Cerebral edema is a nonspecific reaction to the influence of various damaging factors (trauma, hypoxia, intoxication, etc.), expressed in excessive accumulation of fluid in the brain tissue and increased intracranial pressure. Being essentially a defensive reaction, cerebral edema, if diagnosed and treated untimely, can become the main reason determining the severity of the patient’s condition and even death.
From this article you will learn the main causes and symptoms of cerebral edema in children, how cerebral edema in children is treated and what preventive measures you can take to protect your child from this disease.
Varieties, reasons
Brain edema occurs:
- vasogenic;
- cytotoxic;
- interstitial;
- osmotic.
The signs of cerebral edema depend on the type of developing pathology.
Causes of disease progression:
- Vasogenic edema occurs due to increased cerebral vascular permeability.
- Cytotoxic is the “swelling” of brain cells due to an increase in the amount of fluid inside them.
- Interstitial edema develops when there is increased pressure of the cerebrospinal fluid in the ventricles of the brain.
- Osmotic edema - with an increase in the osmolarity of brain tissue.
The most common reasons that cause brain swelling are: brain injury and disruption of its tissues in various pathologies.
Brain edema most often occurs in the following pathological conditions of a traumatic nature:
- brain contusion;
- fracture of the base of the skull;
- intracerebral hematoma;
- subdural hematoma. The prognosis of surgery for cerebral edema depends on its size.
The described pathology develops against the background of such organic brain lesions:
- ischemic and hemorrhagic stroke;
- hemorrhage under the arachnoid membrane;
- tumors;
- infectious diseases - encephalitis (inflammation of brain tissue) and meningitis (inflammation of the meninges).
Extracranial causes of cerebral edema can result from:
- Quincke's edema is a severe allergic reaction of the body;
- infectious diseases - scarlet fever, measles, mumps;
- diabetes;
- liver failure;
- alcoholism.
On our website Dobrobut.com you will find more information about the causes of cerebral edema in a newborn child, the development of pathology in the elderly and other facts.
Treatment
Your treatment plan for pediatric brain tumors may include one or more of the following:
Surgical intervention
This method must be resorted to in almost all cases, either to remove a tumor or to perform a biopsy. For slow-growing tumors, this is the only treatment needed.
Radiation therapy
In this case, a narrow beam of high-energy radiation is directed at the tumor and a small area of neighboring tissue. For the treatment of children under 3 years of age, this method is used with great caution due to the risk of interfering with brain development.
Chemotherapy
This treatment method is used quite widely, especially in the case of aggressive, fast-growing tumors. Chemotherapy drugs can be taken orally, injected into a vein, into the cerebrospinal fluid, or directly into the cavity left by surgery.
Signs of cerebral edema
Symptoms depend on how quickly brain swelling develops.
Signs of acute cerebral edema:
- disturbance of consciousness - from slight stupor to a state of coma with cerebral edema;
- convulsions – occur as swelling progresses;
- muscle atony – develops after seizures;
- membrane symptoms.
Gradual increase in edema – additional symptoms of cerebral edema in adults:
- headache;
- nausea and vomiting that does not bring relief;
- movement disorders;
- visual and speech disorders;
- hallucinatory syndrome.
Signs indicating critical development of the condition:
- paradoxical breathing (deep breaths with long gaps between them);
- a sharp decrease in blood pressure;
- unstable pulse;
- increase in body temperature above 40 degrees Celsius.
The appearance of such signs indicates compression of the brain stem, which leads to death.
Types of brain tumors in children
Brain tumors can be classified as:
- Primary, that is, those that arose directly in the brain.
- Metastatic, which arose as a result of metastases from tumors of other organs entering the brain.
- Benign, non-cancerous, growing rather slowly.
- Malignant, cancerous. These tumors can be very aggressive and spread quickly to other parts of the brain.
Below we look at some common types of brain tumors in children.
Astrocytoma. Astrocytomas account for about half of all childhood brain tumors and most often appear between the ages of 5 and 8 years. Tumors of this type develop from glial cells and astrocytes. For these tumors, it is very important to know their growth rate (although 80% of them are slow-growing).
There are 4 main types of astrocytomas in children:
- Pilocytic astrocytoma (grade 1). These tumors are filled with fluid and grow very slowly. When these tumors occur in the cerebellum, surgery is necessary.
- Diffuse astrocytoma (grade 2) invades adjacent parts of the brain, making surgery to remove it quite difficult.
- Anaplastic astrocytoma (grade 3) is a malignant tumor that requires combined treatment.
- Glioblastoma multiforme (grade 4) is the most malignant of all types of astrocytomas.
Children may also experience:
- Brain stem glioma;
- Tumor of the choroid plexus;
- Craniopharyngioma;
- Tumor of germ cells;
- Medulloblastoma;
- Optic nerve glioma.
Diagnostics
Cerebral edema should be suspected if impairment of consciousness increases, meningeal symptoms are observed, and the patient's condition worsens.
Instrumental methods that are used to confirm the diagnosis of cerebral edema:
- computed tomography (CT);
- magnetic resonance imaging (MRI). This is an important diagnostic method - you can detect swelling of the spinal cord on MRI, and not just the brain.
Of the laboratory research methods, general and biochemical blood tests are important.
It is dangerous to perform a lumbar puncture for diagnostic purposes - displacement of brain structures and jamming of the brain stem in the occipital foramen of the skull may occur.
Convulsions at high temperature in a child
Convulsive syndrome itself is an incredibly broad topic; there are very, very many reasons that cause increased excitability of the brain. Today I want to tell you about convulsions that occur when a child has an elevated temperature.
In order to cause seizure activity in a healthy adult, he needs to be constantly intoxicated for weeks or take a very serious dose of poison. And a baby can develop seizures from a very small dose of a pathological agent. This is due to the fact that children, especially infants, have an immature central nervous system, and the barrier between blood and brain tissue is not as strong as in an adult.
Therefore, if an adult suddenly develops seizures against the background of complete health, then you need to look for a serious reason. Children, of course, also need to be comprehensively examined, but the reason may be simple, for example, a banal increase in temperature in response to an acute intestinal infection. Moreover, children react much more strongly to the infectious agent than adults.
Factors that provoke seizures in children
In newborns
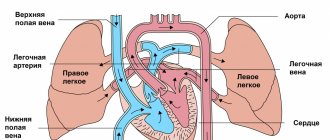
the most basic reasons are asphyxia (tight entanglement of the umbilical cord, premature rupture of amniotic fluid, placental abruption), birth trauma, intoxication, defects of the central nervous system, problems with the cardiovascular system.
In older age
Neuroinfection, measles, rubella, ARVI, and influenza are added to the previous causes. After vaccinations, it is extremely rare, but convulsions still occur. And, of course, the beginning of epilepsy as an independent disease.
Now you understand how many-sided seizures are, hiding many different ailments, so you need to understand each seizure scrupulously.
Convulsions are tonic
, when the victim seems to freeze in one position, stretches out, the head is thrown back or pressed against the body, and
clonic
, when a dynamic contraction of the flexor and extensor muscles occurs. And when the patient first freezes and then contracts, this is called tonic-clonic seizures.
There are many more subtleties in the manifestations of seizures, but I think this information is mainly needed by doctors.
Yes, an attack can occur anywhere, and the child can be injured. But this is not the main thing. The problem is that an overstimulated brain swells. Sometimes the swelling reaches such a size that it becomes wedged into the foramen magnum with disruption of vital functions.
How do febrile seizures occur?
I will dwell in a little more detail on one type of seizure that occurs in very young children under 6 years of age in response to elevated temperature (usually over 39 degrees). Hyperthermia can be of various origins, not necessarily with the flu, but also with intestinal infections, as well as with overheating and many other reasons.
Seizures should be considered febrile only in those children who have never had anything like this before. Otherwise, you need to figure it out; it is quite possible that the child has epilepsy. However, in any case, seizures are more likely to occur in children prone to convulsive brain activity, so it is important to be wary here. Remember that frequent attacks lead to intellectual impairment.
During convulsions, the baby loses consciousness, his head falls back, and his limbs stretch out. The teeth clench, foam appears, sometimes mixed with blood (the teeth injure the mucous membrane or tongue). Then possible twitching of the limbs. Breathing becomes intermittent due to lack of oxygen in the arterial blood, and the mucous membranes turn blue. Involuntary urination and defecation may occur. After an attack, the baby most often falls asleep.
what can you do
First, call an ambulance.
Second, ensure a safe position.
Place a pillow under the head and turn the victim on his side, thereby ensuring patency of the airway and preventing foreign bodies from entering the trachea.
And you don’t have to put anything in your mouth! No need to shove rags and unclench your teeth with sticks! It was not enough for a bone fragment to get into the respiratory tract. In general, there is no need to fuss, just help the victim survive the attack safely, without injury.
It is extremely rare that an attack leads to fatal respiratory failure, but most often this occurs with prolonged, uncontrollable convulsions (and you didn’t forget to call the doctors, right?).
And most importantly, febrile seizures can be easily avoided by controlling the temperature so that it does not rise above 38.3 degrees. It's much easier than fighting an attack.
Health to you and your children!
Vladimir Shpinev
Photo thinkstockphotos.com
Treatment of cerebral edema
The main principles of treatment for cerebral edema are:
- dehydration;
- improvement of metabolic processes in the brain;
- etiotropic treatment;
- symptomatic therapy.
What consequences of cerebral edema during stroke and other pathologies will accompany the patient depends on the timeliness and competence of the therapy.
Dehydration therapy
Its purpose is to remove excess fluid from brain tissue. Based on the appointments:
- osmotic diuretics (diuretics);
- magnesium sulfate and glucose solution - they enhance the effect of diuretics and also improve brain nutrition;
- L-lysine escinate - the drug is not a diuretic, but removes fluid.
Improving brain processes
For this purpose the following are appointed:
- metabolic drugs;
- glucocorticosteroids;
- oxygen therapy.
Etiotropic therapy
When treating cerebral edema, it is necessary to eliminate the causes of the development of the pathology and “destroy” the mechanism of edema formation. Destination:
- antibiotics;
- removal of tumors and hematomas;
- shunt operations, after which cerebral blood supply improves
This treatment is carried out after the patient’s condition has stabilized.
Symptomatic therapy
It is aimed at eliminating cramps, vomiting, pain, and so on. In addition to conservative therapy, surgical treatment can be used:
- decompression craniotomy;
- Ventricular drainage.
Second opinion for brain tumors in children
Despite the fact that brain tumors are often quite well identified on MRI and CT, errors in the interpretation of scan results do occur.
This may be due to a number of reasons, including:
- Low accuracy of equipment (for example, an outdated tomograph or one with defects that arose during operation);
- Lack of sufficient experience of a CT and MRI specialist.
Moreover, medical errors do not always indicate low qualifications of the doctor. They can happen even to fairly experienced CT scanners who simply don't see rare tumors very often. For example, a brain test may go to a doctor who has more experience diagnosing the lungs or liver.
In this situation, the only option to avoid incorrect treatment (which could endanger the child’s life) is to get a second opinion from qualified radiologists. The National Teleradiological Network (NTRS) invites you to get a second opinion from leading specialists from the best clinics and institutes in the country, with just access to the Internet. It doesn’t matter how far you are, just upload the scan results to our server and within a day the primary diagnosis will either be refuted or confirmed.
NTRS is a simple way to reduce the risk of scanning errors to a minimum.