General information about the disease
Meningitis is a dangerous disease that can cause serious consequences. The pathology is characterized by inflammation of the lining of the brain, in which a large amount of cerebrospinal fluid (CSF) begins to form, the medulla is damaged, and blood microcirculation in the vascular bed deteriorates.
The consequences of such inflammation are neurological changes that negatively affect the life and health of the patient, as well as cerebral edema - an emergency condition requiring immediate medical attention.
Factors causing the development of meningitis are divided into aseptic and purulent subtypes. The aseptic type is characterized by the viral nature of infection: enterovirus, herpes and choriomeningitis viruses. The purulent type of infection is caused by the intervention of bacteria: meningococcal, pneumococcal, staphylococcal - or external surgical influence.
For meningitis, depending on the nature of the infection, special treatment is required. To diagnose the causative agent of the disease and determine the method of therapy, a specific study of the spinal cerebrospinal fluid is performed - a puncture for meningitis.
Excess cerebrospinal fluid (cerebrospinal fluid) is produced in the cerebral ventricles. At the bottom of these areas of the brain there are plexuses of blood vessels responsible for the production of fluid. The cerebrospinal fluid passes through the ventricles and penetrates the subarachnoid space of the brain and spinal cord. Liquor is necessary to maintain an optimal level of intracranial pressure, provide shock absorption during shock and injury, and nourish brain tissue and cells. Liquor washes the lining of the brain and therefore represents a certain container for the accumulation of viruses and bacterial microorganisms during illness.
Insertion of a special needle into the subarachnoid space - lumbar puncture - is a modern and accurate method for diagnosing the causative agent of infectious meningitis using spinal cord fluid analysis.
4. Bone marrow biopsy results
Bone marrow biopsy results are usually ready within a week.
The following indicators are considered the norm:
- Bone marrow has normal amounts of fat, connective tissue, and iron. Normal ratio of adult and growing bone marrow cells.
- There are no signs of infection.
- There are no cancer cells such as leukemia, lymphoma or multiple myeloma.
- There is no spread of cancer cells from other affected areas.
Deviation from the norm:
- Bone marrow cells with pathology.
- The ratio of the number of different cells is disturbed.
- Bone tissue with pathology.
- Too much iron or too little iron (iron deficiency anemia).
- There are signs of infection.
- Cancer cells (leukemia, lymphoma, or multiple myeloma) are present.
- The bone marrow is replaced by scar tissue.
Depending on the results of a bone marrow biopsy or spinal tap, the doctor may prescribe additional examinations, select or adjust a treatment regimen, or, conversely, make sure that everything is in order with your health.
Features of the procedure
A puncture for meningitis is carried out as follows. The manipulation is carried out on the operating table, where the patient is positioned lying on his side with his legs pulled up to his chest. The head is tilted forward. The specific position of the body ensures the expansion of the intervertebral spaces, which facilitates the insertion of the needle and reduces the patient’s pain. In some cases, the procedure is performed while sitting (if the patient is overweight).
The target area from which material for analysis is taken is at the level of the 3rd – 4th lumbar vertebrae. To quickly and accurately determine the 4th vertebra, the following method is used: when connecting the iliac crests, a conditional line is drawn, which is located at the level of the desired vertebra.
The procedure is carried out under sterile conditions. The puncture site is treated with a disinfectant. After which the patient is injected with a drug for local anesthesia. The anesthetic is administered three times: intradermally, subcutaneously and additionally during manipulation.
The needle with the mandrel is inserted parallel to the spinous processes and slowly moved forward until it enters the cavity (feeling of failure). This means that the instrument has passed through the dura and ligaments and entered the subarachnoid space. An initial collection of cerebrospinal fluid is then performed to verify correct needle placement. After this, the material for research is collected into a clean test tube.
When assessing the result of the manipulation, the nature of the flow of cerebrospinal fluid into the test tube, the color and type of brain fluid are taken into account.
Normally, cerebrospinal fluid should flow out in the form of rare drops. With frequent and rapid flow, a significant increase in intracranial pressure is likely. The red tint of the secreted fluid indicates a possible hemorrhage in the subarachnoid space or damage to the vessel during puncture.
The duration of the procedure is about 7 – 10 minutes. In this case, the patient may experience quite unpleasant sensations. At the end of the manipulation, the needle is removed, the injection site is treated with an antiseptic and a bandage is applied. The patient must remain motionless for 2 to 3 hours after the puncture to eliminate the risk of cerebrospinal fluid leaking out of the hole.
A cerebrospinal fluid puncture can be taken not only to establish an accurate diagnosis and the causes of meningitis infection. The procedure is prescribed to eliminate intracranial hypertension through the direct administration of antibiotics. Also, during the manipulation, the pressure of the cerebrospinal fluid is measured and the patency of the cerebrospinal fluid tract is examined.
Analysis results
Each type of meningitis is characterized by a specific type of pathogen, which will describe changes in the spinal cerebrospinal fluid.
Viral meningitis is characterized by certain changes in the cerebrospinal fluid:
- the predominance of the concentration of lymphocytes over the content of leukocytes in percentage terms;
- absence of bacterial microorganisms in the sown material;
- clear color of cerebrospinal fluid.
Bacterial meningitis is accompanied by the following changes in the cerebrospinal fluid:
- increase in the number of neutrophils (above 1000 per 1 mm3);
- the predominance of the concentration of leukocytes over the number of lymphocytes in percentage terms;
- opaque color of cerebrospinal fluid;
- low glucose levels;
- the presence of a bacterial focus of infection;
- positive reaction on Gram stain.
In typical types of the disease, the level of neutrophils reaches 75–95%. The leukocyte norm for newborns is up to 30/mm3. At an older age, the concentration should not exceed 5 leukocytes per 1 mm3. In healthy children who do not suffer from viral or bacterial meningitis, monocytes and lymphocytes predominate in the cerebrospinal fluid.
Tuberculous meningitis is characterized by specific symptoms:
- the lymphocyte content reaches 100/mm3;
- low glucose;
- bacterial foci determined by staining of the cerebrospinal fluid;
- cloudy liquid.
Indications and contraindications for the procedure
Lumbar puncture is prescribed in the following cases:
- signs of neuroinfection (encephalitis, meningitis and others);
- risk of hemorrhage in the subarachnoid space;
- clarification of the diagnosis of liquorrhea;
- diagnosis of oncological processes and metastases in the lining of the brain;
- diagnosis of cerebrospinal fluid fistulas using cerebrospinal fluid puncture and injection of contrast agent;
- diagnosis and prevention of neuroleukemia in patients with hematological oncology.
If there are such indications, taking a puncture of liquor fluid is the only and key diagnostic method. In some cases, the procedure is used as an additional examination method:
- diseases accompanied by destruction of the membrane of neurons of the central nervous system and PNS (demyelinating processes);
- inflammatory polyneuropathy;
- attacks of fever in the absence of other symptoms.
3.How is a biopsy performed?
These procedures are performed by a hematologist, oncologist, internist, pathologist, or specially trained physician. In adults, a sample of bone marrow fluid is usually taken from the back of the pelvic bone. In rare cases, a fluid sample is taken from the chest or the front of the pelvic bone. In young children, samples are obtained from the front lower part of the lower leg, just below the knee. A bone marrow biopsy is taken only from the pelvic bone. The puncture is performed using a needle. A biopsy uses a special instrument that is screwed into the bone.
Risks and consequences of a spinal tap
Complications after puncture occur primarily when the rules of manipulation are not followed and doctors make mistakes. In other cases, the following consequences may occur:
- wedging of individual structural elements of the brain;
- dislocation of midbrain structures;
- damage to nerve endings causing pain in the patient;
- headaches, nausea, vomiting;
- hematomas at the site of needle insertion when small capillaries are damaged.
When taking cerebrospinal fluid material from pregnant women, the risk of spontaneous abortion increases, especially in the first third. Patients suffering from cardiovascular diseases also represent a risk group during manipulation. In particularly serious cases, the launch of vasovagal processes can provoke cardiac and respiratory arrest.
Contrary to popular belief that puncture can lead to paralysis, this complication is unlikely. The needle is inserted into the part of the spine that is most poorly innervated and the risk of damage to nerve endings is very low. The incidence of complications after puncture in patients does not exceed 1%.
After two weeks of intensive treatment, the patient’s health condition and the effectiveness of the chosen therapy method are assessed. To do this, repeat manipulation is performed with the collection of spinal fluid material for research. Based on the results of the puncture, changes in the cellular composition are analyzed and the presence or absence of a bacterial culture in the contents is determined. Positive dynamics indicate the patient’s clinical recovery.
Meningitis is a serious disease that requires accurate identification of the causative agent of the infection and the appointment of competent treatment. Cerebrospinal fluid puncture is the only and reliable method for diagnosing the disease.
Will an MRI show meningitis?
Frequent vomiting? Severe headaches? Do you think these are signs of poisoning?
These symptoms are not always associated with eating poor quality food or diseases of the digestive system. Today, with the radiologist of MRT Expert Lipetsk LLC, Alexander Konstantinovich Samaev, we are talking about such a terrible disease as meningitis.
- Alexander Konstantinovich, please tell me what kind of disease this is - meningitis and why it is dangerous?
The brain and spinal cord are covered by several membranes. Their inflammation is called meningitis.
The danger of this pathology is the occurrence of various kinds of complications, primarily from the central nervous system. This could be, for example, an abscess or cerebral infarction, venous sinus thrombosis, hydrocephalus.
- What causes this inflammation of the membranes?
These are mainly various bacteria, viruses, and fungi. One of the common pathogens that causes meningitis is meningococcus (N. meningitidis).
-What is the prevalence of meningitis? Is the mortality rate high for this disease?
Globally, it is estimated that 10 to 20% of people are carriers of meningococcal disease at any given time.
In Russia, per 100 thousand population there are about 3 cases of disease caused by this pathogen, and about 10 cases if we are talking about a viral pathogen.
The fatality rate for bacterial meningitis is 14%.
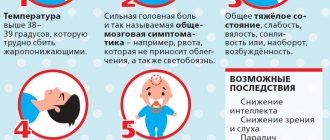
- How to recognize meningitis, what are its symptoms?
Manifestations of the disease are varied. In addition to general signs, such as increased body temperature, general weakness, there are symptoms that are quite characteristic of this pathology. This, for example, is a severe headache that cannot be relieved by common painkillers, a sharp tension in the extensor muscles of the neck (due to which the head seems to be thrown back and is difficult to tilt), arching of the back. Nausea and vomiting are also common, which does not bring relief and is not associated with food intake and pathology of the digestive system.
A pinkish or red rash may appear on the skin.
In children, dilation of the veins of the head and eyelids is often observed. In infants - bulging fontanelles.
-What are the ways of transmission of meningitis? Is it transmitted by airborne droplets or not?
It depends on the specific infectious agent. If we talk about meningococcus itself, it is transmitted by airborne droplets. In this case, the microorganism first enters the nasopharynx, and from there it is carried into the membranes of the brain with the blood.
The spread can also be by contact: for example, during purulent processes in the paranasal sinuses or middle ear cavity, when pus melts the bone wall and breaks into the cranial cavity.
- What to do at the first signs of meningitis?
Consult a doctor immediately for further diagnosis and treatment. Bacteria tend to multiply very quickly, so the infectious process will only progressively intensify.
- How is meningitis diagnosed?
The doctor receives important information already at the stage of examining the patient and identifying the symptoms listed above.
But to confirm the diagnosis, additional laboratory and instrumental research methods are needed.
This is, first of all, a so-called lumbar puncture, when a needle is used to puncture the membranes of the spinal cord in the lumbar spine and take a little cerebrospinal fluid (CSF) for examination. A natural question may arise: why and why, if meningitis is suspected, is a puncture performed in the lumbar spine? The fact is that cerebrospinal fluid circulates between the membranes of both the brain and the spinal cord, and inflammation in the membranes of the brain usually makes itself felt by changes in the cerebrospinal fluid wherever it is present.
The pressure of the cerebrospinal fluid is also determined at the same time - with meningitis it increases.
The liquid itself is subjected to microbiological and biochemical studies to detect the causative microorganism and signs of inflammation.
- That is, attempts are actually made to detect the infectious agent. Is it possible to somehow “see” the membranes of the brain themselves and their inflammation?
Yes it is possible. Will an MRI show meningitis? Undoubtedly. Moreover, the most suitable test for “visual” detection of meningitis is magnetic resonance imaging. It can also be successfully used to diagnose complications of this pathology.
Computed tomography can also be used to detect inflammation of the membranes.
I would like to note that meningitis is a serious infectious disease of the nervous system, and the choice of research method(s) for it is most often carried out by the attending physician, depending on the condition of the particular patient. Therefore, when its symptoms appear, which we talked about earlier, ask yourself the question “which method is applicable to detect meningitis: MRI or CT?” - a serious tactical mistake. You should immediately consult a doctor and entrust him with the further diagnostic algorithm.
- How is meningitis treated? Is this disease curable or not?
Of course, it is being treated. The causal factor must be influenced, i.e. bacteria, viruses, etc. Accordingly, antibacterial and antiviral drugs are prescribed. If meningitis is caused by an introduced infection, for example, from a purulent focus, it is searched for and eliminated (for example, in case of ENT pathology: purulent inflammation of the frontal sinus, middle ear cavity, etc.).
Therapy is also carried out aimed at relieving swelling of the membranes of the brain, eliminating seizures, and symptoms of intoxication.
- Alexander Konstantinovich, what could be the consequences of meningitis and how to avoid them?
We talked about some of them earlier: this is the development of an abscess or cerebral infarction, thrombosis of the venous sinus, hydrocephalus.
In addition, there may be hearing loss, infection in other organs, the appearance of epilepsy, a child's mental retardation, increased excitability and fatigue.
- What are the main measures to prevent meningitis?
Strengthening the immune system, routine vaccinations, compliance with sanitary and hygienic measures to prevent ARVI and other infectious pathologies.
For reference:
Samaev Alexander Konstantinovich
Graduate of the medical faculty of the North Ossetian State Medical Academy in 2008.
In 2009, he completed an internship in the specialty “Radiology”
Since 2013, he has been working as a radiologist at MRI Expert Lipetsk LLC.
Read more about Alexander Samaev here