Cerebral edema is a nonspecific pathology in which an increase in tissue volume is observed due to an increase in the amount of fluid contained in them. This pathological condition is not an independent disease, because it is formed due to the influence of various endogenous and exogenous factors.
A disease of this type usually poses a serious danger to a person’s life, because during its development nerves, arteries, tissues, and important brain structures begin to be compressed, which invariably leads to disruption of the central nervous system, visual and speech centers, prostate gland, and many others. the most important systems of the body.
Causes of cerebral edema
Cerebral edema occurs against the background of various neurological and other pathological conditions:
- Encephalitis due to tick bites, as complications after influenza.
- Infectious factors: neurocysticercosis (parasitic brain damage), cerebral malaria or meningitis .
- Ischemic, hemorrhagic and embolic strokes.
- Hydrocephalus as a consequence of meningitis or trauma.
- Ischemic encephalopathy due to birth injuries, high blood pressure, atherosclerosis.
- Venous thrombosis of intracranial sinuses.
- Brain tumors.
Diseases that provoke cerebral edema include diabetic ketoacidosis, liver failure, and electrolyte imbalance. Symptoms of cerebral edema may not appear immediately.
Cerebral edema in children with hydrocephalus is associated with increased intracranial pressure.
Etiology
There can be many reasons for the development of cerebral edema in children and adults. The most common of them are:
- Infections (toxins damage nerve tissue, which leads to the occurrence of an inflammatory process).
- Trauma to the brain and spine (for example, swelling of the brain after an accident, surgery, a strong blow to the head, a fall, etc.). The site of injury on the head after an injury in an accident may become very swollen, which usually occurs with a TBI.
- Tumor processes (cancer), in particular glioblastoma and cysts, localized in various parts of the brain, which lead to problems with the outflow of cerebrospinal fluid or displacement of brain structures.
- Hemorrhagic stroke, penetration of blood into the subarachnoid space.
- Embolism of the head vessels with the simultaneous occurrence of ischemic stroke.
- Heavy exposure to radiation.
- Poisoning with drugs, poisons, toxins (extremely dangerous during pregnancy).
- Encephalitis tick bite (the likelihood of dying from such a pathological process is high).
- The presence of metastases in the brain due to cancer.
- Metabolic encephalopathy (observed in severe renal or liver failure, in the last stages of alcohol dependence, in diabetes).
- Eclampsia.
- Water intoxication.
- Some types of vaccinations (controversial issue).
It happens that the brain often begins to swell in newborns who were born prematurely, or during a pathological course of labor. In this case, swelling in infants is traumatic.
The brain may begin to swell due to exposure to a number of toxins: gasoline, ethyl alcohol (and other types of alcohols), phenol, cyanide, etc. A huge number of medications that are used to treat various diseases and have a pronounced neurotoxic effect, in cases of overdose, can also lead to toxic cerebral edema. This category of medications includes: tranquilizers, antipsychotic drugs, tricyclic antidepressants, antihistamines.
Who's at risk
High-risk groups include people with severe diabetic ketoacidosis, as well as children who are experiencing acidosis for the first time. Factors that increase the likelihood of swelling are: dehydration, inflammation and blood clotting.
As a result, blood flow to the brain decreases and a cascade of ischemia and edema reactions occurs. Intracranial pressure increases, blood pressure and heart rate decrease. A brain herniation can compress vital structures in the brain stem. Patients with hyperactive ketoacidosis are at greater risk. High levels of ammonia above 200 µmol/L in the blood may be an indicator of the risk of developing intracranial hypertension.
In hepatic encephalopathy, cerebral edema is caused by a decrease in perfusion pressure in the brain vessels, swelling of astrocyte cells due to the accumulation of ammonia and increased glutamine production. Against the background of edema, intracranial pressure increases, ischemic contusion and brain hernia develop.
Often, cerebral edema develops in children who have suffered hypoxia and have hydrocephalus. Cerebral edema can complicate the course of strokes and traumatic brain injuries.
Pathogenesis
Brain swelling is a stepwise process in which acute injury results in the formation of cytotoxic, ionic, or vasogenic edema. What is edema? This is a combination of pathogenetic mechanisms. Cytotoxic edema is characterized by depletion of intracellular adenosine triphosphate (ATP), which impairs the active transport of osmolytes across cell membranes. Sodium and water ions accumulate in cells.
On the surface of cell membranes, the pressure and ratio of ions are disrupted, which leads to the movement of fluid into the extracellular space of the brain parenchyma from the vessels. This mechanism is also called ionic. During brain contusions, the activity of the Sur1-Trpm4 ion channel in endothelial cells increases, which leads to fluid accumulation.
A separate form of cytotoxic edema is vasogenic. The pathology develops due to increased permeability of the blood-brain barrier of the brain after a bruise, the release of inflammatory substances during infection and an increase in free radicals. As a result, fluid is released outside the cell along with blood plasma proteins.
As brain contusion develops, these mechanisms replace and complement each other, leading to swelling. It is believed that edema is preceded by an increase in intracranial pressure due to the fixed volume of the closed cranial cavity. At the same time, capillary perfusion - blood pressure in the vessels of the brain - decreases. The tissues do not receive enough nutrients and oxygen, and hypoxemia develops.
Classification
Brain edema occurs due to increased cerebral fluid content. In the pathogenesis of edema development, three forms are conventionally divided: cytotoxic, vasogenic and interstitial, or a combination thereof.
Vasogenic edema
Vasogenic edema is the most common form caused by disruption of the blood-brain barrier. Plasma proteins penetrate beyond the blood vessels, causing osmotic pressure to force fluid into the interstitial space of the brain. For example, endothelial growth factor, glutamate and leukotrienes locally increase the permeability of cells around the tumor. It is this, along with the weakness of the vascular walls, that leads to the entry of fluid with proteins into the parenchyma of the white matter. Swelling near tumors in 65% leads to cognitive impairment in patients due to displacement of brain structures.
Vasogenic edema is provoked by impaired vascular permeability and changes in perfusion pressure against the background of the following diseases and conditions:
- brain abscess;
- stroke;
- hypercapnia;
- encephalopathy due to hypertension;
- hepatic encephalopathy;
- metabolic disorders;
- diabetic ketoacidosis;
- lead poisoning;
- mountain sickness
Pathogenic microorganisms in meningitis disrupt the permeability of the blood-brain barrier to proteins and sodium ions. This leads to the accumulation of fluid in the intercellular space, as well as cell swelling due to passive hypoxia. Increased intracranial pressure disrupts connections between neurons.
Cytotoxic edema
Cellular or cytotoxic edema occurs within cells without damage to the blood-brain barrier. Pathology develops after a stroke or traumatic brain injury with damage to glial tissue, neurons and endothelial cells. The hemostatic mechanism in the cells is disrupted, and sodium accumulates in them, and the release of ions outside the membrane is disrupted. Anions try to restore neutrality on the surface of the membrane, which leads to swelling inside the cell.
Cytotoxic is associated with a change in the ion balance on the surface of cell membranes as a result of several reasons:
- hypoxic ischemic brain injury (drowning, cardiac arrest);
- brain injury;
- metabolic disorders of organic acid metabolism;
- hepatic encephalopathy;
- Reye's syndrome (acute liver failure);
- infections (encephalitis and meningitis);
- diabetic ketoacidosis;
- intoxication (aspirin, ethylene glycol, methanol);
- hyponatremia, or excess water intake without electrolytes.
Interstitial edema
One of the main causes of interstitial edema is obstructive hydrocephalus. Interstitial edema develops due to the leakage of cerebrospinal fluid from the ventricles of the brain into the interstitial space of the brain. Patients with hydrocephalus or meningitis are predisposed to this pathology. Increased pressure in the ventricles causes the contents of the ventricles to be forced out, resulting in swelling of the white matter.
Diagnostics
Various modern methods are used to diagnose the disease: MRI, CT, ultrasound and many others. If the form of the pathology is not fulminant, then a neurologist may suspect the presence of the disease, who will note the progress of deterioration of the patient’s condition, the increase in processes of impaired consciousness along with the symptoms of meningitis.
To confirm the diagnosis, magnetic resonance and computed tomography methods are used.
Lumbar puncture is not performed in all cases, because there is a certain danger that the cerebral structures, as a result of developing edema, change their location simultaneously with compression of the trunk. They also help in making a diagnosis: blood biochemistry, medical history, analysis of neurological status, neuroimaging examinations.
Considering the fact that cerebral edema causes serious complications, and the patient himself often requires emergency care, diagnosis should take a minimum amount of time. Diagnostics is performed in a hospital setting with simultaneous implementation of all necessary therapeutic measures. Afterwards the patient is placed in intensive care or intensive care.
Symptoms of cerebral edema
Cerebral edema, depending on the degree of changes, can be asymptomatic or symptomatic. The severity of the manifestations depends on the age of the person. In children, edema is compensated by the presence of fontanelles, and therefore the symptoms are different.
Cerebral edema has various manifestations:
- changes in consciousness, including coma;
- headaches and migraines;
- epilepsy;
- intoxication;
- intestinal obstruction (volvulus, intussusception)
- optic neuritis;
- hypertrophic pyloric stenosis
- macrocephaly.
General cerebral symptoms are associated with increased intracranial pressure:
- With a slow increase, patients experience morning headaches and vomiting without nausea, which is typical for brain tumors Transient dizziness occurs. Behavior changes slowly: patients become irritable and moody.
- With a rapid increase, the pain is paroxysmal, bursting, and severe. Vomiting does not provide relief. In patients, tendon reflexes increase, heartbeat and motor reactions slow down. Eye movements change, drowsiness sets in, speech and thinking are impaired.
With decompensation of increased intracranial pressure, coma develops, and with displacement of brain structures, breathing problems and heart contractions occur.
Signs of a pathological process
The main symptom of the developing anomaly is a progressive disorder of consciousness. At the initial stage, confusion of thinking and coordination failures are observed. At the last stage, a coma may occur. The first manifestation is often fainting, which lasts quite a long time. The patient experiences a convulsive syndrome, followed by complete weakening of the muscles. During the examination, the doctor notes signs of meningitis.
If a person has previously been diagnosed with cerebral disorders, swelling may not lead to loss of consciousness. The patient complains of persistent pain in the head, nausea, vomiting attacks that are not associated with food intake or complaints about the gastrointestinal tract. Accompanying symptoms include motor dysfunction, impaired visual perception, and hallucinations.
A 100% sign of severe compression of the brain stem is incorrect breathing. The patient breathes unevenly, deep sighs are replaced by a shallow intake of air into the lungs. The frequency of inhalations also varies. There are also sharp surges in pressure, and the heart rate is unstable. Often there is a strong increase in body temperature - over 40 degrees. It is very difficult to bring down the temperature. In an unconscious state, the eyeballs begin to diverge and “float.”
Diagnosis of cerebral edema
Early diagnosis of cerebral edema reduces mortality and improves functional capacity of patients after ischemic stroke. When pathology is established, decompression trepanation is performed. An increase in cerebral edema can be determined by symptoms of increased intracranial pressure: increased episodes of loss of consciousness, nausea and vomiting, headache, blurred vision, and hemiparesis. Among the listed signs, it is the unconscious state associated with damage to the reticular activating system and the thalamic-hypothalamic-cortical axis that is considered the most important clinical parameter. The degree of consciousness impairment is measured using the Glasgow Coma Scale.
In hemorrhagic stroke, there are other criteria for assessing the risk of cerebral edema. The likelihood of an enlarged hematoma increases with its initial significant size, the use of anticoagulants, and the early onset of symptoms. The risk of edema increases with hyperglycemia, elevated blood pressure, large hematoma size, and increased cerebral perfusion pressure.
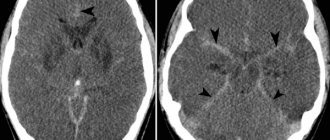
Swelling and dislocation of the brain during cerebral ischemia
CT picture - cerebral edema
Symptoms
Despite the causes and consequences of cerebral edema, in any case, the clinical picture of the disease will include focal and general cerebral symptoms. The order in which signs of pathology appear will depend on the underlying causes of hemorrhage. The form of the disease can be lightning fast (immediate help is required, there is a real struggle for the patient’s survival, the probability of death is high) and gradual (there is a short time period that allows you to easily prevent the death of the patient).
The main symptoms of edematous type cerebral hematoma include:
- Darkness of consciousness. This symptom will manifest itself in any case, regardless of the cause of the disease. Clouding of consciousness can be expressed in different ways: seizures of epilepsy, congestion, stupor, coma, clouding of consciousness, fainting. The development of swelling will always be accompanied by an increase in the depth of a person’s fainting state.
- Pain in the head. Headaches as a result of the development of edema are observed only in those patients who have a history of an acute form of some kind of brain pathology.
- Symptoms of meningitis. With the development of inflammation, tumor, and edema in the brain structures, meningeal symptoms often appear. Their presence in elderly patients should be alarming, because such symptoms are extremely dangerous for them.
- Focal symptoms. Typically, signs of this type are recorded at the stage of development of swelling. The patient may have impaired movement of the limbs, and paralysis of half the torso and face may develop. Problems with the functioning of the visual and speech centers, visual and audio hallucinations, and difficulties with coordination of movements are also often observed. Traditionally, cerebral edema, which leads to loss of consciousness in patients, leads to the inability to conduct higher nervous activity.
- Cramps. As the area of swelling increases, brief cramps may occur that last only a few minutes. The highest degree of this symptom is the development of muscle atony.
- Decreased blood pressure, unstable pulse. Dangerous symptoms, which clearly indicate that the edema spreads to the trunk, where the main central nervous system centers responsible for the vital functions of the body are located.
The consequences of cerebral edema will directly depend on the therapeutic effect, the form of pathology, the age of the patient and a number of other factors. Moreover, it is extremely difficult to eliminate edema completely (this is only possible in young patients). Most often, swelling cannot be completely removed, so the consequence of the disease is disability.
Treatment of cerebral edema
The goal of intensive care is to maintain breathing and normal hemodynamic parameters. The patient's head is elevated at a height of 30 degrees for the outflow of venous blood. Early enteral nutrition is started.
The following therapy methods are used:
- artificial ventilation for symptoms of brain dislocation;
- hyperventilation subject to monitoring blood oxygen saturation levels;
- administration of hyperosmolar solutions;
- barbiturate coma;
- craniotomy;
- hypothermia (lower body temperature).
Treatment protocols for edema depend on its cause. With vasospasm, it is important to increase the volume of blood plasma, and with hyperemia, diuretics and hyperventilation.
Conservative methods
Osmotherapy is a basic drug therapy for cerebral edema. It is rarely used for prophylaxis due to limited effectiveness due to early use. Hyperosmolar agents create an intravascular osmotic gradient that facilitates water excretion. The most commonly used drugs are mannitol and hypertonic saline. The latter helps to expand intravascular volume, increase cardiac contractility and intracranial pressure.
Osmotic diuresis with mannitol can cause intravascular dehydration and hypotension, and after it it is necessary to ensure adequate fluid replacement with isotonic solutions. Prolonged repeated use of hypertonic saline will lead to the development of hyperchloremic metabolic acidosis. Therefore, the drugs are used as an alternative for the treatment of symptomatic cerebral edema.
Surgical methods
Surgical intervention avoids deaths in cases of extensive hemispheric strokes. Especially in patients under 60 years of age, if the procedure is performed within 48 hours of the onset of symptoms. Decompression surgery is performed at an early stage of edema development, bone with a diameter of at least 12 cm is removed. After decompression, doctors monitor the development of subdural hemorrhage, external hydrocephalus, and prevent wound infection and divergence of blood vessels.
Surgery is used to remove a mass that is causing swelling of the brain - an intracerebral hematoma, abscess or tumor. Hematomas in the cortex larger than 3 cm in size, as well as in the cerebellum area larger than 2 cm must be removed.
Features of the treatment of cytotoxic edema
Cytotoxic edema is treated with mannitol or another osmodiuretic. Mannitol is used in a dosage of 0.5-1 g per kilogram of body weight intravenously. The effectiveness of osmotic agents lasts for the first 48-72 hours. In case of cytotoxic edema, they try not to reduce blood pressure if the mechanisms of autoregulation are preserved. Solutions are administered intravenously to increase the volume of circulating blood, and vasopressor therapy is carried out. The approach is used while maintaining the blood-brain barrier. Barbiturate anesthesia reduces swelling. Sodium thiopental is administered to reduce intracranial pressure below 20 mmHg. Art.
Features of the treatment of vasogenic edema
Vasogenic edema requires the use of angioprotective drugs. Escinulisinate restores the tone of vascular walls, enhances reabsorption and reduces interstitial edema. For vasogenic edema, glucocorticoids are used to reduce the permeability of the blood-brain barrier. Dexamethasone is usually administered simultaneously with antibiotics for meningitis. In vasogenic edema, mannitol, on the contrary, increases the flow of fluid into the tissue. To protect the brain parenchyma, antioxidants and agents to improve metabolism (Actovegin, Cortexin) are used.
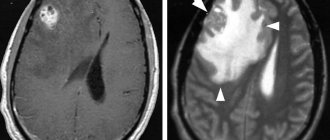
MRI diagnosis of some brain tumors
Co-author: Sotnikov V.V., Ph.D., chief physician of the Veterinary Clinic of Neurology, Traumatology and Intensive Care, St. Petersburg.
To select optimal treatment tactics and plan neurosurgical intervention for brain tumors, it is important to obtain the most complete diagnostic information not only about the location and histological properties of the tumor, but also about the severity and nature of perifocal reactions of the brain, which significantly influence the clinical manifestations of the disease. Significant perifocal edema reduces survival of patients with meningiomas (Motta L, Mandara MT, Skerritt GC.2012).
The most common, naturally developing reaction in focal lesions (primarily brain tumors) is perifocal edema, the development of which is based on the interaction of vascular and parenchymal factors.
It is customary to distinguish between vasogenic and cytotoxic cerebral edema, which can be combined and change quantitative relationships in the dynamics of development, depending on the cause that caused them. Perifocal edema in brain tumors is formed due to an increase in the volume of extracellular space as a result of the accumulation of fluid in it coming from damaged glial cells, and due to an increase in the permeability of the cell membrane of the capillary endothelium in the area surrounding the lesion. The prevalence of the perifocal edema zone is determined not only by the increase in water content in it, but also by the degree of regional demyelination of the fibers of the white matter of the brain.
The higher the degree of demyelination, the lower the lipid content in the perifocal zone and the more pronounced the disturbances in the processes of oxidation and phosphorylation, as well as the phenomenon of cerebral edema (Chan R.N., Fishmann RA 1978). In the progression of perifocal edema, two mechanisms play a major role: the entry of plasma proteins into the white matter of the brain and their binding to glial elements; an increase in further fluid flow into the perivasal space due to the osmotic gradient; and also, by a similar mechanism, the flow of fluid from the liquor system (Priden FR, Tsayumu M., Reulen HJ 1979; S.Reulen HJ, Graber S., Huber P., Jto U. 1988).
Numerous studies in humane medicine conducted at the Institute of Neurosurgery of the Academy of Medical Sciences of Ukraine indicate the existence of dynamic differences between the phenomena of edema and swelling of the brain. Edema is an increase in the content of free water in the intercellular interstitial spaces, and swelling is the accumulation of free water in the cells and bound water in the intercellular spaces. Intracerebral tumors, especially gliomas, are characterized by a predominance of edema in the perifocal zone (O.Yu. Chuvashova 2000).
As the volume of the tumor increases and the phenomena of intracranial hypertension increase, the protein composition changes both in the lesion and in the perifocal zone, in which these changes correlate with the degree of malignancy of the tumor. In this case, regional disturbances in the permeability of the blood-brain barrier develop, which increase cytotoxic edema. A specific role in this process appears to be played by a specific protein recently discovered in the brain—vascular permeability factor, which stimulates angiogenesis in tumor tissue and increases capillary permeability, and a correlation has been found between the concentration of this protein and the severity of perifocal edema.
The stated premises justify the search for the possibility of non-invasively obtaining diagnostic information characterizing the severity of perifocal cerebral edema in gliomas, taking into account their location, size and histological properties.
According to MRI data, the boundaries of gliomas and perifocal edema are optimally distinguished in T2 mode, since the signal intensity increases in the area of large accumulation of extracellular fluid. Fig 1(a)
Rice. 1A. T2 mode, perifocal edema is well expressed (white arrows). Rice. 1B. T1 mode without contrast injection, the right ventricle is absent, there is a displacement of the midline structures. Rice. 1B. T1 mode with the administered contrast agent “Magnevist”. An intense signal from the neoplasm is recorded (indicated by an arrow), perifocal edema is not visible.
The ability to identify the boundaries between the tumor and the area of perifocal edema increases with repeated MRI examinations after the introduction of magnetically enhancing drugs (Magnevist). Since Magnevist does not penetrate the intact blood-brain barrier, comparison of tomograms obtained before and after administration of the drug makes it possible to judge regional violations of the barrier permeability. Fig 1(A,B)
This is especially clearly manifested in astrocytomas of a typical structure, in which the function of the blood-parenchymal barrier at the tumor border and adjacent areas of the brain remains relatively intact until a certain time, so Magnevist does not penetrate into the tumor tissue.
In this regard, the zone of signal hypointensity is more clearly defined in the projection of the astrocytoma than in the area of perifocal edema. Assessment of the size and distribution of gliomas is more accurate on MRI than on CT (Kobyakov G.L., Konovalov A.N., Lichinitser M.R. 2001; Konovalov A.N., Kornienko V.N. 1985; Konovalov A.N. ., Kornienko V.N., Pronin I.N., 1997; Yamada K., Soreusen AG 2000).
There is greater accuracy and resolution of MRI in diagnosing gliomas of the cerebral hemispheres; this method is not comparable with the data obtained from CT examination. It allows you to more accurately determine the type of tumor, the degree of its anaplasia and the severity of perifocal cerebral edema, which is important for choosing the most rational anti-edematous therapy in the process of preoperative preparation and planning of surgical intervention (Fig. 2,3,4,5,6). In all figures, the results of MRI images are presented on the right, and CT scans in similar sections are shown on the left.
Rice. 2 a. CT. Displacement of the midline structures is noticeable (arrow). Swelling is not visible Fig. 2b. MRI. Perifocal edema is clearly visible
Rice. 3a. CT. Displacement of the midline structures is noticeable (arrow). Swelling is not visible Fig. 3b. MRI. Perifocal edema is clearly visible
Rice. 4a. CT. Displacement of the midline structures is noticeable. Edema is not visible. Fig. 4b. MRI. Perifocal edema is clearly visible. FLAIR sequence
Rice. 5a. CT. Perifocal edema is poorly visible, but the neoplasm is clearly visible (arrow) Fig. 5 B. MRI. The tumor is visible (large arrow), swelling is most clearly visible in the FLAIR program (small arrows)
Figure 6a. CT. A neoplasm is visualized in the area of the olfactory bulb Fig. 6b. MRI. T1 mode with contrast makes it possible to much more accurately assess the volume of the tumor and its boundaries
The above figures demonstrate that visualization of brain mass, perifocal edema and its extent is much more informative using MRI than CT. The use of contrast helps to improve visualization, as well as sequential execution of programs: to assess perifocal edema, it is advisable to use the FLAIR pulse sequence of MRI. T2-weighted images, which are widely used to detect pathological changes, do not always allow sufficient reliability to distinguish between affected areas and some normal tissues. Thus, on T2-weighted images, areas of pathological changes in brain substances often have a high signal and appear as brighter areas. Normal cerebrospinal fluid also has a similar high signal, which makes it difficult to identify pathological foci located near spaces filled with this fluid. To overcome this drawback, the FLAIR (Fluid Attenuated Inversion Recovery) technique has been developed, which suppresses the signal of free water (cerebrospinal and some other physiological fluids) while maintaining the basic T2-weighted image. FLAIR is better at detecting focal brain changes.
It should be noted that (according to our observation data of 35 patients) it is impossible to assess the presence and size of perifocal edema with an EEG study. The same situation exists in humane medicine. Changes in bioelectrical activity of the brain (EEG) in glial tumors are nonspecific and reflect the brain’s response to the lesion developing in it. In the preoperative period, EEG allows one to obtain objective information about the functional state of the brain, to identify the presence and localization of an epileptic focus in patients with epileptic seizures (Fadeeva T.N. 2004). It should be assumed that the tumor tissue is electrically neutral, so the EEG does not reflect the location of the tumor. However, when carrying out anti-edematous therapy (dexamethasone 1 mg/kg 2 times a day) before surgical treatment or for inoperable tumors, along with regression of neurological symptoms, normalization of the electrical activity of the brain occurs very quickly, which undoubtedly indicates the influence of perifocal edema on the electrical activity of the brain.
Bibliography:
- Chan R.N., Fishmann R.A. Brain edema: induction in cortical slices by polyunsaturated fatty acids //Science. - 1978. - V.201, No. 5607. — P.358—360.
- Priden FR, Tsayumu M., Reulen HJ Measurement of vasogenic brain edema clearance into ventricular CSF //Surg. Forum. - 1979. - V.30, No. 5. — P. 446—453.
- S.Reulen H.J., Graber S., Huber P., Jto U. Factors off ecting the extension of peritumoral brain oedema ACT-study //Acta Neurochir. - 1988. - V.96, No. 1-2. - P. 19-24.
- Motta L., Mandara MT, Skerritt GC Canine and feline intracranial meningiomas: an updated review. The Veterinary Journal, 192, 153-165. Source ChesterGates Animal Referral Hospital, Chester Gate Road, Telford Court, Unit EF, Chester CH16LT, United Kingdom.
- Chuvashova O.Yu. Characteristics of perifocal edema in gliomas of the cerebral hemispheres of varying degrees of anaplasia according to computed tomography and magnetic resonance imaging. Institute of Neurosurgery named after. acad. A.P. Romodanova AMS of Ukraine, Kyiv. 2000.
- Kobyakov G.L., Konovalov A.N., Lichinitser M.R. and others. Modern possibilities of chemotherapy in the treatment of malignant tumors // Modern minimally invasive technologies (neurosurgery, vertebrology, neurology, neurophysiology): Proceedings of the symposium. - St. Petersburg, 2001.—S. 251-253.
- Konovalov A.N., Kornienko V.N. Computed tomography in a neurosurgical clinic. - M.: Medicine, 1985. - P. 20-44.
- Konovalov A.N., Kornienko V.N., Pronin I.N. Magnetic resonance imaging in neurosurgery. — M.: Vidar, 1997.—S. 95-134.
- Yamada K., Soreusen AG Diagnostic imaging // Neurooncology. The Essentials. - New York, 2000. - Ch. 6. - P. 56 -77
Forecast
Cerebral edema after a stroke in adults develops under the influence of a number of factors. Epidemiological includes a history of hypertension or coronary heart disease. An important clinical criterion is a score on the neurological scale NIHSS for stroke above 20 in the dominant hemisphere or more than 15 in the non-dominant hemisphere. Development of nausea and vomiting the first day after a stroke. Systolic blood pressure is above 180 mm Hg. the first 12 hours after the attack. Decreased reactions to stimuli.
You can determine the risk of cerebral edema using MRI:
- occlusion of large arteries;
- damage to a large number of vessels;
- anomalies of the circle of Willis.
- infarction greater than 82 ml 6 hours after the onset of symptoms;
- outbreak of more than 145 or 14 hours after the first signs.
In case of traumatic brain injuries, even before hospitalization, it is important to begin neuroprotective therapy, the administration of corticosteroids and diuretics, which improves the prognosis in young patients.
What development options are possible?
Depending on the spread of edema, three syndromes of its development are distinguished:
- General cerebral – associated with an increase in intracranial hypertension. Headache, vomiting, visual disturbances, decreased pulse due to increased SBP and impaired thinking.
- Rostrocaudal growth syndrome is the spread of edema to the cortex, subcortical structures and brain stem. When the cortex is damaged, convulsions appear, in the subcortical areas - hyperkinesis, pathological reflexes. Impaired consciousness means damage to the hypothalamus. Trunk damage is manifested by respiratory depression and cardiovascular activity.
- Dislocation syndrome is manifested by loss of function of the oculomotor nerves, stiffness of the neck muscles, and impaired swallowing.
When the brain stem is wedged into the foramen magnum, many changes are irreversible.