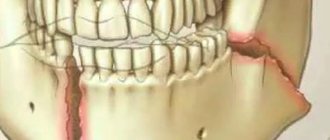
Dental implants solve a lot of problems in complex prosthetics, when there are difficulties in restoring acceptable function. When installing implants in the lower jaw, there is a significant risk of damage to any of the peripheral branches (inferior alveolar, mental, lingual nerve) of the mandibular part of the trigeminal nerve.
Although sensory impairment is a known and expected risk of some dental (medical and surgical) procedures, despite the highest quality care provided by the most qualified professionals, neurological complications are now the second most common cause of lawsuits against dentists in the United States.
Impaired sensitivity of oral structures is of great importance from a psychological and functional point of view. Anesthesia, soreness, or hypersensitivity may occur in the lips, cheeks, teeth, gums, or tongue. Drooling, choking on pieces of food or drinks, biting the lips or tongue, difficulty performing daily tasks such as shaving, applying makeup, talking, chewing, swallowing, kissing, smoking are a consequence of damage to the mandibular nerve and certainly cause extreme discomfort to the patient. especially if the patient was not warned about such complications in advance, and also if these problems are not completely resolved.
Nerve injuries do not always resolve on their own. However, in some patients they can be successfully treated using microsurgical techniques, provided they are performed promptly. In other patients, symptoms of nerve damage can be effectively managed with appropriate non-surgical therapy.
Causes of nerve damage
Injuries to the inferior alveolar, mental or lingual nerves result from compression, crushing, stretching, partial or complete rupture. In implantology practice, nerve rupture can occur when making an incision in the mucosa or when drilling into the bone to prepare an osteotomy hole for the purpose of inserting an implant. Nerve stretch occurs during prolonged retraction of the mucoperiosteal flap. Compression or crushing of the inferior alveolar nerve occurs as a result of the installation of a long implant. Injection of a local anesthetic may cause nerve damage through direct needle trauma or, more plausibly, through rupture of perineural or endonerval blood vessels with subsequent formation of scar tissue adhesions.
Prevention methods
Careful planning and skilled execution of manipulations minimize the risk of nerve damage. Panoramic and periapical radiographs, supplemented by scanning (if indicated), make it possible to determine the height of the alveolar process above the nerve, the medial lateral and vertical localization of the canal of the mandibular nerve and the mental foramen. Careful soft tissue incisions help avoid direct contact with the mental and lingual nerves, and gentle retraction of the flap minimizes indirect stretch of the nerve. When preparing the osteotomy hole and installing the implant, it is necessary to avoid damage to the mandibular nerve canal.
In the absence of sufficient height of the alveolar process to install an implant without the risk of damage to the canal of the mandibular nerve, lateralization of the mandibular nerve is indicated. Implants can be placed during this procedure (Figure 1-3).
Figure 1. Nerve reduction. The inferior alveolar nerve prevents adequate implant placement.
Figure 2. Transoral reduction of the nerve and its lateral retraction.
Figure 3. The implants are installed in the desired position and at the required depth, and the nerve is repositioned.
Classification of nerve injuries
Seddon described three types of nerve damage: neuropraxia, axonotmesis and neurotmesis. This classification is based on the relationship between the pathophysiology of nerve injury, the ability of the nerve to regenerate and clinical symptoms, which forms the basis for determining the prognosis of spontaneous recovery of sensitivity, indications and timing of surgery or other therapy.
Neuropraxia is a benign condition. There is temporary loss of sensation, but no anatomical damage to the nerve. Spontaneous recovery of sensitivity is possible within 4 weeks.
Axonotmesis is a more serious condition in which there is partial anatomical disruption of the integrity of the nerve and incomplete degeneration of the nerve distal to the injury. Initial symptoms of restoration of sensitivity do not appear until 6-8 weeks after the injury. Recovery may be incomplete (hypoesthesia) and is often accompanied by pain (dysesthesia).
Neurotmesis is a complete transection of a nerve or other complete disruption of its integrity with total degeneration of the portion of the nerve distal to the injury. There is little or no hope for spontaneous recovery. If the patient remains fully anesthetized for 3 months after injury, sensation is rarely recovered to a significant degree. Persistent and severe dysesthesia often develops. The progressive failure of the structures supporting the nerve and their replacement by scar tissue leads to the fact that, ultimately, 1 year after injury, even surgical intervention cannot restore nerve function in humans.
Grade
Documentation of nerve damage is necessary to evaluate sensory deficits, decide whether and when to perform surgery or other treatment, and for legal reasons.
The medical history should include the reason for the operation, the date of injury, and symptoms of sensory changes (if any).
A study is being conducted to assess the severity of sensitivity disorders, for which neurosensory tests are used (response to irritating stimuli, static electricity, vitalometer, etc.). Re-evaluation is performed every 4 weeks until sensitivity is acceptable or other surgery is required.
What diagnostic methods can a doctor prescribe for trigeminal neuritis?
The disease can be caused by various reasons, sometimes very serious (for example, cancer). Diagnosing them is not always easy. Depending on your complaints and information obtained during the examination, the neurologist may prescribe various instrumental studies and laboratory tests.
Magnetic resonance imaging of the head is most often used. This diagnostic method helps to identify pathological changes in the brain characteristic of multiple sclerosis and intracranial tumors.
The doctors of the medical center International Clinic Medica24 adhere to modern current standards - this guarantees that you will be prescribed all the tests necessary in your case, the doctor will not miss anything. At the same time, the coordinating doctor in our clinic will make sure that only truly necessary procedures are prescribed to you, so that you do not overpay for unnecessary things. All types of diagnostics are carried out using our medical center’s own equipment.
The material was prepared by Natalya Yurievna, a neurologist at the international clinic Medica24, Candidate of Medical Sciences Lasch.
Indications for microsurgery
The indications for surgery to correct nerve damage are based on the author's own experience, which includes the observation of more than 1000 patients and the performance of 375 microsurgical procedures to correct nerve damage, 21 of which resulted from dental implants between 1987 and 1996. year. The author's opinion regarding indications for surgical interventions is shared by many specialists in the field of microsurgery.
- Open (visible) nerve damage should be repaired as soon as possible. Such injuries usually occur during operations to install implants.
- Closed (non-visualized) damage must be repaired in the following order:
- Anesthesia lasting more than 3 months is reversed by suturing or nerve grafting.
- Dysesthesia that is unacceptable to the patient and lasts more than 4 months is eliminated with open exploration of the nerve through external decompression, internal neurolysis, excision of the neuroma, suturing and nerve transplantation.
- Severe hypoesthesia, unacceptable to the patient and lasting more than 4 months, can be eliminated by removing or partially unscrewing the implant, as well as by open exploration of the nerve and performing the manipulations described above.
- In general, patients who do not return to normal sensation within 4 weeks of surgery should be referred to a microsurgery specialist who can monitor the patient and modify the treatment plan as needed.
Anatomy of the Human Mandibular Nerve - information:
N. mandibularis, the mandibular nerve, the third branch of the trigeminal nerve, contains, in addition to the sensory one, the entire motor root of the trigeminal nerve, coming from the mentioned motor nucleus, nucleus motorius, to the muscles arising from the mandibular arch, and therefore innervates the muscles attached to mandible, the skin covering it, and other derivatives of the mandibular arch. Upon exiting the skull through the foramen ovale, it divides into two groups of branches.
Muscle branches: To the same muscles: n. massetericus, nn. temporales profundi, nn. pterygoidei medialis et lateralis, n. tensoris tympani, n. tensoris veli palatini, n. mylohyoideus; the latter departs from n. alveolaris inferior, branches n. mandibularis, and also innervates the anterior abdomen of m. digastricus.
Sensitive branches:
- N. buccalis to the buccal mucosa.
- N. lingualis lies under the mucous membrane of the floor of the mouth. Having given n. sublingualis to the mucous membrane of the floor of the mouth, it innervates the mucous membrane of the dorsum of the tongue throughout its anterior two-thirds. In the place where n. The lingualis passes between both pterygoid muscles and is joined by a thin branch of the facial nerve, the chorda tympani, emerging from the fissura petrotympanica. It contains the n. emanating from the nucleus salivatorius superior n. intermedii parasympathetic secretory fibers for the sublingual and submandibular salivary glands. It also contains taste fibers from the anterior two-thirds of the tongue. The fibers of n. lingualis, spreading in the tongue, are conductors of general sensitivity (touch, pain, temperature sensitivity).
- N. alveolaris inferior, through the foramen mandibulae, together with the artery of the same name, goes into the canal of the lower jaw, where it gives branches to all lower teeth, having previously formed a plexus, plexus dentalis inferior. At the anterior end of the canalis mandibulae n. alveolaris inferior produces a thick branch, n. mentalis, which emerges from the foramen mentale and spreads to the skin of the chin and lower lip. N. alveolaris inferior is a sensory nerve with a small admixture of motor fibers that leave it at the foramen mandibulae as part of n. mylohyoideus.
- N. auriculotemporalis penetrates the upper part of the parotid gland and goes to the temporal region, accompanying a. temporalis superficialis. It gives secretory branches to the parotid salivary gland, as well as sensitive branches to the temporomandibular joint, to the skin of the anterior part of the auricle, external auditory canal and to the skin of the temple.
In the area of the third branch of the trigeminal nerve there are two nodules related to the autonomic system, through which the salivary glands are mainly innervated. One of them is the ganglion oticum; the ear ganglion is a small roundish body located under the foramen ovale on the medial side of n. mandibularis. Parasympathetic secretory fibers come to it, consisting of n. petrosus minor, which is a continuation of n. tympanicus, originating from the glossopharyngeal nerve. These fibers are interrupted in the node and go to the parotid gland through n. auriculotemporalis, with which the ganglion oticum is connected. Another nodule, ganglion submandibular, submandibular node, is located at the anterior edge of m. pterygoideus medialis, over the submandibular salivary gland, under n. lingualis. The node is connected by branches to n. lingualis. Through these branches the fibers of the chorda tympani go to the node and end there; their continuation is the fibers emanating from the ganglion submandibular, innervating the submandibular and sublingual salivary glands.
Other treatments
In general, implant removal does not eliminate nerve damage when treating nerve damage early. Nerve injury most often occurs during incision, flap retraction, or during osteotomy hole preparation. Nerve compression by an implant, unless severe, rarely results in permanent nerve injury.
Moderate dysesthesia or a syndrome of long-term (more than 1 year) painful nerve injury can sometimes be successfully treated with non-surgical treatments. Antineuralgic drugs (carbemazepine, phenytoin, clonazepam, bacolofen) or antidepressants (amitriptyline, notriptyline, imipramine), topical applications (capsaicin) or local anesthetic components (mixeltin) taken orally help patients with severe dysesthesia for whom surgery is not indicated or did not help. Other therapies (eg, acupuncture, transcutaneous electrical nerve stimulation, psychological or psychiatric therapy, physical therapy) may play a role in treating the painful manifestations of nerve damage.
Treatment of trigeminal neuritis
Typically, treatment of the disease begins with medications:
- Anticonvulsants . Usually the drug carbamazepine or phenytoin, oxcarbazepine is prescribed; the doctor selects the dose individually. Over time, these medications may become less effective, in which case your doctor will increase the dosage. However, anticonvulsants have some side effects that may make it difficult to use them.
- Antispasmodics . Used together with anticonvulsants. For example, a neurologist may prescribe baclofen for you.
- Physiotherapy . Diadynamic currents, ionogalvanization with novocaine, and ultraphonophoresis with hydrocortisone help to cope with the symptoms of trigeminal neuritis.
If neuralgia manifests itself in the form of severe toothaches, painkillers are used, and ointments with anesthetics are rubbed into the gums.
If medications no longer help, the neurologist raises the question of surgical treatment of trigeminal neuritis. The following operations are possible:
- Microsurgical decompression . During the intervention, compression of nerve fibers by blood vessels is eliminated. Typically the incision is made behind the ear. The operation effectively eliminates pain, but after it a relapse may occur, complications such as hearing loss, numbness of the face, paresis and paralysis of the facial muscles.
- Transection of nerve branches . In this case, the transmission of pain impulses is disrupted.
- Radiosurgery (gamma knife). A special device generates a high dose of ionizing radiation, which damages nerve fibers. If painful attacks begin to bother you again in the future, the procedure can be repeated.
There are other surgical methods for treating this type of neuritis.
We will call you back
Message sent!
expect a call, we will contact you shortly
The trigeminal nerve provides sensation to the skin of almost the entire face and front of the head. It is mixed in structure, that is, it is responsible for both sensitivity and movement, but the motor fibers are thinner. Still, the trigeminal nerve is mostly sensitive. This determines the characteristics of the symptoms of the disease.
results
The prognosis for improvement or restoration of sensitivity after microsurgery depends on the age of the patient, the technical skills of the surgeon, and the length of the period between the fact of damage and surgical intervention aimed at eliminating its consequences.
From the author’s experience, in 80-90% of patients suffering from neurotmesis (usually expressed by anesthesia), operated on up to 6 months after the injury, it was possible to improve or restore sensitivity. Interventions performed more than 6 months after injury resulted in improvement in fewer patients. When operations were performed 1 year after the injury or later, the condition of less than 10% of patients improved. Patients who underwent surgery to correct dysesthesia after 9 months achieved improvement in 70% of cases, with worsening results as time to surgery increased.
Diagnosis of trigeminal neuritis: what happens during an appointment with a neurologist?
An appointment with a doctor begins with a conversation. First of all, it is important for a neurologist to get answers to three questions:
What is the nature of the pain? Is it typical for this disease ? With trigeminal neuritis, pain attacks occur suddenly, they are strong, painful and pass quickly.
Where does the pain occur ? When the trigeminal nerve is damaged, pain is localized on the face, in certain places.
What triggers lead to seizures ? Usually this is touching the face, exposure to wind, high and low temperatures.
You will be asked how long you have been experiencing symptoms, whether you suffer from any chronic diseases, and whether you are receiving any treatment. Then the neurologist will examine you and press on certain points on your face where the branches of the trigeminal nerve enter the skin. A general neurological examination will be performed to diagnose any possible medical conditions that may be causing your symptoms.