Magnetic resonance imaging allows you to visualize the network of blood vessels, determining the lumen, tone, and condition of the walls of veins and arteries. Blood clots are visible on MRI using special sequences and/or contrast enhancement, when the subject is injected intravenously with a “staining” solution of gadolinium salts.
MRI image of the brain in axial projection with signs of hemorrhage in the acute period
The diagnostic method is based on the use of a magnetic field that changes the position of water dipoles in the cells of the body. The tomograph sensors record the resonance of hydrogen atoms, and software converts the signal into a series of layer-by-layer photographs that are sent to a computer monitor. Scanning is carried out in axial, sagittal and frontal projections. Based on the images obtained, the doctor can reconstruct a three-dimensional image of the area of the circulatory system being studied.
What are blood clots and why do they appear?
Thrombi are clots that form from connections between blood cells. Platelets, sticking together in chains, form lumps that are attached to the walls of blood vessels. In some situations, blood clots form due to disorders of the hematopoietic system, in others - as a result of damage to the inner wall of the vessel.
Large growths inside the vein prevent blood flow from passing through the obstructed area. As a result, congestion forms in the veins, leading to varicose veins. When a blood clot blocks the lumen, a heart attack occurs—the death of tissue that has not received oxygen through the bloodstream.
The formation of blood clots is influenced by several factors from a person’s daily life:
- Sedentary lifestyle. Lack of active mobility leads to stagnation of blood in the lower legs. Therefore, constantly sitting at a computer, as well as choosing an escalator instead of stairs, give the blood a reason to stagnate and form clots.
- Insufficient fluid intake. The quality of blood directly depends on what a person eats. With insufficient fluid intake, the blood becomes thick, which means it cannot fully perform its functions and puts a greater strain on the heart. It is easy to pump liquid blood through the system, but thick blood is much more difficult.
- Taking medications that affect the hematopoietic system. In medical practice, drugs are often used to treat certain diseases, one of the side effects of which is blood thickening. Therefore, such medications must be taken simultaneously with anticoagulants that prevent the formation of blood clots.
You can protect yourself from blood clots by regularly exposing your body to physical activity, drinking enough fluids, and including more plant-based foods rich in fiber in your diet.
The process of blood clot formation in the circulatory system
Magnetic resonance imaging is one of the most effective methods for diagnosing blood clot problems. In the absence of pathologies, after the formation of a blood clot, it gradually dissolves, and if there are problems, resorption does not occur. On the contrary, there is a layering of cells and the clot becomes denser, can break away from the vessel wall and move through the blood. This provokes vascular blockages, venous thrombosis, and pulmonary embolism. A detached blood clot causes cardiac arrest and cerebral hemorrhage.
The main causes of blood flow disorders
Problems can be caused by both congenital pathologies and external, acquired factors, the main ones include:
- mechanical damage to blood vessels and surgical intervention;
- metabolic disorders and obesity;
- contraceptives and hormonal drugs;
- advanced age;
- varicose veins and endocrine disorders;
- malignant tumors;
- inactive lifestyle.
These are all high-risk factors that require preventive diagnostics. MRI of brain vessels will help identify problems at an early stage, prescribe the correct course of treatment and avoid complications.
Additional options for improving the accuracy of magnetic resonance imaging of the circulatory system
Magnetic resonance imaging is not the only method of examining the circulatory system, although it is the most accessible; it is not inferior in accuracy to CT angiography. To improve diagnostic accuracy, additional tools are used. A contrast solution (gadolinium salts) is injected into the vessel, it stops at the site of thrombus formation, and the problem area is displayed on the screen. Also, a specialist can visualize a wall defect when the channel is not fully filled.
How do blood clots occur?
If a blood clot has formed on the wall of an artery, its appearance can be described in the following stages:
- Some process damages the artery wall.
- The body notices the violation and begins to build protection against blood loss, forming a large number of special blood cells - platelets, which, attaching to the damaged area, form a kind of patch.
- In case of coagulation disorders or changes in the hematopoietic system, platelet formation does not stop on time and continues longer than expected. This causes too much growth to form on the wall. Or platelets, which are in small quantities in the blood, floating past in the bloodstream, stick to the resulting accumulation.
The causes of damage to the walls of blood vessels can be:
- mechanical disruption of the structure due to injury;
- infectious lesion;
- high levels of glucose molecules in the blood;
- immune system dysfunction.
If there are no factors that contribute to the formation of blood clots, any injury or other damage will not lead to a large accumulation of blood cells. Under the layer of platelets, the artery wall will heal and recover, and the crust will resolve over time.
There are several stages of thrombus formation:
- disruption of the structure of the inner surface of the artery;
- activation of blood clotting factors;
- platelet adhesion at the site of injury;
- the appearance of substances that trigger a chain of reactions that form fibrin threads, which contribute to thrombus formation;
- a kind of network of fibrin threads is formed, into which blood cells enter, creating a large clot;
- Over time, the clot thickens, forming a thrombus.
When a blood clot breaks off under the influence of any factors, it begins to move through the bloodstream. Once it hits the nearest bottleneck, the blood flow will be blocked. If a similar situation happens outside a medical facility, it is impossible to save the person.
Does MRI show blood clots?
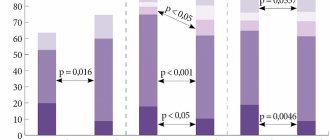
Magnetic resonance imaging is an informative type of diagnosis of vascular pathologies. Thrombi are determined less accurately on MRI than with CT angiography, based on indirect signs. For better visualization during magnetic resonance scanning, a contrast solution may be used. The drug is injected into the lumen of the vessel; at the site of occlusion, the gadolinium salts stop, “resting” against the thrombus due to the lack of blood flow in this area, or a parietal defect in the filling of the bed is visualized. However, both options, especially the second, can be caused by more than just the formation of a clot.
Thrombosis of the left sigmoid sinus on MR angiography (left image) with no visualization of the venous bed. In the native image (right picture) the pathology is not visible
MRI allows you to:
- determine the presence and location of a blood clot;
- clarify the size, quality of attachment to the vascular wall;
- identify emboli as they move through the bloodstream;
- determine the degree of patency of the vessel.
With thrombophlebitis, a scan shows signs of inflammation of the venous wall (thickening, stratification, changes in structure, etc.).
MRI visualizes the condition of the surrounding soft tissues, helping to determine the cause of blood flow disturbances (compression of a vessel by tumor masses, etc.). Diagnosis of thrombosis using magnetic resonance imaging makes it possible to clarify the consequences of this pathological phenomenon and visualize foci of ischemia and collaterals in the study area.
Control MRIs are carried out to determine the effectiveness of the treatment aimed at restoring the hemostatic system.
MRI shows small blood clots, clots located in deep veins, vessels of the lower extremities, brain, and internal organs. This type of instrumental research provides a three-dimensional image, visualizing the state of a section of the circulatory system and interaction with surrounding tissues.
Thrombosis factors
An increased risk of blood clots is caused by:
- Genetic inheritance to predisposition.
- Diseases that force you to limit physical activity, for example, bed rest.
- High degree of blood clotting.
- Arrhythmia, cardiomyopathy and other diseases that disrupt the strength and rhythm of blood flow throughout the system.
- Varicose veins.
- Liver dysfunction.
- Alcoholism.
- Smoking.
- High body mass index.
- Age-related changes in hormone levels in both men and women.
Some of these factors cannot be influenced, for example, genetic predisposition. However, you can protect yourself from the serious consequences of blood clots by maintaining an active and healthy lifestyle.
Magnetic resonance imaging (MRI) in St. Petersburg
Venous sinus thrombosis is one of the causes of stroke - stroke, especially in children and adolescents. The anatomy of the venous drainage from the brain is presented below. The main highways are the venous sinuses, the main ones being the superior and inferior sagittal, into which the superficial cortical veins flow (Labbe and Trolara) and the vein of Galen, which collects blood from the deep veins of the brain. Ultimately, all sinuses are collected through the drain into the transverse and sigmoid sinuses and leave the cranial cavities through the jugular veins.
Venous sinus thrombosis is caused by infection or coagulopathy. Contraceptive use and pregnancy are considered risk factors. You can read about infectious diseases of the brain on the page of our other website
In newborns, venous sinus thrombosis can be caused by dehydration.
With thrombosis of the venous sinus, there is an acute onset with headaches, seizures and even coma. Clinical signs are nonspecific, so radiodiagnosis plays a leading role in making a diagnosis.
On non-contrast images, blood clots in the thrombosed sinus may be visible (“delta” - symptom), increased density from the sinus (“cord” symptom). With contrast, on the contrary, there is a lack of filling of the sinus in a limited area (“reverse delta” symptom) and a lack of filling of the sinus with contrast.
| direct “delta” sign. CT, enlarged area of interest | CT with contrast. “reverse” delta sign. |
CT. Labbe vein thrombosis.
CT. Venous infarction.
MRI of the brain. T2-dependent MRI. Bilateral venous infarction.
MRI of the brain. Axial MRI type DWI. Bilateral venous infarction of the visual tuberosities.
A simple way to confirm venous sinus thrombosis is CT venography. The delay from the administration of the contrast agent should be at least 45-50 ms to avoid entering the arterial phase. The ideal delay is just over 1 minute. On CT, it is important not to confuse thrombosis with arachnoid granulations, which can grow into the venous sinus. A false “Delta sign” is not uncommon, therefore, only in combination with a filling defect during contrast can one speak with confidence about thrombosis. Sometimes a subdural hematoma or hyperdense empyema resembles increased density in the sinus, however, the spread will be more extensive.
MRI venography can be performed using 2D TOF, phase contrast (PC), or any of them under contrast conditions. The lack of vessel visualization is not always associated with thrombosis, but may reflect the specific structure of the venous system.
MRI and MRA of the brain. Thrombosis of the left cavernous sinus.
MR venography. Thrombosis of the left transverse sinus.
MRI of the brain clearly shows the consequences of thrombosis of the venous sinuses and cortical veins - venous infarctions. With MRI in St. Petersburg, we see (both in a high field and on an open MRI) that they differ in that they are not associated with the arterial circulation and contain a hemorrhagic component. Venous sinus thrombosis as an emergency condition during MRI of St. Petersburg should be diagnosed in a specialized hospital.
Leave feedback.
MRI in St. Petersburg USA
Arterial thrombosis - symptoms and treatment
Arterial thrombosis is a sudden, acute cessation of arterial blood flow caused by a thrombus blocking a blood vessel. Thrombus (from ancient Greek - lump, clot) is an intravital blood clot that forms during diseases or injuries. Normally, the circulatory system does not contain blood clots. Their appearance in the vessel threatens the patient’s life.
Arteries are blood vessels that carry oxygenated blood from the heart to the limbs, organs and tissues. Arterial thrombosis leads to a sudden cessation or deterioration of arterial blood flow in a limb or organ with a potential threat to its viability [1].
Arterial thrombosis in 40% of cases causes acute limb ischemia (lack of blood supply), and in 37% - embolism [2][3]. Embolism (from Greek - invasion) is the separation of a blood clot from the site of its initial formation, or the transfer of a pathological substrate with the bloodstream along the vascular bed with subsequent blockage of an arterial vessel. The pathological substrate can be solid, liquid or gaseous formations: drops of fat, gas or air bubbles, masses from a “burst” cholesterol plaque, pus, etc.
Arterial thrombosis and embolism cannot be considered independent diseases. They always arise as a consequence of other pathological conditions.
The causes of a blood clot in the lumen of a vessel are described by the German scientist Rudolf Virchow. They are united in the well-known triad:
- Damage to the vascular wall.
- Slowing blood flow.
- Violation of blood composition.
A thrombus is formed under the influence of all three factors with dominance of one of them.
Damage to the vascular wall is caused by:
- injuries - mechanical, thermal, electrical, etc.;
- inflammatory diseases of the arteries - arteritis, obliterating atherosclerosis with the development of atherothrombosis;
- severe infectious diseases - typhus, influenza, sepsis.
Slow blood flow occurs in the following cases:
- extravasal compression - compression of a vessel from the outside by a tumor, effusion of blood, an additional cervical rib, a bone fragment during a fracture, mechanical pressure during accidents, etc.;
- aneurysms (dilation of blood vessels);
- arterial spasms;
- acute circulatory failure;
- prolonged immobilization of limbs;
- oncological diseases.
to disturbances in blood composition [11]:
- blood diseases - leukemia, erythrocytosis, polycythemia;
- significant dehydration of the body;
- hereditary or acquired thrombophilia (pathological thrombus formation);
- systemic atherosclerosis;
- diabetes;
- hypertonic disease;
- malignant neoplasms;
- endotoxemia (accumulation of toxic breakdown products and bacterial activity in the blood and tissues);
- states of shock;
- taking medications - glucocorticosteroids, estrogens and gestagens (hormone replacement therapy and combined oral contraceptives), hemostatic agents, antifibrinolytic agents.
Emboli can be caused by heart disease or other causes.
Cardiac causes of embolism:
- cardiac ischemia;
- myocardial infarction;
- post-infarction cardiosclerosis;
- post-infarction aneurysms of the left ventricle;
- rheumatic heart defects;
- septic bacterial endocarditis;
- heart tumors (myxomas).
In these cases, a blood clot forms in the cavities of the heart. Then, under the influence of a hypertensive crisis, changes in heart rhythm and other reasons, its defragmentation occurs. The thrombus rushes with the blood flow, blocks a section of the arterial bed of a smaller diameter or a fork in the area of the division of the vessel.
Noncardiac causes:
- aortic aneurysm;
- ulcerated arterial plaques;
- pneumonia;
- lung tumor.
In rare cases, paradoxical embolism is possible - migration of a blood clot from the venous system through the right side of the heart to the left. This occurs with congenital heart disease and embolism with foreign objects (for example, a bullet or shot) [4].
The incidence of acute limb ischemia is one case per 6000 people annually [12]. With age, the incidence increases sharply. In the vast majority of cases, the pathology affects people over 60 years of age [8]. Ischemia, which occurs as a complication of thrombosis, more often affects men than women.
Smoking, an inactive lifestyle and poor nutrition lead to the development of atherosclerosis, hypertension and diabetes. At the same time, the risk of developing arterial thrombosis also increases.
The individual risk of vascular pathology includes:
- age younger than 50 years in the presence of diabetes mellitus and one of the risk factors for atherosclerosis: smoking, dyslipidemia (impaired lipid ratio in the blood serum), hypertension, hyperhomocysteinemia (increased level of the amino acid homocysteine in the blood);
- age 50-69 years and presence of diabetes mellitus or smoking;
- age 70 years and older [8].