Serous meningitis is a lesion of the membranes of the brain, which is characterized by a serous inflammatory process. Serous meningitis in children and adults develops when viruses, bacteria or fungi enter the body. In 80% of clinical cases, serous inflammation of the membranes of the brain and spinal cord is caused by viruses. Viral meningitis affects preschool children, schoolchildren and adults. At the Yusupov Hospital, the nature of meningitis is determined using modern laboratory methods for studying cerebrospinal fluid, blood and other biological materials.
To diagnose changes in the brain, innovative research methods are used using the latest equipment from European and American manufacturers. Doctors take an individual approach to the treatment of each patient suffering from serous meningitis and use modern antiviral and antibacterial drugs registered in the Russian Federation. Neurologists take into account the sensitivity of viruses to the drug and the patient’s body’s response to antimicrobial therapy. Rarely, serous viral meningitis is reported in adults.
Causes
Serous viral meningitis is an infectious disease.
In 75-80% of cases, viral meningitis is caused by enterovirus infection (Coxsackie and ECHO viruses). Less commonly, the cause of serous meningitis is the mumps virus, adenoviruses, Epstein-Barr virus (the causative agent of infectious mononucleosis), cytomegalovirus, herpes and measles viruses. HIV infection can also lead to the development of viral meningitis. Viral meningitis has a seasonal incidence, which depends on the type of pathogen. Most cases of serous meningitis occur in the summer. The mumps virus has a peak incidence in spring and winter. Serous meningitis can be not only viral, but also bacterial (with syphilis, tuberculosis), and sometimes fungal.
Transmission routes
The incubation period for serous viral meningitis is 2-4 days. Depending on the type of pathogen, the following paths take place:
- transmission of serous meningitis pathogens:
- airborne (from coughing, sneezing);
- contact (in the case of direct contact of a child or adult with the skin of a patient or with infected objects);
- water (when swimming in bodies of water contaminated with infectious agents).
The causative agents of serous viral meningitis reach the meninges by hematogenous (through blood vessels), lymphogenous (with lymph flow) or perineural (with cerebrospinal fluid) route. The peak incidence of serous meningitis occurs in the summer. Preschoolers and children of primary school age, as well as persons with immunodeficiency conditions or weakened by other serious illnesses, are most susceptible to the disease.
Symptoms
Serous meningitis, as well as inflammation of the meninges of bacterial origin, is characterized by common meningeal symptoms:
- nausea;
- Strong headache;
- temperature increase;
- repeated vomiting.
Distinctive features of serous meningitis of viral origin are the very abrupt onset of the disease.
Consciousness is slightly impaired. When serous meningitis is detected, symptoms in children may be mild. This type of meningitis does not last long and has a favorable outcome. In most cases, there are no complications after serous meningitis. With serous inflammation, cerebral edema develops. The outflow of cerebrospinal fluid is disrupted. Brain swelling provokes an increase in intracranial pressure. Unlike bacterial purulent meningitis, the serous form of inflammation does not lead to massive exudation of neutrophils and brain cells do not die.
From the second or third day of the disease, serous meningitis manifests itself as a pronounced meningeal syndrome. A mandatory sign of serous viral meningitis is fever. Patients' temperature rises to 40 degrees, then after 3-4 days it decreases and after a while it rises again. 2 waves of high temperature are recorded. With mild viral meningitis, this does not always happen.
A painful headache constantly accompanies a patient suffering from viral meningitis. It starts from the temples, intensifies when moving the eyes, from bright light and harsh noise. This type of headache is difficult to control with painkillers.
Children may experience limb cramps and general irritability increases.
They become whiny and capricious. In newborns, the fontanel swells and a “brain” cry appears. Intoxication causes general weakness, malaise, muscle and joint pain. Patients are concerned about nausea, repeated vomiting, and lack of appetite. Abdominal pain and diarrhea appear. Often children, in addition to meningeal symptoms, show signs of acute respiratory viral infection:
- mucous discharge from the nose;
- a sore throat;
- cough.
Skin sensitivity increases.
Patients react sharply to loud sounds, bright lights, noise, and touch. A patient with meningitis feels much better in a quiet, darkened room. In this case, the child lies on his side in bed, his head is thrown back, his knees are pressed to his stomach, his hands are pressed to his chest. In infants, tension and bulging of the fontanel occurs, Lesage's symptom appears - if the baby is lifted up, holding it under the armpits, he pulls his legs towards his stomach and bends them. With viral serous meningitis, there may be minor disturbances of consciousness (stunning or drowsiness). Sometimes signs of damage to the cranial nerves develop, difficulties with swallowing, double vision, and strabismus appear. Motor activity disorders manifest themselves as partial or complete paralysis.
In patients with serous viral meningitis, the following meningeal signs are determined:
- Kernig's symptom - the inability to straighten a leg bent at a right angle;
- Brudzinski's symptom: lower (when trying to straighten one bent leg, a reflex flexion of the second leg occurs), and upper - when bending the head, involuntary flexion of the lower limb occurs.
- Babinski's symptom - with line irritation of the plantar surface of the foot, dorsal flexion of the first toe is observed.
The duration of serous meningitis is on average 10 days.
Make an appointment
The first signs and symptoms of meningitis in a child
Clinical picture of the disease
Meningitis is most dangerous for children from 3 to 5-6 years old - the first signs in a child appear as a cold or flu, and since at this age patients cannot yet describe their condition, parents often discover symptoms of inflammation late.
In order to start treatment on time, it is important to know the characteristics of the disease. The lesion affects the lining of the spinal cord or brain. An acute inflammatory process quickly affects soft and arachnoid tissues, leading to swelling and increased intracranial pressure. Meningitis often develops against the background of viral and cold infections, but fungal and bacterial varieties are the most dangerous. The patient may feel a rapid deterioration of the condition over several days, which without treatment can lead to death.
The main way pathogens spread is hematogenous, that is, through the blood. Microorganisms enter the ducts and attack the bone marrow. Less commonly observed is the route through purulent wounds, abscesses at the base of the skull, nose or ear. Pus enters the arachnoid membrane, forming a focus of the disease there. Next, a chain reaction occurs - inflammation affects a wide area. The larger the radius of infection, the more pronounced the swelling.
The disease has a long incubation period - the first symptoms of meningitis in children from 3 to 5 years old may appear after one or two weeks. During this time, the child will feel weak, unwell, and there will be a slight increase in temperature.
Statistics and Risk Factors
The disease is more often diagnosed in preschool children and adolescents. Among adults, pensioners are the most vulnerable. Boys are more often infected than girls; this trend remains among the older generation - women are diagnosed less often.
Exacerbations and epidemics occur under the following conditions:
- The cold season is from late autumn to mid-spring. Temperature changes and wind contribute to the emergence of a source of infection.
- Poor ecology, in particular, lack of fresh air. Residents of megacities are more often admitted to hospitals with this diagnosis.
- Failure to comply with sanitary standards. This rule applies to regions and entire countries. In the population of Africa, South America and Southeast Asia, 40% more patients were identified than in Europe.
Causes of meningitis in children and manifestations of varieties of the disease
There are several options for causative agents of inflammation of the lining of the brain:
- Bacteria. These are meningococci, pneumococci, Haemophilus influenzae serogroup b, staphylococci, enterobacteria, mycobacterium tuberculosis, listeria monocytogenes, propionibacteria acne, diplococci. This group can be called the largest. Such pathogens multiply very quickly and attack healthy cells. The tissues quickly swell, increasing the risk of internal bleeding. The course of the disease is very acute and rapid, and the incubation period of this variety is the shortest. The main symptoms of childhood bacterial meningitis are: high fever, intoxication and delirium.
- Viruses. Often, inflammation of the lining of the brain is the result of damage to the body by enterovirus, echovirus, Coxsackie, mumps, chickenpox, measles, rubella, polio, tick-borne encephalitis, herpes or adenoviruses. The main problem with this course of the disease is its disguised manifestation, since all the initial signs indicate only the primary disease. Moreover, such a latent period can last up to two weeks.
These are the main causes of infection. Less commonly, infestation can be caused by:
- fungi;
- protozoa;
- helminths and other pathogens.
Depending on the source of infection, the following clinical types of meningitis in children are distinguished:
- Bacterial.
- Viral.
- Fungal.
- Protozoan.
- Mixed.
- Non-specific. Its nature has not been established, but there are documented cases of infection.
The types of disease are also distinguished by the nature of inflammation:
- Purulent. Accompanied by the release of pus in the foci of infection.
- Serous. The main manifestation is swelling without extraneous masses.
Methods of infection - routes of invasion
It is dangerous for a preschool child to be in a kindergarten or other educational institution during an epidemic if a case of the disease has been recorded in the group. The main reason is household contact. You can become infected through:
- air, in case of a viral cause;
- natural fluids - saliva entering when coughing or sneezing;
- water when the source of infection is bacteria or parasites;
- bodily contact if the infection is fungal in nature.
Risk factors and causes of infection:
- Stress and worries. It often accompanies the period of kindergarten and the transition to first grade for a student. At this time, parents need to be as attentive as possible to the emotional state of the child.
- A severe form of a viral disease - influenza, ARVI, sore throat, pharyngitis, pneumonia, etc. It is very important to complete the course of treatment and limit contact with others when the immune system has not yet strengthened. To restore immunity after an illness, “Tsitovir-3” for children – in the form of syrup or suspension – effectively helps. It can be taken by children from one year old. And after 6 years, doctors recommend prophylaxis with capsules. The course lasts only 4 days, it should be carried out once every six months, and if necessary (during epidemics, the first signs of a cold) repeated.
- The presence of chronic forms of certain diseases - syphilis, diabetes, tuberculosis, HIV infection.
- Poor nutrition, lack of fruit. A growing body requires more vitamins and microorganisms, so a good appetite must be encouraged, but within realistic limits. Overeating and excess weight also lead to a slow metabolism - proteins, fats and carbohydrates are not fully absorbed, and a malfunction occurs in the digestive system. The optimal solution is a healthy diet and a well-composed diet.
- Head and back injuries. This can cause a concussion, swelling of the brain, pinched nerves, or impaired blood flow. A compressed vessel can initiate an abscess where infection will accumulate.
- Hypothermia and high negative temperatures. This point is especially relevant for teenagers who prefer light jackets to warm down jackets and a bare head over a hat. Pay close attention to your child's wardrobe.
- A large number of medications that weaken the immune system - the body stops fighting pathogens on its own. To support the production of natural interferon, take an immunomodulator in combination with prescribed medications. "Tsitovir-3" will support the child's protective functions even while taking antibiotics.
What are the symptoms of meningitis in children?
At the first stage of the disease, all signs are smooth, so many parents often mistake the onset of inflammation of the lining of the brain for a cold or ARVI. The main ones are:
- Headache. At first it can be expressed as dizziness, mild malaise, and over time it becomes permanent, bordering on migraine.
- Lack of appetite. Along with this, there is a constant desire to drink due to a dry throat.
- In young patients, a complete imbalance of the intestines occurs - peristalsis increases, diarrhea appears.
- General weakness, body aches.
- A sharp reaction to light, loud sounds and touches.
- Temperature increase.
Over time, symptoms become more pronounced:
- Fever up to 40 degrees, which is difficult to reduce even under the influence of strong medications.
- Redness of the skin, rash. The skin begins to itch and sweat. When pressed, the redness goes away.
- Numbness of the neck muscles - it is difficult for the child to turn his head. This is especially noticeable in infants.
- Urge to vomit, nausea.
- Nervous overexcitation or pathological fatigue, insomnia, hallucinations.
- Loss of coordination, fainting.
- Conjunctivitis, redness of the whites, pain in the eyes.
- Enlarged axillary and cervical lymph nodes, less often - tissue in the groin area.
- Painful sensations when pressing on the space between the eyebrows or forehead.
These signs of childhood meningitis can be recognized at home and immediately contact a specialist. The doctor will conduct a more complete diagnosis, including identifying the presence of the following symptoms:
- Kernig - muscle stiffness in the knee;
- Brudzinsky - involuntary movement of the limbs;
- Bekhterev - reduction of a number of tissues on the face during certain manipulations;
- Pulatova – pain in specific points of the skull;
- Mendelian – painful sensations in the ear area;
- Lesage - swelling of the fontanel in infants.
The disease may also be accompanied by:
- complications in the eyes - blurred vision, temporary loss of vision;
- decreased hearing threshold;
- cough and runny nose;
- convulsions of the limbs;
- heart rhythm disturbances;
- increase or decrease in pressure;
- uveitis.
What are the signs of meningitis in children under 1 year of age - symptoms for urgent medical attention?
- Decreased motor activity, decreased period of wakefulness, lethargy.
- Instant increase in temperature to 39-40 degrees.
- Changing body position - the baby turns out, bends his back, rests his head on the pillow.
- Lack of appetite, refusal of breast milk.
- Feeling worse when touching the neck or base of the head.
- Frequent regurgitation.
- Pale with pronounced red spots.
Depending on the cause of the invasion, the patient will have a different incubation period. But in most cases, all signs appear quickly, so you should immediately consult a doctor.
Treatment and prevention
It is strictly forbidden to be treated without examination by a pediatrician. If meningitis is suspected, emergency hospitalization and bed rest are prescribed. Only a professional can write a prescription, according to which the following will need to be included in drug therapy:
- Antibiotics.
- Antiviral drugs.
- Antimeningococcal gamma globulin.
- Symptomatic medicines: for fever, body pain, cough, vomiting and diarrhea.
- Nootropic drugs.
- Tablets and solutions for intoxication.
- Immunomodulators.
To protect your child from infection even during an epidemic, take preventive measures. Strengthen your immune system with the immunostimulant Cytovir-3. The active substances support the natural induction of endogenous interferon at a high level, which guarantees good protection of the body from bacteria and microbes.
Protect your children from hypothermia and carefully monitor the first signs of illness.
Diagnostics
The diagnosis of serous viral meningitis can be confirmed or excluded only based on the results of a cerebrospinal fluid examination.
CSF is obtained using lumbar puncture. It is performed at the slightest suspicion of viral meningitis. Contraindications for spinal puncture for serous viral meningitis are:
- infectious-toxic shock.
- signs of brain herniation (a combination of arterial hypertension and bradycardia, increasing focal symptoms, depression of consciousness, impaired pupillary reactions);
- infectious lesions of the skin and soft tissues in the area of the spinal puncture;
- convulsive status.
Cerebrospinal fluid in serous viral meningitis is always clear and colorless.
Its pressure reaches 300 - 400 mm. water Art. In the cerebrospinal fluid, a moderate increase in the number of lymphocytes is determined (from 30 to 800 cells in 1 μl). In the first days of the disease, neutrophils can be detected in the cerebrospinal fluid, and from the second or third day lymphocytes appear. The protein content may be normal or reduced, the level of sugar and chlorides does not change. By slowly releasing 3-6 ml of cerebrospinal fluid during the first puncture, intracranial pressure decreases, so patients experience less headaches and significantly improve well-being. In the peripheral blood there is a reduced number of leukocytes, a slight increase in the content of neutrophils without a significant shift in the leukocyte formula to the left, and a moderate increase in the erythrocyte sedimentation rate. By the beginning of the second week of the disease, the number of eosinophils in the peripheral blood increases.
Expert opinion
Andrey Igorevich Volkov Neurologist, Candidate of Medical Sciences
The viral nature of inflammation of the meninges accounts for 80% of cases. Serous meningitis is most often caused by enteroviruses. The disease is most common in children, but in some cases, viral meningitis also affects adults. The symptoms of serous pathology have no distinctive features compared to other forms.Without prescribing etiotropic therapy, in more than half of cases, meningitis ends in death. The infectious disease quickly becomes severe and complicated. In 10% of cases, death occurs within 1–2 days, even with treatment started.
At the Yusupov Hospital, neurologists use their entire diagnostic arsenal to identify infectious diseases. The main method for detecting viral meningitis in adults is cerebrospinal fluid analysis. With its help, the pathogen is determined. CT and MRI are highly informative. Their results make it possible to determine the localization of the pathological focus in the brain. Based on the data obtained, etiotropic therapy is selected. Depending on the accompanying symptoms, symptomatic treatment is selected.
Diagnosis of meningitis
The main methods for diagnosing meningitis include:
- Cerebrospinal fluid examination. Cerebrospinal fluid is obtained using a lumbar puncture. When diagnosing meningitis, various fluid characteristics are determined (transparency and color, number and composition of cells, amounts of protein, glucose, and the presence of microflora), which make it possible to identify changes characteristic of meningitis.
- X-ray of the skull.
- Fundus examination.
- Computer and nuclear magnetic resonance tomography.
- Electroencephalography.
The diagnosis of meningitis is established based on a combination of 3 signs:
- Presence of symptoms of meningitis.
- Signs of infection.
- The presence of characteristic changes in the cerebrospinal fluid.
Treatment
Treatment of serous meningitis is aimed at preventing or limiting the formation of irreversible brain damage. Doctors do not use antibacterial drugs in the treatment of serous meningitis of viral origin. Means aimed at destroying infectious agents include:
- recombinant α-interferon (Viferon in suppositories);
- inducers of endogenous interferon (cycloferon, neovir);
- RNase;
- intravenous immunoglobulins (intraglobin f at a dose of 3 ml/kg per day), which are prescribed from the second to the fifth day of the disease or in severe condition of the patient.
In severe cases of the pathological process, glucocorticoids are used: prednisolone or dexazone during the first 2-3 days of the disease.
Antibiotics are prescribed only for the development of bacterial complications of serous viral meningitis. For serous meningitis caused by the herpes virus or Epstein-Barr virus, acyclovir is prescribed. Infants and immunocompromised patients need nonspecific and specific antiviral therapy. They are given intravenous immunoglobulin. To reduce intracranial pressure, diuretics are prescribed - furosemide, Lasix, acetazolamide. For severe cerebral edema, the starting drug is mannitol. In order to reduce the manifestations of intoxication, infusion therapy is carried out. The volume of intravenous fluid administered is 2/3 of the child’s physiological need for water. It must strictly correspond to the amount of fluid removed. A 10% glucose solution, rheopolyglucin, albumin, and plasma are used. Colloidal and crystalloid solutions are administered.
At temperatures above 38 C, antipyretics are used - ibuprofen, paracetamol. Anticonvulsants include seduxen (Relanium), GHB (sodium hydroxybutyrate 20%). For persistent disturbance of consciousness, intractable repeated convulsions, central hyperthermia (increased temperature) and arterial hypertension, sodium thiopental is administered intravenously.
The use of barbiturates requires the patient to be placed on artificial ventilation. It is carried out at the Yusupov Hospital using expert-class ventilators. All patients with serous meningitis are shown early administration of drugs that improve the metabolism of cells of the central nervous system. Neurologists use piracetam, nootropil, picamilon. Nootropics are first administered intravenously and then patients take them orally.
Ascorbic acid and riboxin help reduce brain energy deficiency and improve tissue metabolism during meningitis. In severe cases of the disease, antioxidants (cytochrome, cytomol) are prescribed. Medicines that improve cerebral circulation are prescribed to all patients from the first day of treatment. The drugs of choice are Cavinton (Vinpocetine) and dipyridamole (Curantyl). The most effective is the combined use of vasoactive and neurometabolic drugs (instenon and actovegin).
Consequences
Serous meningitis can have various consequences.
When the first symptoms of this disease appear, it is important to seek medical help promptly. The best thing to do is call an ambulance. Treatment of serous meningitis must necessarily take place in a hospital setting. Self-medication is unacceptable. The sooner adequate medical care is provided, the greater the chance that the consequences of the disease will never appear or will be minimal.
In cases where the patient delays treatment for too long, the following complications may occur:
- blindness;
- deafness;
- brain disorders;
- dysfunction of the speech apparatus;
- delay in psychomotor development.
In medical practice, in the advanced stage of serous meningitis, in the absence of treatment, paralysis, coma and death occurred. But this is rather an exception to the rule. In most cases, serous meningitis is not as serious as, for example, tuberculosis.
Even with favorable treatment and prognosis, the patient may experience headaches for a long time. If after a course of therapy pain persists for more than 2 months, you should definitely consult a doctor. If necessary, repeated examination is possible.
Symptoms of serous meningitis
Serous meningitis in children usually begins with a sharp rise in temperature and the appearance of a severe headache, after which other signs of this disease may appear. The virus is extremely stable in the external environment and can easily exist, for example, in tap water, for up to several weeks, and can even withstand short boiling. Most often, this type of meningitis affects children of preschool and school age. The acute period of this disease lasts 3-5 days, and approximately 2 weeks pass before complete recovery occurs. In many children, the signs of meningitis are not clearly expressed, which causes an incorrect diagnosis. But despite this, the prognosis regarding the consequences of the disease and recovery with serous meningitis in children is more favorable.
There are a number of signs of meningitis in children, they are called meningeal syndrome. Cases when signs of meningitis appear all at once in children, especially in children, are not very common.
Main signs of meningitis in children
- Strong headache. (May be aggravated by exposure to light and sound)
- Vomit
- Lethargy. In almost all cases, the child simply lies flat
- Heat. (Practically not affected by conventional antipyretics)
- Muscle stiffness. Try with the child lying on his back to press his chin to his chest. If muscle rigidity is observed, this is very difficult to do, and more often than not, simply impossible.
- Sick children try to lie on their side with their legs tucked in and their head thrown back.
- In babies under one year of age, the fontanel may swell.
All of the listed signs of meningitis in children are indirect and serve only to make a preliminary diagnosis. The final diagnosis, and accordingly treatment, is determined only by the results of a spinal puncture. Unfortunately, this far from unpleasant procedure is the only accurate method for diagnosing this disease. When serous meningitis occurs in children, doctors usually give a favorable prognosis, except in special cases. The child is placed in a hospital for treatment, where he spends 2-3 weeks under the supervision of doctors. Subsequently, a child who has had serous meningitis is registered with a neurologist. The most important condition for correct, complete treatment with subsequent recovery is a correct and timely diagnosis.
When a spinal puncture is taken from a child with meningitis, the cerebrospinal fluid is milky-colored and flows out under pressure. But, despite the fact that the procedure is somewhat painful, after it the child immediately feels better, the headache practically goes away, and the temperature gradually returns to normal.
Meningitis is a dangerous disease with its consequences. If you do not seek medical help in time, the consequences of serous meningitis can be:
- Hearing loss (partial or complete)
- Loss of vision
- Speech apparatus disorders
- Children may experience mental retardation.
In particularly severe cases, coma or death
Prevention
During outbreaks of serous meningitis, it is not advisable for adolescents and young children to swim in open water.
You should always drink specially purified or boiled water, observe personal hygiene rules, wash your hands thoroughly with soap after using the toilet and before eating. It is also necessary to wash vegetables and fruits before eating, and if possible, pour boiling water over them. It is worth paying attention to any viral disease in children: acute respiratory viral infection, influenza, chickenpox, measles, mumps. The child’s contact with rodents and ticks should be minimized as much as possible, since they are considered carriers of viruses. To prevent measles, mumps, and rubella, infectious disease specialists recommend routine vaccinations for children. Meningitis caused by the influenza virus is prevented by seasonal specific vaccination.
If a viral infection proceeds atypically, the temperature does not decrease when taking therapeutic doses of antipyretic drugs, vomiting occurs, which does not bring relief, call an ambulance and call the Yusupov Hospital. The neurology clinic admits patients with meningeal symptoms 24 hours a day, 7 days a week. Doctors will determine the cause of meningitis and provide adequate treatment for the disease.
Make an appointment
Symptoms
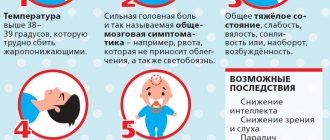
When the incubation period ends, serous meningitis manifests itself with sharp and obvious signs, which are collectively called meningeal syndrome.
A sick child exhibits several symptoms from this list:
- Fever. An indispensable symptom of serous meningitis, occurring in two waves. First, the temperature rises to 39.5-40 degrees and usually lasts for about three days. Then it subsides and returns again in a day or two. In mild cases, the temperature may return in a “truncated” version – 37-38 degrees.
- Severe headache. It starts from the temples and smoothly moves to the back of the head. Bright light and noise increase pain.
- A characteristic symptom of childhood serous meningitis is limb cramps.
- Lack of appetite, nausea, vomiting (without relief), diarrhea, abdominal pain.
- Intoxication, which entails joint pain, general weakness, moodiness and irritability of the child.
- In children, meningitis is often accompanied by standard symptoms of respiratory diseases - runny nose and sore throat. Therefore, parents sometimes mistake it for acute respiratory infections and do not sound the alarm.
- Sick children from three years of age try to take a characteristic position: lying on their side, pressing their hands to their chest and knees to their stomach. The head is thrown back towards the back.
- The acute form of meningitis may be accompanied by impaired motor functions (partial paralysis and paresis).
- Double vision and strabismus are another symptom of the so-called reactive meningitis, which develops over a few hours.
- An attentive parent may notice increased tension in the neck muscles.
- Disorders of consciousness: from stupor and absent-mindedness to coma (in advanced acute form).
These signs can manifest themselves to a greater or lesser extent, singly, in groups or complexly.
For an accurate diagnosis, we check for the presence of certain types of meningeal syndromes:
- Kernig syndrome, when a child cannot straighten a leg bent at an angle of 90 degrees.
- Brudzinski syndrome is a reflex flexion of one leg while bending the other (or flexion of the legs simultaneously with flexion of the head).
- Lesage syndrome (for infants): when you hold a baby by the armpits, he bends his legs and pulls them towards his stomach. Swelling of the fontanelle is also observed.
- Mondonesi syndrome is a severe headache with light pressure on the eyeballs covered by the eyelids.
Some of the symptoms of serous meningitis are similar to those of the meningeal form of tick-borne encephalitis. Because this parasite is active during the summer (as are meningitis outbreaks), the diseases can be confused.