Meningitis is a dangerous infectious disease that affects the meninges. It can be bacterial, fungal or viral in nature. Viral meningitis is also called serous meningitis and causes inflammation of the brain and spinal cord. Serous meningitis occurs most often in the summer, which is associated with the seasonality of some viral diseases. However, the risk of infection at other times of the year cannot be excluded. When the first signs of meningitis appear, it is important to consult a doctor as soon as possible.
At the Yusupov Hospital, the patient will be provided with all the necessary medical care: they will conduct an examination and prescribe adequate treatment. Experienced doctors at the Yusupov Hospital can quickly determine the type of disease and, without wasting time, begin therapy, which will reduce the risk of complications.
Causes
More than 60% of cases of serous meningitis are caused by enteroviruses, which are the main causative agents of viral meningitis. Infectious agents that cause inflammation of the meninges include:
- enteroviruses (70-80% of cases);
- arboviruses;
- Coxsackie viruses type A and B;
- parotitis;
- togaviruses;
- HSV type 2;
- cytomegalovirus;
- adenoviruses
The incidence of viral meningitis increases sharply in the summer. Rotavirus meningitis develops extremely rarely.
What to do if you are showing signs of illness?
ADVICE: When you notice the first symptoms, you need to see a therapist (if the course of the disease is acute, call an ambulance). You can seek help either at a local hospital or at a private clinic.
Treatment is carried out by a therapist (in uncomplicated forms) or an infectious disease specialist. Basic principles of treatment of meningitis in a hospital:
- prescription of antibacterial agents (antibiotics);
- relief of inflammation;
- removal of toxins (detoxification therapy);
- symptomatic treatment.
Medicines are administered intravenously; in severe forms, directly into the spinal canal. Traditional medicine is powerless in the fight against meningitis - treatment at home can result in death.
Symptoms
The incubation period for viral meningitis usually lasts 2-4 days.
The disease begins acutely, with high fever and general intoxication. In patients with high body temperature, malaise increases, muscle and joint pain, nausea and vomiting, abdominal pain, and diarrhea appear. Slight drowsiness and stupor are often associated. More severe signs of meningitis (impaired consciousness, stupor and coma) are not typical for inflammation of the meninges caused by viruses and require a more in-depth examination of the patient. From the first or second day of the disease, doctors determine a clearly defined meningeal syndrome:
- severe headache;
- repeated vomiting;
- lethargy and drowsiness, sometimes agitation and anxiety.
Patients may complain of cough, runny nose, sore throat and abdominal pain.
Often, patients with viral meningitis develop skin hyperesthesia (increased sensitivity to various irritants). On examination, neck rigidity and signs of severe hypertensive cerebrospinal fluid syndrome are revealed. During a lumbar puncture, clear, colorless cerebrospinal fluid flows out under pressure. An increased content of lymphocytes is determined in the cerebrospinal fluid, while the levels of protein, glucose and chlorides are within normal limits. After 3-5 days, body temperature normalizes. Sometimes a second wave of fever appears. In patients with viral meningitis, the following meningeal signs are determined:
- Kernig's symptom - the patient cannot straighten the leg bent at a right angle;
- Brudzinski's symptom: lower (when trying to straighten one bent leg, a reflex flexion of the second leg occurs), and upper - when bending the head, involuntary flexion of the lower limb occurs;
- Babinski's symptom - dorsiflexion of the first toe occurs with streak irritation of the plantar surface of the foot.
In most adults, viral meningitis occurs without complications. Some recovering patients complain of headaches for several weeks or months. They have mild intellectual impairment, asthenia or impaired coordination of movements. The prognosis for newborns and infants is not clear. They may have persistent complications in the form of intellectual impairment, learning difficulties, and hearing loss.
Epidemiology of the disease
Most often, the disease is transmitted by droplets. The entry point for infection is the mucous membranes of the respiratory tract, or gastrointestinal tract (less commonly). Also, the route of transmission of infection can be fecal-oral, blood-borne and vertical.
Bacterial, viral, fungal flora, malarial plasmodia, helminthiases, etc. can lead to the appearance of meningitis. However, in children the most common bacterial meningitis is caused by meningo-, pneumococcal infections, Haemophilus influenzae, Yersinia, stepto- and staphylococci.
The source of infection is a sick person or, much less frequently, a domestic or wild animal.
In the spread of true meningococcal infection caused by meningococci (Neisseria meningitidis), not only patients with severe forms of infection or meningococcal nasopharyngitis, but also healthy carriers of meningococci are of great epidemiological importance. Contact with seriously ill patients in the first days of their illness is accompanied by the highest risk of infection
Persons with meningococcal nasopharyngitis remain extremely infectious for up to two weeks. In this regard, the patient is subject to mandatory emergency hospitalization in an infectious diseases hospital.
Infection with meningococcal infection from a healthy carrier occurs less frequently, however, it should be noted that the number of carriers significantly exceeds the number of patients, so they play a significant role in the spread of the infection. The duration of carriage of meningococci in the nasopharynx ranges from two to three weeks (in rare cases, up to six or more weeks), and throughout this period the patient can release them into the environment when coughing and sneezing.
Children are more susceptible to infection and experience it in more severe forms. It should be noted that meningococcal infection is one of the dangerous and unpredictable infections in terms of the speed of its progression and the development of severe complications. In children, the generalized course of meningococcal infections is often extremely severe and, in the absence of timely specialized treatment, has a high risk of death.
Quarantine in schools, kindergartens, boarding schools, etc. for a period of ten days is established specifically for meningococcal meningitis. The quarantine period is calculated from the moment when the last patient was isolated.
Diagnostics
The diagnosis of viral meningitis can be reliably established or refuted by examining the cerebrospinal fluid.
A large number of lymphocytes and a slightly elevated protein level with normal glucose concentrations are detected in the cerebrospinal fluid. An indirect sign of the viral nature of meningitis is the absence of the pathogen in cerebrospinal fluid smears of any type of color. In the first 48 hours of illness, especially in some enterovirus infections and meningitis caused by eastern equine encephalomyelitis virus or ECHO virus 9, cytosis may be predominantly neutrophilic. In this case, the spin fluid analysis is repeated after 8-12 hours and it is monitored whether a lymphocytic shift has appeared. If neutrophils are present in the cerebrospinal fluid, an additional examination is performed to exclude bacterial meningitis or the presence of a focus of infection near the meninges.
Cytosis in viral meningitis does not exceed 1000 in one microliter of cerebrospinal fluid. Glucose levels are normal in most cases, but may be decreased in meningitis caused by the mumps virus, inflammation of the meninges caused by ECHO viruses and other enteroviruses, herpes simplex virus type 2, Varicella-zoster virus, or lymphocytic choriomeningitis. More often, lymphocytosis with low glucose levels is evidence of fungal, tuberculous or listeria meningitis or a non-infectious disease (sarcoid meningitis and diffuse tumor infiltration of the meninges).
Isolating the virus from cerebrospinal fluid is technically difficult. Adenoviruses and enteroviruses can be detected in feces, arboviruses in blood, mumps virus and cytomegalovirus in urine. Enteroviruses, mumps virus and adenoviruses are detected in nasopharyngeal swabs.
An important method for diagnosing viral meningitis is the detection of viral DNA or RNA using polymerase chain reaction (PCR). This method allows the detection of herpes simplex virus DNA in the cerebrospinal fluid of patients with Mollaret meningitis or herpetic encephalitis, even with negative culture results. PCR is widely used to detect Varicella Zoster virus, cytomegalovirus, and Epstein-Barr virus. This is the method of choice for detecting picornaviruses (poliomyelitis, Coxsackie, ECHO viruses) in the cerebrospinal fluid of patients suffering from meningitis.
Diagnosis of viral meningitis is carried out using electrophoresis of cerebrospinal fluid in agarose gel or isoelectric focusing of gamma globulins. These methods make it possible to identify oligoclonal immunoglobulins in meningitis caused by:
- human immunodeficiency virus;
- Human T-lymphotropic virus type 1;
- Varicella Zoster virus;
- mumps virus.
An increase in immunoglobulin titer is often accompanied by the appearance of antibodies to viral proteins.
Identification of oligoclonal immunoglobulins helps to carry out differential diagnosis, since they are absent in viral meningitis caused by enteroviruses, arboviruses and herpes simplex virus. Each patient with suspected viral meningitis at the Yusupov Hospital undergoes:
- general blood analysis;
- biochemical studies of liver function;
- determination of hematocrit, erythrocyte sedimentation rate, nitrogen and urea levels in the blood;
- determination of electrolytes and blood plasma glucose, creatinine, amylase and lipase.
Changes in certain indicators make it possible to clarify the nature of the disease.
Causative agents of meningitis
Depending on the type of pathogen, meningitis can be viral, bacterial, or fungal. Some protozoa (such as amoeba and toxoplasma) can also cause meningitis.
The development of viral meningitis can accompany the course of well-known infections - chickenpox, measles, rubella, mumps; damage to the meninges occurs with influenza and infections caused by herpes viruses. In weakened patients, in the elderly, and in infants, meningitis caused by fungi occurs (it is clear that in these situations it is the lack of immunity that plays the leading role in the occurrence of the disease).
Bacterial meningitis is of particular importance. Any purulent focus in the body - pneumonia, an infected burn, tonsillitis, various abscesses, etc. - can cause meningitis, provided that the pathogen enters the blood and reaches the meninges with the blood flow. It is clear that the well-known causative agents of purulent processes (staphylococci, streptococci, Pseudomonas aeruginosa, etc.) will be the causative agent of meningitis in this case. One of the most terrible is tuberculous meningitis - almost forgotten, it is now occurring more and more often.
At the same time, there is a microorganism that causes meningitis most often (60-70% of all bacterial meningitis). It is not surprising that it is called meningococcus. Infection occurs by airborne droplets, meningococcus settles on the mucous membranes of the nasopharynx and can cause a condition very similar to a common respiratory viral infection: a slight runny nose, redness of the throat - meningococcal nasopharyngitis. It was not for nothing that I used the phrase “can cause” - the fact is that the entry of meningococcus into the body quite rarely leads to the onset of disease, the leading role here belongs to very special individual changes in immunity. Two facts are easily explained in this regard: the first is the risk of developing meningitis during contact, for example, in children's institutions is 1/1000, and the second is the frequent detection of meningococcus in the nasopharynx in completely healthy individuals (from 2 to 5% of children are healthy carriers). The body's inability to localize the microbe in the nasopharynx is accompanied by the penetration of meningococcus through the mucous membrane into the blood. With the bloodstream, it enters the meninges, eyes, ears, joints, lungs, adrenal glands, and in each of these organs a very dangerous inflammatory process can occur. It is obvious that damage to the meninges is accompanied by the development of meningococcal meningitis.
Sometimes meningococcus enters the blood quickly and in huge quantities. Meningococcal sepsis, or meningococcemia, occurs - perhaps the most terrible of all childhood infectious diseases. The microbe secretes poisons (toxins), under their influence multiple blockages of small vessels occur, blood clotting is impaired, and multiple hemorrhages appear on the body. Sometimes, within a few hours after the onset of the disease, hemorrhage occurs in the adrenal glands, blood pressure drops sharply and the person dies.
There is an amazingly dramatic pattern in the occurrence of meningococcemia, which is as follows. The fact is that when a microbe penetrates the blood, it begins to react with certain antibodies that try to destroy meningococcus. It has been proven that there is cross-activity of a number of antibodies - that is, if there are large quantities of antibodies, for example, to streptococcus, pneumococcus, staphylococcus - then these antibodies can have an inhibitory effect on meningococcus. So it turns out that children who are sick, have chronic foci of infection, have had pneumonia and many other illnesses, almost never suffer from meningococcemia. The scary thing about meningococcemia is that within 10-12 hours an absolutely healthy child who has never been sick before can die!
Treatment
At the Yusupov Hospital, doctors provide treatment for viral meningitis, aimed at preventing or limiting the formation of irreversible damage to the brain. To destroy pathogens of viral infection, patients are prescribed the following medications:
- recombinant α-interferon;
- inducers of endogenous interferon (neovir, cycloferon);
- RNase;
- intravenous immunoglobulins (intraglobin F).
Antiviral drugs are prescribed from 2 to 5 days of illness or in severe condition of a patient with viral meningitis.
In severe cases of the disease, glucocorticoids are used during the first 2-3 days of the disease: dexamethasone or prednisolone. If the patient develops complications, antibacterial drugs are prescribed. For serous meningitis caused by a virus or Epstein-Barr, acyclovir is prescribed. For immunocompromised patients, immunoglobulin is administered intravenously. To reduce intracranial pressure, furosemide, Lasix or acetazolamide are prescribed. With severe cerebral edema, treatment with mannitol is started. Detoxification therapy is carried out with glucose solution, rheopolyglucin, albumin, plasma. Crystalloid and colloid solutions are administered intravenously.
When the body temperature is above 38 degrees, antipyretics are used - paracetamol, ibuprofen. All patients with serous meningitis at the Yusupov Hospital are prescribed drugs that improve the metabolism of cells of the central nervous system: piracetam, nootropil, picamilon. To reduce the energy deficit of the brain and improve tissue metabolism in viral meningitis, ascorbic acid and riboxin are prescribed. In severe cases of the disease, antioxidants are prescribed - cytomol, cytochrome. From the first day of therapy, all patients with viral meningitis are prescribed drugs that improve cerebral circulation (Cavinton, dipyridamole).
Variants of the course of the disease
When directly infected with a pathogenic agent in the absence of a general infectious lesion of the body or a disease of another organ, meningitis is called primary. Most often caused by viruses and bacteria. Secondary is always a complication of a local or affecting the entire body.
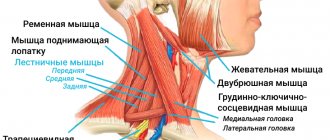
The most common causes of secondary meningitis:
- acute, chronic ear infection (otitis);
- inflammation of the nasal sinuses (frontal sinusitis, sinusitis);
- purulent processes in the soft tissues of the face, neck (boils, carbuncles, abscesses);
- bone damage (osteomyelitis);
- lung abscess.
The pathogens spread to the membranes, resulting in the disease.
Meningitis can be acute, even lightning fast, with the formation of a large amount of pus, severe dysfunction of the nervous system, and the threat of complications and death.
Chronic (long-term, more than 1 month) and subacute (more than 2 weeks), in the absence of antibiotic therapy, processes develop against the background of chronic, protracted infections.
The most significant:
- tuberculosis;
- sarcoidosis (formation of granulomas in the lungs, pleura, and other organs);
- candidiasis (fungal infection);
- AIDS;
- syphilis;
- malignant tumors.
They don't show up as brightly. People suffering from such diseases need constant medical supervision and timely detection of any changes in the picture of symptoms.
The spread of HIV infection, the incidence of AIDS, and the use of a large number of medications in the arsenal of therapeutic agents that weaken the immune system disrupt the natural defenses of the human body. With this option, infection occurs with microbes to which a healthy body is insensitive. The main causative agents of meningitis in such patients are fungi, most often cryptococci.
Against the background of severe diseases and specific treatment, neoplastic (carcinomatous) meningitis may occur. It is characteristic of malignant tumors of the blood (leukemia), nervous structures of the brain, spinal cord (gliomas, blastomas). It is the result of damage to the oncological processes of the membranes, which causes a negative effect on the nervous system and worsens the prognosis.
Prevention
To avoid getting viral meningitis, you should not swallow water while swimming in open water.
You should observe the rules of personal hygiene and thoroughly wash vegetables and fruits before eating. To prevent influenza, vaccination is carried out. If you have signs of viral meningitis, call the Yusupov Hospital. Doctors examine patients using equipment from leading European and American companies. To treat patients, neurologists use effective antiviral drugs that have a minimal range of side effects.
Make an appointment