Today, bacterial meningitis is a rare disease that can be diagnosed anywhere in the world. Some peoples have a genetic predisposition to this pathology, but in each age group the disease can develop for many reasons. This type of meningitis is transmitted by airborne droplets; it is especially easy to become infected when you are in the same room with a sick person. This disease has its own characteristics, symptoms and treatment methods, which differ from other forms of meningitis.
Characteristics and description of the problem
You may be interested in: Sperm aggregation: what does it mean, causes and treatment, consequences of pathology
Bacterial meningitis is an infectious disease of the brain and spinal cord, which is provoked by bacteria of the streptococcus group. Pathology contributes to the development of the inflammatory process in the membranes of the central nervous system. The prevalence of meningitis is insignificant, but it is easily transmitted from an infected person to a healthy person, which can cause an epidemic among the population. The main changes are observed in the soft and arachnoid membranes of the brain; often the gray matter is also involved in the pathological process.
You may be interested in: “Vitaprost Forte”: instructions for use, reviews
In medicine, bacterial meningitis in adults and children is divided into the following types:
- streptococcal;
- staphylococcal;
- pneumococcal;
- meningococcal;
- uncertain.
The disease is rapidly progressive and therefore requires immediate treatment. In the absence of therapy, the risk of complications and even death increases, this is important in childhood and old age, as well as in cases of reduced human immunity.
Infection of the meninges develops due to bacteria entering them. This happens as a result of the body’s reactions to pathogenic microorganisms. In the human body, activation of many physiologically active substances and leukocytes occurs in combination with endothelial damage. All this causes cerebral edema, increases intracranial pressure and reduces blood flow in the brain.
Results and discussion
The etiological structure of BM in the sample of patients we examined is presented in Table. 1.
Table 1. Etiological structure of BM in the examined patients (n=55)
As can be seen from table. 1, more than half of the examined patients suffered from generalized meningococcal infection, which confirms its leading role in the occurrence of BM in children.
In our study, 41 (74.5%) patients were found to have a burdened premorbid background: perinatal damage to the central nervous system - in 14 (34%), frequent acute respiratory viral infections - in 13 (32%), anemia - in 7 (17%), persistent herpesvirus infection - in 7 (17%), as well as their combination in different combinations.
In patients with concomitant somatic and/or neurological pathology, BM was significantly more severe, which is confirmed by the results of statistical analysis of clinical data ( p
<0,05).
Neurological complications of BM
One of the most common neurological complications is cerebral edema. In 11 (20%) patients in the acute period of BM, signs of cerebral edema were detected, which arose on the 2-3rd day of the disease, with progressive impairment of consciousness, motor restlessness, arterial hypertension, tachycardia, and convulsions.
With cerebral edema on NSG, a diffuse increase in the echogenicity of the brain parenchyma and sulci was found in the examined patients; their expansion was similar to the observations of other authors [4]. CT/MRI usually revealed a decrease in the density of brain matter and impaired differentiation of white and gray matter.
It should be noted that the effects of osmotic diuretics in traditionally used dosages in BM are significantly lower than in the treatment of traumatic and ischemic cerebral edema. Our clinic has successful experience in conducting infusion therapy with mannitol 4 times a day (given its fairly rapid elimination); in this case, it is necessary to control the osmolarity of the blood serum. It is advisable to administer the initial dose of dexamethasone before antibiotic therapy is prescribed; the regimens used are considered equally effective (dexamethasone 0.4 mg/kg 2 times a day or 0.15 mg/kg 4 times a day, lasting up to 4 days) [5]. Currently, there are no confirmed randomized studies on the direct effect of corticosteroids on cerebral edema [6–8].
In the acute period of BM, 5 (9%) patients had neurological paroxysmal symptoms, which were represented by generalized (clonic) or complex focal (motor) epileptic seizures with secondary generalization: in 2 (3.6%) patients with generalized meningococcal infection; in 2 (3.6%) - with pneumococcal meningitis and in 1 - with hemophilic meningitis. Epileptic seizures occurred on the 2-4th day from the onset of the disease. The appearance of generalized seizures at the onset of MD should be considered a manifestation of general cerebral disorders resulting from acute metabolic encephalopathy; the presence of focal seizures suggests focal damage to the brain substance.
In our experience, epileptic seizures are effectively controlled with standard intravenous antiepileptic drugs; their prevention in the acute period of BM is carried out by oral administration of barbiturates (gluferal) at a rate of 3-5 mg/kg per day. For children with a relatively mild course of MD, the absence of repeated epileptic seizures and epileptic changes on the electroencephalogram (EEG), anticonvulsant therapy should be discontinued immediately after discharge from the hospital.
In our study, a relatively common complication of MD was subdural empyema. One patient with pneumococcal meningitis developed unilateral subdural empyema in combination with an abscess of the frontotemporal region, and 2 (3.6%) patients with meningococcal infection developed unilateral subdural effusion. Subdural empyema is a source of infection and contributes to the transition of the acute stage of BM to chronic or recurrent. Subdural empyema, as well as a brain abscess, suggests that the patient has primary foci of ENT infection. 7 (12.7%) patients with BM had a history of ethmoiditis and mastoiditis. With a prolonged course of BM (more often in infants), the formation of abscesses is possible even without a primary source of infection. Subdural empyema can reach large sizes and, compressing the brain, demonstrate the clinical picture of a growing subdural hematoma (progressive impairment of consciousness from depression to coma, repeated vomiting, bulging of the large fontanelle in infants, epileptic focal seizures, persistent fever). CSF analysis can differentiate subdural empyema from subdural effusion. In subdural empyema, the cellular composition of the CSF contains predominantly neutrophils.
Subdural effusion in the acute period of BM is common, but its clinical manifestations are rare - usually these are signs of increased intracranial pressure. In the majority of the patients we examined (5.5%), subdural effusion on NSG, CT and MRI revealed an accumulation of fluid compressing the substance of the brain, so the management of such patients should include the possibility of consulting a neurosurgeon.
Treatment of subdural empyema and brain abscess is surgical; prevention consists of sanitizing foci of primary ENT infection. If the subdural effusion does not compress the cerebral structures, surgical intervention is not required.
Oculomotor disorders (strabismus, diplopia, ptosis) indicate involvement of the cranial nerve roots in the pathological process. In our work, oculomotor disorders were transient and after 3-7 days from the onset of the disease, the movements of the eyeballs were completely restored: in 2 (3.6%) patients with pneumococcal meningitis and in 1 with hemophilic meningitis.
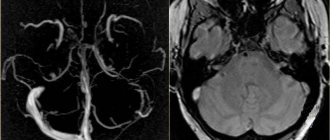
Frequent vascular complications of BM include venous thrombosis [9–10]. In our study, cavernous sinus thrombosis was detected in 1 patient with hemophilic meningitis. Damage to the oculomotor nerve speaks in favor of it. Thrombosis of the cavernous sinus is of great diagnostic importance in terms of objectifying a possible focus of primary infection (ethmoiditis). With ethmoiditis on MRI, swelling of the mucous membrane of the paranasal sinuses or mastoid cells gives the same signal change as purulent inflammation, therefore in these cases it is better to verify the source of the primary infection using CT or radiography. MR venography can detect thrombosis of the venous sinus and cortical veins.
Treatment of venous thrombosis includes the prescription of anticoagulants and moderate dehydration in age-related dosages. Medicinal sedation of the patient is of great importance, since increased intracranial pressure can lead to rupture of the veins in the cranial cavity. Their prevention should include the administration of anticoagulants and fresh frozen plasma.
In table Figure 2 presents neurological complications of MD in children of different age groups depending on the type of pathogen. In 26 (47.3%) patients with MD, certain neurological complications were found, among which, in the acute period of the disease, cerebral edema was detected in 11 (20%) patients.
Table 2. Neurological complications of MD in examined children depending on the type of pathogen (n=55) Note. A number of patients had more than one complication, and therefore their sum does not correspond to the total number of patients.
Thus, the study confirmed that children who have had BM still have a fairly high incidence of neurological complications that have serious consequences for the life and development of the child.
BM outcomes.
19 (34.5%) patients had a favorable BM outcome (recovery), among them 17 (89.5%) children suffered generalized meningococcal infection and 2 (10.5%) had hemophilic meningitis. 25 (45.5%) patients had asthenoneurotic syndrome (a relatively favorable outcome of BM), among them 15 (60%) patients had generalized meningococcal infection, 5 (20%) had hemophilic meningitis, and 5 (20%) had pneumococcal meningitis. Asthenoneurotic syndrome was characterized by chronic or episodic tension headaches, sleep disturbances, emotional disorders, and behavioral disorders. Complaints of headache, as a rule, appeared in the 2-3rd week from the onset of BM, intensifying with mental and/or physical stress. In young children, almost all phases of sleep were disrupted, night fears and sleep talk appeared. In older children, obsessive movements and behavioral disorders were observed.
In 2 (3.6%) patients with meningococcal infection and 1 with pneumococcal meningitis, symptomatic focal epilepsy was diagnosed, requiring long-term antiepileptic therapy (within 2 years from the last attack under EEG control).
When the auditory nerve is involved in the pathological process, a possible outcome of MD is sensorineural hearing loss, found in 2 (3.6%) patients with hemophilic meningitis and in 1 with pneumococcal meningitis. Similar data were obtained in studies by M.N. Sorokina et al. [11]: 2-3% of patients with HD have sensorineural hearing loss and hemiparesis.
According to various authors, there is no selectivity in the nature of the infectious pathogen for the occurrence of sensorineural hearing loss (streptococcus, pneumococcus, meningococcus, Haemophilus influenzae, etc.), and among the predisposing factors, a severe course of BM is usually noted [12-14]. The structures of the inner ear are most often affected [15], in some cases in combination with damage to the vestibular part of the nerve. Hearing may decrease in the first days of MD, but if the course of the disease is favorable, hearing is restored in the first 2 weeks of the disease. N.V. Skripchenko [16] identified a group of patients at risk for the development of sensorineural hearing loss, which includes patients who have had pneumococcal and hemophilic meningitis, manifesting with ARVI or pathology of the upper respiratory tract (otitis). In the same work, some features of the course of MD were identified: the involvement of cranial nerves in the acute period of the disease and an increase in protein levels in the CSF of more than 2.2 g/l with a decrease in glucose levels of less than 2.1 mmol/l.
In cases of severe sensorineural hearing loss, cochlear implantation is advisable. For vestibular dizziness and instability, a short course of symptomatic treatment (histamine analogues, antipsychotics, barbiturates, benzodiazepines, anticholinergic drugs in age-appropriate dosages) and vestibular rehabilitation are recommended.
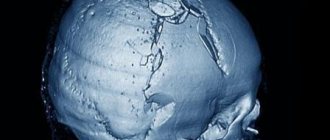
In 2 (5.4%) patients with generalized meningococcal infection, the unfavorable outcome was aresorptive hydrocephalus (in 1 case, requiring shunt surgery), caused by a decrease in the absorption capacity of pachyonic granulations by the inflamed arachnoid membrane of the brain. Clinically, hydrocephalus is manifested by an increase in the size of the head, bulging and tension of the large fontanel, divergence of the sutures of the skull, expansion of the cerebrospinal fluid spaces; in older children - severe headache, the appearance of congestion in the fundus. Hydrocephalus is verified by NSG, CT and MRI in the form of expansion of the ventricular system of the brain due to excessive accumulation of CSF.
Conservative treatment of hydrocephalus is aimed primarily at eliminating the bacterial pathogen; Diacarb is also prescribed (before sanitation of the CSF) at a rate of 50-100 mg/kg per day in infants or up to 750 mg per day in older children. Drainage operations are indicated when hydrocephalus and clinical signs of increased intracranial pressure persist or increase despite conservative treatment. Prevention of hydrocephalus involves prescribing timely and adequate antibacterial therapy.
In 2 (3.6%) patients with generalized meningococcal infection and 1 patient with pneumococcal meningitis, motor disorders (spastic tetra-, hemiparesis) were detected. In 1 patient who suffered pneumococcal meningitis, encephalopathy of mixed (infectious-toxic) origin was detected (see clinical case). Outcomes B.M. in the examined children and their differentiation depending on the type of pathogen are presented in Table. 3.
Table 3. Outcomes of B.M. in the examined children, depending on the type of pathogen Note. In a number of patients, different clinical outcomes of BM were identified, and therefore their sum does not correspond to the total number of patients.
Epidemiology
In developed countries, the disease occurs in 80% of cases in people under sixteen years of age. Males are most often affected. In 10% of cases, this pathology leads to death, and another 10% of infected people develop permanent neurological disorders. An increase in incidence is observed in winter, primarily due to climatic conditions (temperature changes, increased humidity), as well as prolonged stay in enclosed spaces. Every ten years there is an increase in the incidence rate.
You may be interested in: Defecation - what is it?
How bacterial meningitis is transmitted is described above; it is widespread in all countries of the world, especially in African countries, where the pathology occurs in 500 cases per 100,000 people. For a long time, this pathology was considered childhood, since, according to statistics, it was previously observed in children aged 12-18 months. After the introduction of vaccination, the disease began to be frequently observed in the adult population. Today, pathology is diagnosed in 33% of cases among all infectious diseases of the central nervous system.
Causes of the disease
Purulent bacterial meningitis can be caused by various bacteria (see above), including Salmonella, Klebsiella and Pseudomonas aeruginosa. These microorganisms live in the environment and in the human body. When exposed to negative factors, they begin to rapidly multiply and infect brain cells.
There are many reasons why the disease can affect the body of each person:
- head injuries;
- decreased immunity;
- transfer of severe inflammatory diseases;
- genetic predisposition of some peoples;
- infection from a carrier.
Like any infectious disease, bacterial meningitis is transmitted by food or airborne droplets, as well as by direct contact with a carrier of the infection: shaking hands, kissing, sneezing, or using shared household items. Therefore, doctors recommend strictly observing the rules of personal hygiene.
Current problems in the diagnosis and treatment of bacterial meningitis
Bacterial purulent meningitis (BPM) occupies one of the leading places in the structure of neuroinfections; their incidence is in the range of 5–10 per 100 thousand population. Among the causes of mortality from infectious diseases, they occupy tenth place and second after AIDS in the structure of mortality in infectious diseases hospitals. Despite the availability of a large selection of antibacterial drugs and pathogenetic therapy, mortality has not decreased over the past 40–50 years and remains within the following limits: 15–50% for pneumococcal meningitis, 5–15% for meningococcal infection, 3–20% for with hemophilic meningitis. Clinically, HMS are characterized by such syndromes as febrile intoxication (hyperthermia, myasthenia, myalgia, anorexia, toxic damage to the cardiovascular system (CVS), central nervous system (CNS) and autonomic nervous system, etc.) and meningeal (diffuse headache pain accompanied by nausea and vomiting, skin hyperesthesia, stiffness of the neck muscles, positive Kernig and Brudzinski symptoms), as well as characteristic changes in the cerebrospinal fluid (CSF) (a sharp increase in cerebrospinal fluid pressure, changes in transparency, increased levels of protein and lactate, high neutrophil pleocytosis, decreased glucose levels). When the inflammatory process spreads to the substance of the brain and the development of edema-swelling of the brain, a general cerebral syndrome (impaired consciousness and psyche, generalized convulsions) and focal neurological symptoms (paresis of cranial nerves, limbs, pelvic disorders, cerebellar symptoms, pathological reflexes, etc.) join.
Over 5 years, 2148 patients with HD were observed at ICH No. 2 in Moscow, of which 776 were in the ICU (37.2%). Laboratory tests (bacteriologically, latex agglutination reaction - RLA) deciphered the etiology of meningitis in 38% of patients. In 60% of patients with meningococcal infection, the diagnosis is established clinically. Among laboratory-confirmed cases of the disease, meningococcal meningitis (MM) accounted for 64%, pneumococcal meningitis (PM) - 21.3%, meningitis caused by Haemophilus influenzae type B (HiB-meningitis) - 9.3%, however, in the etiological structure of children HiB- meningitis is in second place after meningococcal. 5.3% were meningitis of staphylococcal, streptococcal, listeria, klebsiella, and escherichiosis etiology. Over the past 3 years, according to our observations, there has been a tendency towards a more severe course of the disease. Thus, in 2004, 37.8% of patients were hospitalized in the ICU, in 2005 - 39.1%, in 2006 - 49.9%, i.e. half of all patients with HD.
The causes of severe condition and mortality of patients admitted to the ICU in 86.1% were cerebral edema (CE), CE in combination with infectious toxic shock (ITS), and meningoencephalitis. Mortality fluctuated significantly from year to year. Thus, in 2005 it was 5.2%, and in 2006 it increased to 13.5%. It increased significantly in meningococcal, hemophilic meningitis and meningitis of unknown etiology, amounting to 3.8%, 0%, 5.9% in 2005, respectively, and in 2006 - 9.7%, 15.7%, 13 .6% (Table 1).
The increase in mortality in hemophilic meningitis over the past year is due to the development of ITS in three patients. For 162 patients with hemophilic meningitis observed over the past 20 years, the mortality rate was 3.7%.
The analysis of diagnostics and treatment results for HBM shows that the most pressing practical problems at the present stage are:
- early clinical diagnosis at the prehospital stage and transportation of patients to specialized departments;
- correct assessment of the severity of the patient’s condition followed by adequate therapy at the prehospital level;
- early diagnosis and laboratory confirmation of diagnosis in the hospital;
- adequate etiotropic therapy at all stages;
- early assessment of the effectiveness of etiotropic therapy;
- qualified intensive care and resuscitation of seriously ill patients in ICUs of specialized hospitals.
In Moscow, despite postgraduate training, lectures and other educational events, a significant proportion of patients are hospitalized at a late stage; often, after 2-3 visits, patients are sent to non-core hospitals. Thus, with HiB meningitis, the average length of hospitalization is 3.2 days; patients were hospitalized in five different hospitals, and only 54% - in ICU No. 2. However, the mortality rate in ICU No. 2 is 3.7%, and in non-core hospitals - 23.5%, i.e. more than 6 times higher.
It has been established that patients with HD are admitted to the ICU late, on average 3.5 ± 0.2 days of illness, while in the boxed department (BO) almost in the first 2 days (1.6 ± 0.3 days disease) (p < 0.001). In 38.3% of cases, late admission was due to erroneous diagnoses when patients initially sought help. Moreover, in 2005 the error rate was 27.3%, in 2006 - 45.8%, i.e. it doubled.
According to accompanying documents for 2005–2006. It was found that the most common erroneous diagnoses in the typical clinical picture of purulent meningitis were acute cerebrovascular accident (ACVA), acute respiratory viral infection (ARVI), pyelonephritis, pneumonia, alcoholic delirium, food poisoning, cholecystitis, acute overdose of psychotropic drugs, otitis media, acute appendicitis, acute urinary retention. Erroneous diagnosis led to the fact that patients were hospitalized in non-core hospitals (23.4%), where on average they spent 1.8 days before deciphering the diagnosis and, accordingly, did not receive the necessary qualified care. There were also cases of overdiagnosis, when patients with suspected meningitis were hospitalized in the ICU (9.8%) and BO (16.6%) and were diagnosed with stroke, brain tumor, poisoning with psychotropic drugs, secondary otogenic meningitis, epilepsy, ARVI, osteochondrosis . Overdiagnosis is also a negative factor for patients with HD, since due to the severity of the condition, there was a problem of transfer to a specialized hospital and provision of specialized care.
In a hospital, the outcome of the disease largely depends on the speed of diagnosis of HDM and its etiological decoding, since in the absence of additional symptoms, HDM of various etiologies are clinically indistinguishable.
Based on clinical and laboratory data, an etiological diagnosis was established in 74% of patients (including only 48% using the bacteriological method and RLA). At the same time, I would like to emphasize the role of blood culture. Blood cultures were obtained from 58% of patients with HiB meningitis, 27% with PM, and 16% with the generalized form of meningococcal infection (MI). The results of bacteriological research can be improved by improving research techniques (sampling of material, transportation, quality of media). However, a dramatic increase in the frequency of deciphering the diagnosis is possible only through the introduction of the polymerase chain reaction (PCR) method. So, back in 1998–2000. the use of PCR made it possible to establish the etiology of HD in more than 80% of patients.
When using routine diagnostic methods, the greatest diagnostic difficulties are presented by patients with 2-3-digit neutrophilic or mixed pleocytosis of the CSF. This group may include patients with secondary HBM in sepsis, brain abscesses, primary HBM in the early stages of the disease or treated with antibiotics, patients with tuberculous meningitis, viral neuroinfections in the early stages, subarachnoid hemorrhages. The summarized differential criteria are presented in Table 2.
We attach significant diagnostic importance to the concentration of lactate in the CSF and blood and their ratio, which is based on the results of a dynamic examination of more than 200 patients.
The basic principles and standards of antimicrobial therapy are known. We use the following drugs for empirical therapy of HD: depending on age, we use ceftriaxone, cefotaxime, ampicillin. Depending on the pathogen isolated, etiotropic therapy is prescribed: for meningococcal meningitis - penicillin, ceftriaxone, cefotaxime, cefepime; for pneumococcal - penicillin, ceftriaxone, vancomycin, meropenem, ciprofloxacin; for HiB meningitis - ceftriaxone, cefotaxime, pefloxacin; for meningitis caused by enterobacteria - ceftriaxone, cefotaxime, pefloxacin, cefepime; for staphylococcal - vancomycin, rifampicin, oxacillin, meropenem, linezolid; for Pseudomonas aeruginosa - ceftazidime, ciprofloxacin, cefoperazone, cefepime; for listeria - vancomycin, ceftriaxone, ampicillin; for leptospirosis - penicillin, ampicillin, cefotaxime; for meningitis caused by bacteroids - metronidazole, Co-trimoxazole, meropenem; for meningitis caused by enterococci - ampicillin, amikacin, vancomycin, meropenem. In severe cases of HD, endolumbar administration of vancomycin and amikacin is used. The problem of pathogen resistance is becoming more and more urgent. In recent years, a tendency towards the emergence of resistant strains of pathogens to drugs used in the practice of treating meningitis has become more clearly evident. Thus, 4% of meningococcal and 3% pneumococcal strains were resistant to penicillin. Individual multidrug-resistant strains of meningococcus and pneumococcus are registered.
While there is a choice of drugs from 4–5 different groups, and the frequency of isolation of drugs resistant to individual drugs is no more than 5–6%, this problem can be solved by replacement, however, in the coming years, the problem of “aging” of antimicrobial drugs in relation to the treatment of BGM may become very acute, especially considering the desire of medical practitioners to widely use, often without sufficient justification, antibiotics, especially new ones. As a result, strains of meningitis pathogens appear that are resistant not only to penicillin and chloramphenicol, but also to fluoroquinolones and meropenem.
Another problem is the lack of effect when treated with drugs to which this pathogen strain is sensitive. We observed this phenomenon in different groups of patients with a frequency of 15 to 30%, which can be demonstrated by the example of HiB meningitis (Fig.).
| Drawing. Sensitivity of HiB to antibiotics, % |
The reasons are varied, including:
- insufficient passage of the drug through the blood-brain barrier (BBB);
- the presence of zones of bioinaccessibility of the pathogen;
- insufficient dose or low quality of the drug;
- discrepancy between data on the sensitivity of the pathogen in vitro and in vivo.
It should be noted that in different patients with the same doses of the drug, its concentration in the CSF varies tenfold. Insufficient passage of the antibiotic may be due to the characteristics of the pathological process and insufficient cerebrospinal fluid production. Thus, upon admission, almost 20% of patients with BGM experience liquor hypotension. As the inflammatory process subsides, the permeability of the BBB decreases, the process of CSF resorption prevails over liquor production, which is clearly reflected in the pharmacokinetics of the drug.
Diuretics and corticosteroids have a significant effect on this process. The presence of zones of bioinaccessibility is evidenced by frequent cultures of the pathogen, especially pneumococcus, from cadaveric material in those who died after long-term use of antibiotics. These zones are created in clots of exudate, encephalitic foci, foci of softening of brain tissue, hematomas, cells of the subarachnoid space, and in the ventricles of the brain with ventriculitis. In these cases, it is advisable (if the pathogen is sensitive) to use super-massive doses of penicillin, the use of intracarotid and endolumbar methods of administering antibiotics. The use of low-quality drugs, in particular Indian-made ceftriaxone, is often accompanied by an exacerbation of the process, and sometimes is completely ineffective.
Unfortunately, in recent years, the peculiarities of the pharmacokinetics of antimicrobial drugs in ICU conditions during intensive care have not been studied and, accordingly, there are no recommendations on the correction of antimicrobial and pathogenetic therapy from these positions.
The study of the sensitivity of the pathogen is an important criterion determining the choice of drug, but only in the case of a methodologically correct study. In addition, there is evidence that bacteria dramatically change their activity when living conditions change. It is possible that these changes may affect the results of determining the sensitivity of the pathogen, but the issue needs to be studied. Thus, the problem of increasing the effectiveness of etiotropic therapy for HD requires fundamental research.
It is difficult to assess the effectiveness of antibacterial therapy in the early stages, especially in patients with severe HD, which often leads to unjustified replacement of the antibiotic. So, for example, with HiB meningitis, replacement was made in 68% of the patients we observed, but justified - only in 28%.
When deciding to change the drug, you should keep in mind that:
- in severe patients, assessment of the effectiveness of treatment is possible with MM no earlier than 2 days, with HiB meningitis - no earlier than 3 days, with PM - no earlier than 3-5 days;
- clinical indicators are not informative enough, since improvement of the condition may be associated with the temporary effect of dehydration and detoxification therapy, and deterioration of the condition, including an increase in cerebral, meningeal and focal symptoms, is also possible with effective antibacterial therapy due to cerebral and extracerebral complications (increase in ONGM, intracranial hematomas , epiduritis, herpetic infection, pneumonia, etc.);
- after 1–2 days from the start of treatment, even with adequate antimicrobial therapy, it is possible to inoculate the pathogen from the CSF, and pleocytosis may increase. At the same time, with ineffective therapy, a decrease in pleocytosis is possible;
- According to our data, the earliest and most informative criteria for the effectiveness of etiotropic therapy are: cellular composition of the CSF, concentration of protein and glucose, lactate, pH, partial pressure of oxygen pO2 in the cerebrospinal fluid (Table 3).
The totality of these data in most cases allows, within 2–3 days, to realistically assess the effectiveness of treatment and make an informed decision on the duration of treatment with the same drug or on its replacement. However, it should be noted that with PM, positive dynamics of these indicators can be detected 1–3 days later.
The next aspect is the timely decision to discontinue the antibiotic. According to our data, the duration of antibiotic therapy for patients with HD increases by an average of 1 day over 8–10 years. So, in 1960–1970. The duration of penicillin therapy was on average 7 days, after 2000 - 10 days. In some cases, especially when it is necessary to change drugs during treatment, prolongation of treatment is advisable, but there are typical situations when there are no indications for continuing antibiotic therapy.
- Prolonged fever with complete regression of neurological symptoms and sanitation of the CSF, in the absence of any purulent-septic complications (pneumonia, pyelitis, endocarditis, post-injection abscess, infected intravasal catheter).
- Prolonged fever is most often observed in patients with HiB meningitis and meningococcemia. In such patients, the cause of fever is most often infectious-allergic arthritis and myocarditis. In young children, the temperature may return to normal after stopping antibiotics. Non-steroidal anti-inflammatory drugs are effective.
- Long-term persistence of lymphocytic pleocytosis of CSF ranging from 100 to 200–300 cells/μl in the absence of neurological symptoms, normal levels of CSF glucose and lactate. According to our data, in these cases the main share (more than 90%) is made up of T-lymphocytes, mainly T-helper cells (CD4), and the immunoregulatory index increases sharply, reaching 4.8–5.5. At the same time, the content of immunoglobulins of various classes increases several times. Thus, the inflammation is aseptic in nature and is caused by a local reaction of the immune system.
Premature discontinuation of antibiotics is less common - usually in patients with PM and HiB meningitis with a satisfactory general condition, regression of neurological parameters, low pleocytosis in the range of 40–100 in 1 μl, with neutrophils remaining in the CSF of 20–30%, a decrease in glucose levels and an increase in lactate , which indicates continued activity of the pathogen. It is also necessary to take into account such indicators as a neurologically burdened premorbid background, the undulation of the course of meningitis, and slow sanitation of the CSF.
Premature withdrawal of antibiotics in these cases leads to an exacerbation of the disease within a few days.
The most important direction in reducing mortality is improving methods of intensive care and resuscitation. The result of treatment is largely determined by the qualifications of doctors and nursing staff, and compliance with the sanitary and hygienic regime in the department. Doctors who have two certificates - a resuscitator and an infectious disease specialist - must work in the ICU. A significant reduction in mortality can be achieved thanks to preventive intubation and early transfer of patients with ONGM syndrome to artificial ventilation (ALV), before the development of severe degrees of hypoxemia, development of optimal ventilator modes, development of indications for the use of loop and osmotic diuretics, corticosteroids.
Thus, improving the efficiency of the quality of medical care for patients with HD is a real prospect. It can be achieved by increasing the level of training of doctors in clinics, ambulances and non-core hospitals in neuroinfections, improving diagnostics in hospitals through the introduction of PCR, RLA, improving bacteriological diagnostics, determining sensitivity to antibacterial drugs using standardized methods, including among routine examination methods the determination of blood levels. lactate in the CSF and blood, the use of modern regimens for the use of antibacterial drugs, objective methods for assessing their effectiveness and determining on this basis indications for their replacement, optimizing the duration of the course of treatment, introducing into ICU practice preventive intubation of patients with severe HD and their early transfer to mechanical ventilation , improving methods of pathogenetic therapy.
Yu. Ya. Vengerov, Doctor of Medical Sciences, Professor M. V. Nagibina, Candidate of Medical Sciences, Associate Professor T. E. Migmanov, Candidate of Medical Sciences, Associate Professor R. N. Bykova V. B. Chentsov, Candidate of Medical Sciences G. V Kryuchkova T. Yu. Smirnova T. I. Svistunova, Candidate of Medical Sciences V. A. Myasnikov MGMSU, Clinical Hospital No. 2, Moscow
Risk group
But when an infection enters the body, meningitis does not always develop. For its occurrence, special conditions are necessary: a disorder of the immune system and a throughput reaction of the body. In the presence of these factors, harmful bacteria freely penetrate the circulatory system and move to the brain. Therefore, the risk group includes:
- persons with chronic diseases;
- people who abuse alcohol, nicotine, and drugs;
- HIV-infected;
- children under three years old.
Symptoms and signs of pathology
You may be interested in: The best child psychiatrist in Moscow: reviews
Bacterial meningitis usually does not show symptoms right away. The length of the incubation period depends on the age and health of the person, but it is usually fourteen days. After this, the disease begins to show the first signs, which are similar to those of other infectious diseases:
- increase in body temperature;
- severe headache, dizziness, fever;
- inflammation of the upper respiratory tract, nasopharyngitis;
- nausea accompanied by periodic vomiting;
- lack of appetite, diarrhea;
- hyperesthesia and increased muscle tone.
Diagnostics
Diagnosis of the disease presents certain difficulties in the initial stages of the disease (the only manifestations of which may be symptoms of ARVI), however, in the acute period, diagnosing the disease is quite simple. A neurological examination reveals symptoms of irritation of the meninges (Brudzinsky's, Kernig's, Guillain's and others symptoms). Lights and sounds make headaches worse. Children often develop hydrocephalic cry.
The basis of the instrumental diagnosis of bacterial meningitis is the collection of cerebrospinal fluid. The cerebrospinal fluid pressure is increased, the cerebrospinal fluid may come out in a tense stream. The liquid itself is cloudy and viscous. When analyzing cerebrospinal fluid, cellular-protein dissociation, predominantly of a neutrophilic nature, attracts attention. The number of cells can exceed 1000 per 1 µl. There is also a decrease in glucose and electrolyte levels. Sowing the cerebrospinal fluid on media reveals the bacterial nature of the disease; if necessary, an antibiotic sensitivity test is performed.
Specific signs
Specific signs of the disease include:
- Kerning's sign. In this case, a person is unable to raise his straight leg ninety degrees in a horizontal position.
- Brudzinski's sign. It is characterized by the inability to lean the head to the chest, raise the shoulders when pressing on the cheek, bend the legs when pressing on the pubic area, involuntary bending of the second leg when trying to bend the first.
In especially severe cases, the symptoms of bacterial meningitis in adults manifest themselves in the form of hemorrhagic exanthema, when spider veins or large areas of subcutaneous hemorrhages appear throughout the body. Then cerebral edema, convulsions and shortness of breath occur, the person develops coma and pulmonary edema.
In newborns, the disease manifests itself as tension in the fontanel and neurological symptoms. Often the pathology is complicated by meningoencephalitis or ependymatitis. In this case, severe drowsiness, paresis and paralysis, and hydrocephalus develop. In the absence of proper therapy, the disease develops very quickly, within one day. Therefore, when the first symptoms appear, you should immediately consult a doctor.
How to recognize meningitis?
Meningococcal infection is an extremely dangerous and potentially fatal bacterial infection, the most effective protection against which is vaccination. A hat does not protect against meningitis.
Meningitis can begin as a regular acute respiratory viral infection: with a runny nose, pain in the neck, fever, and it is extremely difficult to recognize a serious illness at this stage.
Young children are most vulnerable to meningitis, and you can get sick at any age.
Main symptoms of meningitis:
- Heat
- Severe headache, difficult to respond to NSAIDs
- Vomiting, often accompanying headache
- Photophobia, soundphobia
- Tension (stiffness) of the neck muscles
- Throwing the head back
- Confusion, lethargy, drowsiness
- Convulsions
- Tension, pulsation of the large fontanel (in children)
- Hemorrhagic rash (bright red spots with jagged edges)
If you notice any of these signs in yourself or your family members, contact your doctor immediately! Most often, the disease develops very quickly and there is a possibility of the child dying in the first hours of the disease!
Complications and consequences
The consequences of bacterial meningitis for human health are catastrophic. One of the most dangerous complications is cerebral edema, which provokes the development of coma, respiratory paralysis and death. Pathology can also cause disturbances in the psyche and central nervous system.
Often the consequences of bacterial meningitis in adults and children are as follows:
- hydrocephalus;
- pathologies of the kidneys and heart;
- hearing loss;
- vasculitis, causing paralysis of the cranial nerve;
- cerebral infarction, accompanied by focal seizures, which gradually develop into epilepsy;
- brain abscess.
After the disease, children often develop mental retardation, speech and memory impairment, and mental disorders. Apathy, passivity or, conversely, aggressiveness are often observed.
Diagnostic measures
A diagnosis of purulent bacterial meningitis can only be made with the results of all laboratory tests and a lumbar puncture, which is performed by inserting a needle into the spine to collect cerebrospinal fluid.
The following diagnostic methods are used in medicine:
- Collecting and studying anamnesis, studying the symptoms of pathology.
- Laboratory tests of blood and urine to determine the inflammatory process and damage to internal organs.
- Spinal puncture and examination of the obtained material.
- Culture of mucus from the nose for the presence of meningococcus or pneumococcus.
- PCR and ELISA.
- MRI to detect hydrocephalus, abscess.
- Blood test for acid-base balance.
The primary diagnosis is made on the basis of a meningeal complex of symptoms, signs of intoxication and inflammation syndrome in the cerebrospinal fluid. Based on the results of a comprehensive examination, a final diagnosis is made.
Material and methods
We examined 55 patients with MD aged from 2 months to 12 years (average age of patients - 3.5±0.36 years). The sample was dominated by boys (58%).
Patients were assessed for somatic status, neurological disorders and depth of consciousness disorder using the Glasgow Coma Scale (GCS).
All patients underwent bacteriological examination of mucus from the nasopharynx, microscopy of blood “in a thick drop”, blood culture for sterility, clinical and biochemical blood tests, serological examination of blood in paired sera - indirect hemagglutination reaction, latex agglutination reaction, immunological examination of blood serum and cerebrospinal fluid (CSF) with determination of the levels of interferon-α, β and γ, procalcitonin and neopterin by enzyme-linked immunosorbent assay (ELISA). In the laboratory of ontogenesis and correction of the interferonogenesis system of the Federal Research Center for Epidemiology and Microbiology named after. N.F. Gamaleya studied the metabolism of cytokines using ELISA.
At the Center for Molecular Diagnostics of the Research Institute of Epidemiology, a molecular genetic study of blood serum and CSF was carried out to amplify the genetic material of the microorganism using the polymerase chain reaction method.
To diagnose cerebral complications, neurosonography (NSG) was performed in the radiology department of Infectious Diseases Hospital No. 2, computed (X-ray) tomography of the brain (CT) - in the radiology department of the same hospital, magnetic resonance imaging of the brain (MRI) - in the department radiology diagnostics of the Children's City Clinical Hospital named after. BEHIND. Bashlyaeva.
Statistical data processing was carried out using R Studio and Excel. Pearson, Wilcoxon and Anderson-Darling χ2 tests were used. To control the group error probability, the Holm method was used. The confidence level was chosen to be 0.05.
Treatment of the disease
Treatment of bacterial meningitis is carried out in a hospital setting using intensive care. Broad-spectrum antibacterial drugs and quinolones are prescribed even before diagnostic results are obtained. Medicines are administered intravenously or by injection into the spinal cord canal. In this case, the patient must be constantly monitored, and in case of convulsions or seizures, he is provided with the necessary assistance. When seizures occur, anticonvulsants and drugs to reduce intracranial pressure are prescribed. Treatment of concomitant pathologies is also carried out jointly. The doctor prescribes antipyretic, painkillers and anti-inflammatory drugs.
Also, doctors must monitor the patient’s water-salt balance and carry out appropriate treatment measures in case of dehydration as a result of diarrhea and vomiting. Since bacterial meningitis often leads to the development of complications, it is necessary to monitor the condition of internal organs and control blood pressure.
To eliminate the symptoms of intoxication, detoxification therapy is carried out and diuretics are prescribed. But such measures are contraindicated in case of cerebral edema. To treat pathology, glucocorticosteroids are also used to eliminate the inflammatory process, which makes it possible to reduce the risk of death and the occurrence of long-term complications. If necessary, perform artificial ventilation.
Treatment of meningitis
Treatment is prescribed depending on the causative agent of meningitis.
Bacterial meningitis requires hospital treatment with intravenous antibiotics and glucocorticosteroid drugs, which reduce the risks of complications and help recovery.
For viral meningitis, antibiotics will be useless. Most often, the disease goes away on its own within a few weeks. With a mild form, bed rest is required, drinking should be observed, as well as taking painkillers.
For more severe forms of viral meningitis, symptomatic treatment and supportive care are prescribed. And if the cause of the disease is the herpes virus, then in this case the administration of antiviral drugs will be prescribed.
There are also cases when the cause of meningitis cannot be identified, then the doctor prescribes blind therapy, which includes both antibiotics and antiviral therapy. This continues until the exact cause is identified.
For fungal meningitis, antifungal drugs are prescribed, but since these drugs can have strong side effects, treatment is prescribed only after the laboratory confirms the fungal nature of the meningitis.
If meningitis is caused by allergic reactions or autoimmune diseases, these can be treated with cortisone medications. In other cases, treatment may not be necessary as the cause may go away on its own.
Rehabilitation
After treatment of the pathology, the patient must be monitored by a neurologist for two years. In the first year, he must be examined once every three months, and then once every six months. Recovery from illness is a complex and multifaceted process that includes:
- Dieting. All foods consumed must be boiled or steamed. It is recommended to consume lean meat and fish, dairy products, compotes and jelly.
- Physiotherapy, which includes massage, electrophoresis, electrosleep, magnetic therapy.
- Exercise therapy using gymnastic exercises and robotic simulators.
- Occupational therapy aimed at a person’s everyday adaptation due to a decrease in the patient’s physical capabilities.
- Cognitive therapy to restore attention, thinking and memory.
Bacterial meningitis: prevention
In order to prevent meningitis, it is necessary to follow all antiseptic rules when treating TBI, as well as isolate patients who are infected in separate rooms. Doctors recommend timely vaccination against this disease. If you come into contact with a carrier of the infection, you must visit a doctor to prescribe an antibacterial drug to prevent meningitis. It is necessary to lead a healthy lifestyle, observe the rules of personal hygiene, monitor your health, and promptly treat chronic diseases.
Meningitis is a dangerous disease that is better to prevent than to treat later. Often the disease leads to serious health problems that are permanent.
Source