headache, as well as LPH, is often difficult [50-52]. These difficulties are associated with the presence of TTH-like “background” pain along with frequent attacks of M in patients with CM [30, 53]. In this case, one should rely on early medical history: in patients with CM, in contrast to chronic headache, at the onset of the disease there are typical attacks of episodic M and other signs characteristic of M (hereditary history, typical migraine triggers, relief of headache during pregnancy), as well as Features of clinical manifestations at the time of visiting a doctor about chronic daily headache: most days with headache are represented by typical attacks of M.
LIHB resembles tension-type headache and manifests as a dull, pressing or squeezing pain throughout the head of mild to moderate intensity for ≥15 days per month for ≥3 months, which is significantly relieved by discontinuation of the drugs of abuse. The greatest intensity of pain in LIHB is observed, as a rule, in the morning, sometimes causing patients to wake up during night sleep (withdrawal pain), forcing them to take an anesthetic drug. Typical complaints are feelings of fatigue, lightheadedness, decreased performance, difficulty concentrating, irritability, and sleep disturbances. Fear of the appearance or increase of pain leads to taking analgesics “for future use,” which contributes to increased abuse [13].
It should be noted that in one patient M can be combined with other types of primary (TH; headache associated with physical or sexual activity; headache associated with cold stimuli, etc.) and secondary (LITH; cervicogenic headache; headache associated with dysfunction of the temporal -mandibular joint, etc.) cephalgia. In such cases, it is recommended to reflect all these forms in the diagnosis, for example, “Migraine without aura. Episodic tension-type headache with pericranial muscle dysfunction" or "Chronic migraine. Drug-induced headache associated with the use of triptans. headache associated with dysfunction of the temporomandibular joints.”
Etiology and pathogenesis
In 60-70% of patients, M is hereditary in nature [11, 54-56]. It has been shown that patients with M are characterized by increased excitability of neurons in the cerebral cortex and the spinal nucleus of the trigeminal nerve, which increases under the influence of endogenous and exogenous migraine triggers. Migraine headache is based on neurogenic inflammation and secondary vasodilation, which develop as a result of the release of pain vasodilator peptides from the perivascular fibers of the trigeminal nerve (including calciotonin gene-related peptide (CGRP) and activation of pain receptors in the walls of blood vessels (primarily the vessels of the dura mater Pain impulses enter the sensory cortex of the brain, which forms the sensation of pulsating pain [13, 22, 49, 57, 58].
The mechanism of migraine aura is associated with the spread in the direction from the visual cortex to the somatosensory and frontotemporal areas of a wave of neuronal depolarization (spreading cortical depression (SCD), the speed and topography of which determine the pace, nature and sequence of aura symptoms.
Treatment
Treatment of M is primarily aimed at alleviating the course of the disease (attacks of hypertension and the inter-attack period), improving the quality of life of patients and preventing chronicity of the disease. Treatment includes: 1) relief of a pain attack; 2) preventive therapy; 3) patient education (behavioral therapy) [26, 49, 59, 60].
Treatment of patients with uncomplicated M can be carried out at the stage of primary care by both a neurologist and a general practitioner. Patients with severe M, including CM, multiple CIs, and drug abuse should be observed in specialized HD centers [26, 34, 61, 62, 63].
Treatment of an attack
The aim is to reduce the intensity, duration of the pain episode and accompanying symptoms, as well as to improve the general condition of the patient. To relieve an attack of M, analgesics and/or NSAIDs (preferably not combined), triptans, and less commonly ergotamine-containing drugs are used [34, 51, 64-71] (Table 6a-6c). Treatment of an attack should begin as early as possible (within the first 30 minutes of the attack). In patients with a short history of M and mild attacks, simple analgesics have a good effect (Table 6a).
Table 6.
It is permissible to use monocomponent analgesics for no more than 14 days a month to avoid the development of LIHB. Due to the high risk of LIHB, the use of combined analgesics containing caffeine, codeine and barbiturates should be limited (no more than 9 days per month), and in patients with a frequency of pain episodes of 5 or more per month, taking drugs from this group is not recommended. Due to the risk of agranulocytosis, the use of drugs containing metamizole sodium (analgin) is not recommended.
In a number of patients, lornoxicam (Xefocam) at a dose of 8 mg at the beginning of an attack of M (included in the Russian standard of primary health care for M) may be effective (insufficient level of evidence) [72].
In case of severe nausea and vomiting, 10-15 minutes before taking analgesics, it is advisable to use antiemetics, which reduce gastrostasis and improve the absorption of painkillers (Table 6b) [73-75].
The most effective and high level of evidence (A) are the specific drugs agonists of serotonin receptors of the 5HT1 type triptans (Table 6c), the indication for use of which is relief of an attack of M [49, 76-82]. Triptans have an advantage in patients with initially severe attacks and severe maladaptation, as well as with a long history of M, when the effectiveness of analgesics is significantly reduced.
In case of M without aura, triptans should be taken at the beginning of the attack (in the first 30 minutes), in case of M with aura - at the end of the aura phase/at the very beginning of the G.B. phase. If some triptans are ineffective, others should be tried, but to assess the effectiveness of each triptan, the drug must be used for at least 3 attacks [38, 49, 66, 83]. When regularly taking one or more triptans ≥10 days per month for ≥3 months, there is a high risk of developing overuse (triptan) headache.
One of the most effective triptans of the latest generation, which has the greatest cardiac safety due to a minimal constrictor effect on the coronary arteries, is eletriptan (relpax). According to a Russian multicenter open study [67], the therapeutic effect of eletriptan develops within 30 minutes, and 4 hours after taking the drug (at a dose of 40 mg at the first signs of headache), 93% of patients noted complete relief of both headache and accompanying symptoms (nausea /vomiting, phono- and photophobia); 97% of patients rated the tolerability of Relpax as good and satisfactory. The low percentage of side effects typical of triptans (primarily an unpleasant sensation of spasm in the chest) is due to the fact that, compared with other drugs of this class, eletriptan has a minimal constrictor effect on the coronary arteries. Relpax can be considered as the drug of choice for the relief of M attacks in elderly patients with initial signs of cardiovascular disorders.
Contraindications for the use of triptans are associated with their potential constrictive effect on the arteries: coronary heart disease (including myocardial infarction and post-infarction cardiosclerosis), occlusive peripheral vascular disease, stroke or a history of transient ischemic attack.
Ergotamine derivatives (ergot alkaloids), including in the form of combined agents, are less effective and safe [83, 84].
Preventative treatment
indicated for patients with frequent episodic and chronic forms of M. Preventive treatment is aimed at reducing the frequency and severity of attacks, overcoming the abuse of drugs to relieve hypertension, treating comorbid disorders and improving the quality of life of patients and is recommended in the following cases [12, 26, 74, 85—90] :
— ≥3 intense attacks of M within a month and ≥8 days per month with headache with adequate relief of attacks of M;
- severe and prolonged auras, even with a low frequency of M attacks;
- ineffectiveness or poor tolerability of drugs to relieve attacks;
— chronic M (number of days with headache ≥15 per month);
— severe comorbid disorders (depression, anxiety disorders, drug abuse, etc.) [31, 91];
— M subtypes that pose a risk for brain damage (stroke): migraine infarction or history of status migraine, M with brainstem aura, hemiplegic M;
— the patient himself prefers preventive therapy to alleviate the course of M and restore quality of life.
Preventive treatment is considered effective if, within 3 months of therapy, the number of days with headache is reduced by 50% or more from the initial level [91-96] (Table 7).
Table 7. Medicines with proven effectiveness recommended for the prevention of M
Principles of preventive drug treatment M:
The duration of the course of treatment is from 3 to 12 months (on average 4-6 months for M with episodic attacks, 12 months for CM), then an attempt is made to gradually withdraw the drug(s) or reduce their dosage.
Treatment begins with monotherapy with a drug with proven effectiveness; if monotherapy is insufficiently effective, a combination of 2 or even 3 drugs from different pharmacological groups, also with proven effectiveness, may be more effective, starting with the minimum recommended doses.
When choosing a prophylactic agent, concomitant/comorbid diseases should be taken into account. It is preferable to choose a drug that is also effective in treating concomitant pathology (for example, a beta blocker in a patient with M and arterial hypertension, an antidepressant in a patient with M and comorbid depression).
The drug should be started with a minimum dose, increasing it to an adequate therapeutic dose over a period of time sufficient for the development of a clinical effect (the initial effect is usually achieved after 1 month of treatment at an adequate dose, the maximum after 2-3 months) or until side effects appear.
To minimize side effects, it is advisable to slowly increase the dose.
If the therapeutic effect is not obtained within 2-3 months of therapy, then the drug is replaced with another or a combination of drugs.
It is necessary to avoid situations leading to excessive use of painkillers: due to insufficiently effective prevention (due to an incorrectly selected drug or its insufficient dose) and/or the influence of treatment of a concomitant disease (for example, taking NSAIDs in connection with concomitant back pain can increase drug abuse and promote chronicity M).
To increase the effectiveness of treatment, patients should follow recommendations for lifestyle modification - eliminating potential triggers of M attacks and factors of chronicity of the disease (abuse of analgesics, stress, excessive caffeine consumption).
In patients with episodic attacks, beta blockers (metoprolol, propranolol), candesartan, AEDs (valproic acid, topiramate) are effective (level A); as well as antidepressants (amitriptyline and venlafaxine) (level B) [12, 26, 28, 35, 64, 86, 94, 97-100]. Acetylsalicylic acid, riboflavin, coenzyme Q10, gabapentin and other agents are less effective (level C) (Table 7). For example, a special dosage form of coenzyme Q10, which penetrates the blood-brain barrier, has a moderate preventive effect (level C) when taken for a long period of 3 to 4 months (idebenone (Noben) at a dose of 60-90 mg per day) [12, 20, 28 , 74, 81].
Selective serotonin reuptake inhibitors (paroxetine, fluoxetine, citalopram, escitalopram, sertraline, etc.) do not have an evidence base in the prevention of M, but can be used to correct concomitant mental disorders (anxiety-depressive disorders, panic attacks, generalized anxiety disorder) [28 , 101].
Non-drug methods.
Biofeedback (BF) and cognitive behavioral therapy (CBT) are moderately effective (level of evidence B-C), aimed at overcoming stress, correcting pain behavior, and teaching psychological and muscle relaxation [12, 70, 75, 102-105] . CBT is primarily indicated for patients with emotional-personal, somatoform and senesto-hypochondriacal disorders; in severe cases, consultation and observation of a psychiatrist is indicated.
For patients with M and severe dysfunction of the pericranial muscles, post-isometric relaxation, massage of the collar area, manual therapy, therapeutic exercises, and acupuncture are recommended (level C) [103]. Greater occipital nerve blocks using corticosteroids and local anesthetics are recommended as an additional therapy in combination with other treatment methods (level B) [60, 81, 89, 92].
Neuromodulation.
As additional methods of treatment, including in forms resistant to all types of drug therapy (refractory CM), it is possible to use various instrumental methods, the therapeutic effect of which is associated with the influence on one of the main pathophysiological mechanisms of M - neuronal hyperexcitability (transcranial direct electrical stimulation and transcranial magnetic stimulation (TMS) (level B); stimulation of the occipital, supraorbital, and, less commonly, vagus nerves (level C) [26, 68, 92, 106, 107].
Occipital nerve stimulation
(SZN) can be used in the treatment of refractory forms of CM; the mechanism of the analgesic effect of the method is associated with the modulating effect of the peripheral electrical SNS on pain transmission, in particular on the activity of neurons of the trigeminocervical complex [109]. The results of several randomized controlled (with sham stimulation) studies of CHN in C.M. have been published. The best results were observed with combined occipital and supraorbital neurostimulation [107].
TMS can be used to relieve attacks of M with aura (level C) - TMS with single stimuli, as well as for preventive treatment (level B) - rhythmic TMS (rTMS) and TMS with single stimuli. When repeated magnetic stimuli are applied above the patient's head at a certain frequency during rTMS, long-lasting neuroplastic effects can occur that remain after the end of stimulation and depend on the frequency of the delivered stimuli [92]. Various stimulation protocols have been proposed for rTMS, but in the preventive treatment of patients with severe M, the best results were obtained with high-frequency rTMS of the motor cortex [106].
Treatment of chronic M.
Due to the severe course of the disease and multiple comorbid disorders, optimal management of patients with CM should be carried out in specialized centers G.B. The goals of treatment are to reduce maladjustment and improve quality of life by reducing the frequency, duration, intensity of headaches and reducing the use of painkillers [32]. The selection of drugs is carried out taking into account comorbid disorders; The duration of treatment should be at least 1 year.
Topiramate and botulinum toxin type A (BTA) drug Botox have proven effectiveness in CM, including in patients with drug abuse (level A) [17, 94, 99, 108, 109] (see Table 7). Topiramate is prescribed for a long course (12 months) with dose titration of 25 mg per week, starting from 25 mg to 100 mg per day.
Botox is so far the only drug approved both in our country and in other countries for the preventive treatment of hypertension specifically in patients with CM; Specific treatment regimens and doses have been developed for this drug [86, 110, 111]4. For example, the level of evidence for the effectiveness and safety of another BTA drug, Lantox, the use of which is permitted in the Russian Federation for severe forms of M, does not correspond to the level of A for CM, and the doses and schedule of administration also differ.
Botox can be used if previously administered courses of preventive treatment are ineffective or used as a first-line drug in the presence of contraindications to taking tablet preventive drugs, as well as in combination with these drugs. In the absence of contraindications to tablet drugs, the choice of Botox as a first-line prophylactic drug is the patient’s right (i.e., possible if the patient himself has the appropriate desire) [101].
The mechanism of action of Botox is associated with the interruption of neurogenic inflammation, which leads to sensitization of peripheral nociceptors and subsequently to central sensitization [92]. The drug is administered intramuscularly strictly in accordance with the special PREEMPT protocol in 7 muscle groups of the head and neck ( mm. frontalis, mm. corrugator supercilii, m. procerus, mm. temporalis, mm. occipitalis, mm. trapezius and mm. paraspinalis cervicis
); the total dose per procedure is 155–195 units [108, 111]. The analgesic effect develops gradually during the 1st month after injections and persists for at least 3 months; To achieve sustainable improvement, at least 3 repeated injections every 3 months are recommended [109, 112]. Failure to comply with the recommended protocol for BTA administration (changes in the number and location of injection points, drug dose and/or frequency of procedures) may lead to insufficient or complete treatment failure
Treatment of M combined with LIHB.
Despite the lack of sufficient evidence, the following approaches to the prevention and treatment of overuse headache are widely and successfully used throughout the world [15, 26, 60, 68, 99, 113, 114].
The main stages of treatment for LIHB include: behavioral therapy (explaining the role of abuse in the formation of a chronic pain pattern and the need to stop taking painkillers); o painkillers for at least 1-1.5 months in an outpatient or inpatient setting “dry” or under the guise of drug detoxification. Detoxification regimen: 1) dexamethasone 4-8 mg (level of evidence B [115]) per 200 ml of saline intravenously drip for 7-10 days in a row in the morning or prednisolone orally (1 g per kg of body weight; on average 60 mg per day with a gradual decrease doses by 1-2 t every 3 days for 1-2 weeks until discontinuation); 2) amitriptyline 20 mg (2.0 ml) per 100 ml of physiological solution intravenously 7-10 days in a row in the evening; 3) rehydration (saline infusion 200-400 ml/day, at least 2 liters per course); selection of an alternative pain reliever from another pharmacological group: in patients with triptan or ergotamine abuse, it is possible to use short courses of long-acting NSAIDs: naproxen (500 mg/day) or flupirtine (100-300 mg/day) for no more than 4 weeks [93, 114]; for LIHB associated with excessive use of analgesics, triptans or ergotamine preparations can be recommended for no more than 8 days per month; preventive drug therapy for the initial form of headache (episodic M); since most patients with M and LIH suffer from CM or frequent episodic M, all principles of treatment for CM apply to them; the most effective in patients with a combination of M and LIGB are topiramate (50-200 mg/day) (evidence level A), amitriptyline (50-100 mg/day) (evidence level B) and injections of onabotulinumtoxin type A (Botox) (evidence level evidence A) [111, 112]; prevention of relapse of LIHB (further lifelong monitoring of the frequency of painkillers taken
Diagnostics
If you have migraines or a family history of migraines, a doctor trained in headache treatment (neurologist) will likely diagnose migraines based on your medical history, symptoms, and physical and neurological examination.
If your condition is unusual, complex, or suddenly becomes severe, tests to rule out other causes of your pain may include:
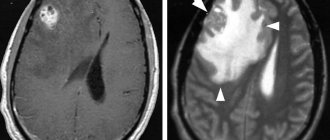
- MRI . MRI scans use a powerful magnetic field and radio waves to produce detailed images of the brain and blood vessels. MRI helps doctors diagnose tumors, strokes, brain bleeding, infections, and other brain and nervous system (neurological) diseases.
- CT scan . A CT scan uses a series of X-rays to create detailed cross-sections of the brain. This helps doctors diagnose tumors, infections, brain damage, bleeding in the brain, and other possible medical problems that may be causing headaches.