With age, people begin to notice that their memory is not as good as before, and it becomes more and more difficult to concentrate on any task. The absent-minded state can go away on its own as stress is overcome, or it can be one of the symptoms of pathology - Alzheimer's disease.
The diagnosis was first described in detail in 1906. The disease affects the nervous system, causes the death of brain cells, and is chronic. This is one of the causes of dementia (senile dementia). According to Rosstat, in Russia more than 44 million people constantly live with this problem.
Timely diagnosis and proper treatment can significantly slow down the development of pathology and preserve the patient’s quality of life for a long time. In our clinic you can undergo the necessary examinations. MCB doctors will confirm or refute the diagnosis, advise on prognosis, and help you choose the treatment that is right for you.
Causes of the disease
There is no exact answer to the question about the causes of the pathology. Early-onset Alzheimer's disease may first appear before age 65 and is hereditary. Such cases account for about 5% of the total. If anyone in the family has already been diagnosed, you should seek advice from a geneticist.
Late-onset Alzheimer's disease is more common. The disease affects older people over the age of 65. The pattern of development of the pathology has not been identified. Although the essence of Alzheimer's disease is well known, it is impossible to say exactly why one person suffers from the pathology, while another maintains a clear mind even in old age.
According to the global Alzheimer's Association, several genes have been discovered that increase the risk of developing the disease:
- APOE allele e4 (risk gene) - every fourth case;
- determining gene (heredity, autosomal dominant Alzheimer's disease) - less than 1% of cases, only 1 confirmed diagnosis in the world.
Scientists suggest that the state of the nervous system is influenced by heredity, the environmental environment, and the patient’s lifestyle. The main risk factor is age. Other causes include midlife depression and smoking.
At the same time, a healthy lifestyle, proper nutrition, and regular physical activity have a beneficial effect on the body’s condition, but do not exclude the development of Alzheimer’s disease. Decades before the first symptoms appear, pathological changes already begin in brain cells. Amyloids and tau proteins are formed in tissues, blocking the function of nerve structures. Gradually, non-functioning cells die.
Other possible reasons:
- cardiovascular diseases;
- diabetes, excess weight;
- elevated cholesterol levels;
- hypertension;
- traumatic brain injuries.
Symptoms of Alzheimer's disease
The first sign of pathology is often memory impairment. The patient forgets names and faces, and it becomes difficult to find the right word in a conversation. When a person begins to notice memory deterioration with age, this is rarely paid attention to, associating the changes with the aging of the body. Gradually, the necrosis of brain cells spreads, and difficulty in performing daily activities is added to forgetfulness: cleaning the house, washing clothes, preparing food, etc.
In people engaged in intellectual work, symptoms of Alzheimer's disease appear later. Their brains are better able to adapt to change. In the early stages, the pathology may manifest itself as difficulty in choosing words during speech, difficulties in orienting in familiar terrain. Later, a noticeable decrease in memory occurs.
Other characteristic symptoms include:
- difficulties understanding spoken speech and written text;
- personality changes noticeable to close people;
- violation of the concept of time;
- difficulties with writing texts.
As Alzheimer's disease progresses, it turns into severe dementia, and the manifestations of the pathology vary from person to person.
Brush your teeth
It may be hard to believe, but those who skip brushing their teeth are at increased risk of not only tooth decay, but also brain cell damage! Scientists at the University of Bergen (Norway) have found a direct link between gum disease (gingivitis) and Alzheimer's disease. It turns out that the bacteria Porphyromonas gingivalis, which causes gum disease, also produces a protein that destroys nerve cells, leading to memory impairment.
Of course, this is not the only cause of Alzheimer’s disease, but while scientists are creating a cure, you can now take preventive measures and protect yourself from a possible threat: just regularly brush your teeth for at least two minutes twice a day, and also visit the dentist every six months for preventative hygiene and inspection.
Features of the course of the disease
In the early stages of Alzheimer's disease, the patient himself becomes aware of memory problems and tries to cope with them and carry out everyday activities. Diagnosis of pathology at this stage gives the most favorable prognosis. If a person does not notice deterioration, close people can help him with this.
As the pathology develops, obvious changes in the patient’s behavior are observed:
- often repeats itself in conversation, tells the same story several times;
- forgets answers to previously asked questions and asks them again;
- while going to the store, makes spontaneous purchases and acquires a lot of unnecessary things;
- spends more time on household chores and copes poorly with his daily responsibilities;
- loses the ability to learn, cannot acquire new knowledge and skills, for example, cannot cope with a new door lock;
- more often suffers from depression, apathy, refuses to meet with friends and go on visits;
- devotes less time to his appearance, allows sloppiness and sloppiness in his wardrobe.
Against the background of previous behavior, new habits are clearly visible, even if the patient first tries to hide his problems from others. Over time, the ability to self-criticize is lost, and memory loss becomes obvious. The patient begins to forget the names and faces of family members, does not remember his own last name, and loses orientation in space and time. An older person with late-stage Alzheimer's disease may no longer be aware that anything is wrong with them. Basic self-care skills disappear; assistance is needed when eating, going to the toilet, and changing clothes. Periods of clarity of consciousness occur less and less often.
Useful exercises for brain training
Special exercises can help to stimulate the brain cognitively. They can be performed independently or together with your loved ones. The main condition is their regularity.
Here are some examples of effective activities:
Place in front of you a piece of paper with a list of words written in different colors. You should start with the first word. But you need to name the color in which the text is written. After you reach the end, the words must be repeated in reverse order. It can be difficult at first, since different hemispheres of the brain are responsible for the perception of text and color.
Benefit: helps to establish new connections between the hemispheres of the brain, and also trains concentration and attention switching.
When performing this exercise, you should focus on the number “19” in the center of the square. Then you need to look for “1” and then all the other numbers in ascending order. You can draw the table yourself, and arrange the numbers in the cells in any order. This activity increases the speed of perception and processing of information and promotes the development of peripheral vision.
In older people, thinking, memory and speech are directly dependent on hand movements. In this regard, activities such as knitting, embroidery, or other activities that involve fine motor skills are helpful in maintaining mental clarity.
Fold the fingers of your right hand so that they show the “peace” sign, and show “ok” with the fingers of your left hand. Then, take turns changing your finger shapes so that your left hand shows “peace” and your right hand shows “ok”. Repeat several times. Then try doing this exercise with your right and left hands at the same time. Such gymnastics trains attention and the ability to quickly switch from one task to another.
Take two blank sheets of paper and two pens. The task is to draw geometric shapes with both hands at the same time. Instead of shapes, you can write letters or words with the same set of letters. Synchronous writing trains the brain to cope with several tasks simultaneously, involving both hemispheres in the work.
Diagnosis of Alzheimer's disease
When the first symptoms appear, you should consult a general practitioner, family doctor or neurologist. The patient is recommended to come to the appointment with a relative who can describe changes in behavior from the outside. The patient cannot always adequately assess his condition and often does not tell the doctor important facts.
Diagnostic procedure:
- Anamnesis collection. The doctor finds out what kind of life the patient leads, finds out his habits, place of work, what illness he had, and whether there is any family history.
- Analysis of clinical symptoms. You need to talk about your complaints and observations. The specialist will ask how long ago and with what intensity the symptoms of the disease have been increasing. It is better to keep a diary of observations from the first changes and show it to the doctor at the appointment.
- Assessment of the patient's condition at the time of consultation. The doctor conducts a cognitive test for attentiveness, memory, ability to navigate in space, and perform tasks. When assessing the actual condition, the patient’s level of education and the presence of concomitant pathologies, for example, hearing impairment, are taken into account. Tests such as the Mini Mental State Examination (MMSE) are used to determine the degree of dementia.
At the first appointment, a primary diagnosis of Alzheimer’s disease is carried out according to the algorithm described above and additional examinations are prescribed:
- General blood test and hormone levels. Based on the results, the doctor determines the presence of other diseases that can cause memory loss, for example, thyroid dysfunction, anemia, vitamin deficiency and others.
- Blood test for infections, HIV, syphilis. Treatment of diseases will help improve memory and get rid of other disturbing symptoms.
- Consultations with doctors of other specialties. To correctly diagnose Alzheimer's disease in the elderly, a conclusion from a geriatrician, psychiatrist, or neurologist may be required.
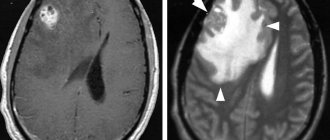
- Magnetic resonance or computed tomography of the head. The images show brain tissue and structures. Based on the examination results, pathologies such as hydrocephalus, stroke, and neoplasms are excluded.
- Neuropsychological examination. Patients with early-onset mild dementia undergo special tests to find out what type of memory impairment is present.
A comprehensive analysis of the examination results allows us to establish a diagnosis.
Traditional criteria for Alzheimer's disease:
- clinically confirmed dementia;
- impairments in 2 or more cognitive areas;
- preservation of consciousness;
- gradual decline in memory and other functions;
- age after 40 years;
- absence of brain diseases and systemic pathologies that can affect the functioning of the nervous system.
The National Institute for the Diagnosis of Age-Related Alzheimer's Disease guidelines also list characteristic biomarkers:
- beta-amyloid proteins in the brain, visible on PET scans;
- low levels of beta-amyloid and increased levels of tau protein in the cerebrospinal fluid;
- local atrophy of the temporal lobes and medial parietal cortex on the tomogram.
PHARMACOTHERAPY OF ALZHEIMER'S DISEASE: MYTH OR REALITY?
S. I. Gavrilova
Scientific and Methodological Center for the Study of Alzheimer's Disease and Associated Disorders of the Scientific Center for Clinical Prevention of the Russian Academy of Medical Sciences, Moscow
In the context of a changing demographic situation with a significant “aging” of the Russian population predicted for the next quarter of a century, the problem of dementia developing at a late age is becoming particularly relevant and socio-economically significant. According to WHO experts, Alzheimer's disease (synonym: Alzheimer's type dementia) is the most common cause of dementia in old age. In the last decade, Alzheimer's disease has been recognized as one of the four main medical and social problems of modern society. This is explained both by the steadily growing number of the population at risk of developing the disease, and by the duration of the disease and the severe disability of patients, requiring their lifelong hospitalization in psychiatric hospitals and psychoneurological boarding schools.
Epidemiological studies conducted at the Scientific Center for Health Care of the Russian Academy of Medical Sciences showed that 4.5% (more than 70 thousand people) of the Moscow population aged 60 and older suffer from dementia of the Alzheimer's type, and 1.8% of those examined (more than 30 thousand people) were diagnosed with pronounced and severe, i.e. requiring outside care and supervision, forms of dementia (Kalyn Ya. B., Gavrilova S. I., 1997). Extrapolation of the data obtained to the older population of Russia as a whole suggests that at present the total number of patients suffering from Alzheimer's disease in Russia is approaching 1.4 million people.
According to experts from the US National Institute of Aging, Alzheimer's disease ranks 4th among the causes of death in the US population, and the total number of such patients is about 4 million people. According to various estimates, from 40 to 78 million dollars are spent annually on medical and various types of social services for patients with Alzheimer's disease in the United States. (Henke S. I., Burchmore MJ, 1997). Similar indicators of economic costs for these patients are given by Canadian researchers (Ostbye T., Crosse E., 1987).
Unfortunately, we do not have corresponding data for Russia. However, even if we adjust these calculations in accordance with the more limited possibilities of diagnosis, treatment and social assistance for patients in Russia, it is obvious that the economic costs associated with Alzheimer's disease for Russian society (and, to an even greater extent, the moral burden of the families of patients) are truly enormous.
Despite the rapid development in the USA, Japan and Western Europe of molecular genetic, neurochemical and neurophysiological and other studies of Alzheimer's disease, which have made a significant contribution to the understanding of its pathogenetic mechanisms, the etiology of the so-called sporadic forms of the disease, constituting from 75 to 90% of all cases of the disease remain unknown, and accordingly, etiologically oriented therapy for the disease still does not exist.
However, in the last decade, attempts to target various parts of the pathogenesis of the neurodegenerative process underlying Alzheimer's disease have led to the development of several areas of therapeutic influence on the manifestations of this destructive disease.
Currently existing therapeutic strategies are represented by the following main directions: 1) compensatory (replacement) therapy aimed at overcoming neurotransmitter deficiency; 2) protective therapy: the use of neuroprotectors and neurotrophic factors; correction of disorders of free radical processes, as well as calcium metabolism; 3) anti-inflammatory therapy; 4) hormonal therapy; 5) behavioral therapy, including psychopharmacotherapy of productive psychopathological disorders and psychological correction (training) of cognitive functions.
The most numerous and well-developed compensatory therapeutic approaches are based on attempts to compensate for cholinergic deficiency, which plays a leading role in the pathogenesis of memory impairment and cognitive function in Alzheimer's disease. It is now generally accepted that the most effective approach to treating Alzheimer's disease is based on the use of acetylcholinesterase (AChE) inhibitors.
A representative of the new generation of AChE inhibitors is Exelon (rivastigmine). Exelon, a pseudoreversible carbamate-type AChE inhibitor with a selective effect on acetylcholinesterase in the central nervous system, has been successfully clinically tested in the USA and several European countries in two large multicenter (double-blind) studies (R. Anand, G. Gharabawi; 1996). A clinical study of Exelon conducted in our clinic also yielded extremely encouraging results regarding both therapeutic efficacy and clinical safety of long-term (6 months) use of the drug in patients with mild and moderate dementia of the Alzheimer's type. A feature of the use of Exelon is the individual selection of optimal therapeutic dosages at the level of maximum tolerated doses in the range from 3.0 to 12 mg/day and the possibility of its combination with other medications, often necessary for elderly patients.
In addition to cholinergic deficiency, which is the earliest and most pronounced manifestation of Alzheimer's disease, insufficiency of other neurotransmitter systems has also been established, in particular, serotonergic, glutamatergic, as well as impaired activity of monoamine oxidase (MAO) type B (Q. B. Baker, S. P. Reynolds , 1989; S. L. Lowe et al., 1990; K. Blennow et al., 1992). For these types of neurotransmitter deficiency, various means of replacement therapy are used, in particular the glutamatergic system modulator akatinol memantine (to correct glutamatergic dysfunction), serotonin reuptake inhibitors (citalopram) for serotonergic deficiency, etc.
There is also evidence of the successful use of MAO-B inhibitors (selegiline) for the treatment of Alzheimer's disease.
The symptomatic therapeutic effects of most of the drugs mentioned are considered proven, however, none of the methods of replacement therapy used have an established ability to reliably stabilize or significantly influence the course of the neurodegenerative process itself.
Protective therapy
is aimed at preserving and increasing the viability (survival) of neurons. It includes therapy with drugs that have neurotrophic properties, nootropics, antioxidants, vasoactive agents, etc.
The use of nootropics, for example, piracetam (nootropil), pyriditol (encephabol), which improve cerebral metabolism, has not, however, given reliable positive results in the treatment of patients suffering from Alzheimer's disease. The use of large doses of piracetam may even have a negative effect, since there is evidence of possible neurotransmitter depletion with its use.
New directions in pathogenetic therapy for Alzheimer's disease, based on the modern concept of neuroprotection, are associated with the development of neurotrophins. Unfortunately, despite significant experimental advances in this area, there is not yet a drug containing neural growth factor (NGF) available for peripheral administration and penetrating the blood-brain barrier. However, we can already talk about neuroprotective therapy for Alzheimer's disease using the drug Cerebrolysin, which has neurotrophic properties.
Cerebrolysin, a drug that has long been used in neurology for the treatment of stroke and other forms of cerebrovascular pathology, has been recommended in recent years for the treatment of dementia of the Alzheimer's type. It contains biologically active low molecular weight neuropeptides and has multimodal effects: a regulatory effect on brain metabolism, neuroprotective properties and a unique neuron-specific activity similar to that of NGF. Independent clinical studies conducted in different countries of the world (including double-blind trials) have proven the effectiveness of the drug for the treatment of Alzheimer's disease with intravenous drip administration of 20-30 ml of the drug in 150 ml of isotonic sodium chloride solution, and also showed the absence of any side effects (E. Ruether et al., 1994; N. Selezneva et al., 1997) when administered for a month.
Anti-inflammatory and estrogen therapy
are still under study (J. B. Rich et al., 1995). The basis for the development of these areas of therapy for Alzheimer's disease was epidemiological data, according to which individuals who have been receiving non-hormonal anti-inflammatory therapy or estrogen replacement therapy for a long time are significantly less likely to develop Alzheimer's disease.
Behavioral therapy.
Treatment of productive psychopathological disorders and behavioral disorders acquires particular importance in connection with... because it is precisely such manifestations of the disease that make patients difficult for examination, rehabilitation measures, and especially for care. However, it is extremely important to correctly assess the origin of psychotic symptoms, such as confusion. Delirium, acute confusion and other psychotic conditions of an exogenous type usually develop in patients suffering from dementia with the addition of additional exogenous hazards - most often intercurrent somatic diseases or with aggravation of somatic dysfunctions (for example, with intestinal atony and constipation), as well as as a result drug or other intoxication. Each case of the occurrence of psychotic disorders of an exogenous type requires a mandatory thorough (with the necessary clinical and laboratory studies) clarification of its cause and its elimination. Especially often, the worsening of symptoms of dementia and/or the development of states of confusion is caused by inadequate prescription of psychotropic drugs, in particular, drugs that have anticholinergic effects (tricyclic antidepressants), antipsychotics, beta-blockers, benzodiazepines and sedative hypnotics. Therefore, when treating patients with Alzheimer's disease, their use should be avoided if possible. This is a fundamental principle in the treatment of patients with Alzheimer's disease and senile dementia of the Alzheimer's type.
The growth in the number of patients suffering from Alzheimer's disease projected over the coming decades and the almost complete absence in practical medicine of Russia of treatments for this serious illness require urgent measures to be taken to develop means and methods of effective therapy for the disease. The above-mentioned current problems of pharmacotherapy of Alzheimer's disease, including the creation of therapy methods that stabilize the neurodegenerative process, and the development of differentiated therapeutic approaches are highly relevant tasks for domestic medical science.
The only specialized scientific and medical unit in Russia - the Department for the Study of Alzheimer's Disease and Associated Disorders of the National Center for Clinical Prevention of the Russian Academy of Medical Sciences - has been intensively engaged in multidisciplinary research into Alzheimer's disease and other debilitating processes of late age over the past 10 years. By the Decree of the Presidium of the Russian Academy of Medical Sciences dated October 25, 1995, it was entrusted with the function of the Scientific and Methodological Center of the Russian Academy of Medical Sciences for the study of Alzheimer's disease and associated disorders.
The research conducted in this scientific unit made it possible to make a significant contribution to the development of both basic and practical aspects of dementia of the Alzheimer's type. In particular, the standards for diagnosing Alzheimer's disease have been improved, and new (including neuropsychological, neurointrascopic and neurophysiological) methods for the differential diagnosis of dementia of various origins in the early stages of their development have been developed.
The concept of heterogeneity of Alzheimer's type dementia has been developed, creating the prerequisites for differentiated therapeutic approaches. The epidemiological indicators of mental disorders of late age, including Alzheimer's disease and other dementias, are determined and the trends in their dynamics in recent years are shown. Genetic and environmental risk factors for the development of Alzheimer's disease have been established for the domestic population.
Over the past 5 years, the Scientific and Methodological Center for the Study of Alzheimer's Disease has regularly studied new drugs (mainly from leading foreign companies) for the treatment of Alzheimer's disease.
During this period, a total of 445 courses of therapy with various medications were carried out, including 85 courses of neuroprotective therapy (Cortexin and Cerebrolysin), 255 courses of cholinergic therapy (including Amiridin 150, Gliatilin 50, Exelon 30, Arisept 25) . In addition, 105 courses of glutamatergic therapy with the drug akatinol memantine were carried out.
The studies conducted showed greater or lesser effectiveness of the studied drugs based on their impact on both the symptoms of cognitive deficits and the daily functioning of patients, as well as on the behavioral disorders that these patients had. Certain differences were found in the therapeutic effects of the studied drugs on various components of the dementia syndrome, including cognitive symptoms themselves, praxis and motor dysfunction, affective and psychotic disorders.
In addition, a certain dependence of the therapeutic response on the severity of dementia (stage of the disease) and on the characteristics of its structure was established. It was found that the quality of the therapeutic response is determined to a large extent by the characteristics of the ApoE genotype. Thus, it has been shown that patients who are carriers of the ApoE4 genotype respond to therapy with acetylcholinesterase inhibitors much worse than patients without the epsilon 4 allele in the ApoE genotype.
Thus, when prescribing a long course of very expensive therapy, for example, acetylcholinesterase inhibitors, it is necessary to take into account the possibility of the patient's reaction to the prescribed drug.
In connection with the above, there is an obvious urgent need for the development of differentiated therapeutic programs that are specifically focused on the characteristics of the course of the disease in its various clinical varieties, taking into account the genetic characteristics of patients. I think that solving these problems will become possible in the coming years.
The basis for such an optimistic assessment of the prospects for the development of pharmacotherapy for AD is the data from an analysis of the long-term effects of our original strategy of combined effects on various components of the pathological process underlying Alzheimer's disease. The basis of this strategy is a combination of replacement (cholinergic and/or glutamatergic action) and neuroprotective therapy.
In order to assess whether the treatment strategy we developed really produces obvious long-term results, we conducted a comparative assessment of the rate of progression of cognitive deficits in 2 groups (Table 1) of patients with mild and moderate dementia of the Alzheimer's type who were followed for at least 2 years ( Alzheimer's disease, according to ICD-10 and NINCDS/ADRDA criteria (GM McKhann et al., 1984).
Patients of group 1 (61 people) received at least 2 courses of combined therapy with various medications, including 28 patients with Cerebrolysin, 14 patients with Cortexin; gliatilin - 20; acetylcholinesterase inhibitors - 37; akatinol memantine - 24.
Table 1. Distribution of patients with Alzheimer's disease.
those who received
and did not receive therapy, depending on the severity of the initial condition
| Severity of dementia | Carried treatment | Treated patients | Total | MMSE |
| Mild dementia | 6 | 20 | 26 | 18-25 |
| Moderate dementia | 48 | 41 | 89 | 10- 17 |
| Total | 54 | 61 | 115 |
Patients of group 2 (54 people) did not receive drug treatment for at least 2 years. This group included 6 patients with mild and 48 patients with moderately severe dementia.
The state of cognitive functions of patients in both groups was assessed over time every 6 months using the MMSE scale (Folstein MF, 1975). The severity of dementia was determined in accordance with the CDR - Clinical Dementia Rating scale (Morris J. S., 1993).
As evidenced by the results of the comparative analysis, the state of cognitive functions in treated and untreated patients, who initially did not differ in the severity of dementia, underwent different dynamics during the observation period. The condition of untreated patients with initial moderately severe dementia after 12 months of observation corresponded to the MMSE score characterizing the onset of the stage of severe dementia (10 points and below). In the group of treated patients, even after 3 years of observation, the state of cognitive functions did not differ significantly from the initial level.
Puc .
l . Comparative dynamics of the state of cognitive functions (according to the MMSE } in treated and untreated AD patients with moderately severe dementia.
Untreated patients with initial mild dementia after 2 years of observation approached the border of severe dementia in terms of the state of cognitive functions. The average MMSE score in this group was after 2 years 12.3 + 3.1, while at the beginning of observation the state of cognitive functions in these patients was assessed by an average score of 21.2 + 1.6. The state of treated patients with mild dementia not only after 2, but even after 3 years of observation did not change for the worse compared to the initial level.The average MMSE scores in these patients were, respectively: 21.1 + 2.3, 22.7 + 4.5 and 21.9 ± 2.4 (Fig. 2).
Thus, we can talk not only about temporary symptomatic improvement, but also about a significant stabilizing effect of the therapy used, restraining the decay of cognitive functions and slowing down the onset of severe dementia for at least 2 years, even in patients with clinically severe dementia. Consequently, for these patients, the onset of total disability and the need for their lifelong placement in institutions for the chronically mentally ill are postponed by at least, and possibly more than 2 years.
Rice.
2. Comparative dynamics of the state of cognitive functions (according to the MMSE ) in treated and untreated voluntary AD with mild dementia.
In relation to patients with mild dementia, we can talk about achieving stable stabilization of the condition at the level of the initial manifestations of the disease. Thus, this category of patients was able to delay the progression of the disease to the stage of clinically pronounced dementia for several years, i.e., preserving the patient several years of independent and relatively fulfilling life, and in some cases, ability to work. We have not yet studied the economic aspects of therapy for Alzheimer's disease. However, according to US experts, the use of even the first generation AChE inhibitor, tacrine, makes it possible to reduce the economic costs of the patient from 7.5% to 17% (depending on the severity of the condition) mainly by reducing the time of permanent stay of patients in institutions for chronic sick.
The above assessment of the long-term effects of the combined therapy strategy used indicates that the treatment of Alzheimer's disease now, i.e., even in the absence of radical treatment methods for the disease, has ceased to be just a myth and has become a clinical reality.
Treatment of Alzheimer's disease
The earlier neurodegenerative changes are detected, the more effective the treatment. The therapy will preserve the patient’s intelligence and memory for a long time. Changes slow down, the patient and his family have time to adapt to the new way of life.
To treat the disease, drug therapy and measures to improve brain activity are prescribed. Depending on the patient’s condition, medications are selected to stabilize the mental state, to maintain the functioning of nerve cells (increasing the number of neurotransmitters, inhibiting cholinesterase), to eliminate concomitant pathologies.
To preserve intelligence, patients are recommended to:
- engage in creativity;
- actively carry out daily activities with other family members;
- communicate with friends and relatives;
- care for flowers in the garden or pets;
- increase physical activity (long walks in parks, walking, dancing, classes in groups for older people, etc.);
- play musical instruments, sing, etc.
Constant communication helps a person maintain attention, speech, and the ability to understand other people. Close relatives are advised to be patient and not show irritation from the patient’s forgetfulness or from his sometimes inappropriate remarks and questions. In order for a person to better understand the speech addressed to him, he needs to speak in short, simple phrases.
It is important to maintain your usual lifestyle as much as possible. If the patient was involved in painting or sports before diagnosis, he should continue to the best of his ability. Positive emotions have a beneficial effect on the health of the nervous system.
The disease progresses slowly. After diagnosis, a patient with high-quality drug support can live for many years. Late-stage Alzheimer's disease cannot be cured. The average life expectancy after immobilization is 6 months. Palliative care is indicated.
Prevention of Alzheimer's disease
The medical community has not yet provided convincing data. Prevention of Alzheimer's disease essentially comes down to eliminating precipitating factors.
The risk of developing pathology is reduced in the following cases:
- maintaining intellectual stress in old age: solving crossword puzzles, mastering new skills;
- prevention of hypertension;
- maintaining good physical shape;
- lowering blood cholesterol levels;
- proper nutrition including foods rich in saturated fats and omega-3 fatty acids.
Communicate
Socializing with people is not only a way to relax between activities, but also, as research shows, a means of improving cognitive function. It requires our attention, working memory, assessment of situations and the actions of other people.
Scientists from the universities of Michigan, California and Colorado recently published their research showing that even short, ten-minute intervals of social interaction can improve overall cognitive function.
According to the American Association of Retired Persons, social interaction is important as you age to maintain good mental health, memory, and prevent dementia and Alzheimer's disease.