Homeostasis of the cerebrospinal fluid system and, in particular, cerebrospinal fluid is maintained by cellular systems that form appropriate barriers.
The blood-brain barrier ( BBB ) is identified with the endothelial cells of the brain capillaries, and the blood-cerebrospinal fluid barrier ( HLB ) is identified with the epithelial cells of the choroid plexus and arachnoid membranes. Many authors prefer the term “blood-brain barrier”, including the blood-cerebrospinal fluid barrier.
Using the concept of “barrier” always requires clarification of the metabolic composition (water, electrolytes, micromolecules, amino acids, etc.).
What is the BBB?
One of the most interesting and mysterious histohematic barriers is the blood-brain barrier, or the barrier between capillary blood and neurons of the central nervous system. In modern, informational language, there is a completely “secure connection” between the capillaries and the substance of the brain.
The meaning of the blood-brain barrier (abbreviation - BBB) is that neurons do not come into direct contact with the capillary network, but interact with the supplying capillaries through “intermediaries”. These mediators are astrocytes, or neuroglial cells.
Neuroglia is an auxiliary tissue of the central nervous system that performs many functions, such as supporting, supporting neurons, and trophic, nourishing them. In this case, astrocytes directly take from the capillary everything that the neurons need and transfer it to them. At the same time, they control that harmful and foreign substances do not enter the brain.
Thus, not only various toxins, but also many drugs do not pass through the blood-brain barrier, and this is the subject of research in modern medicine, since every day the number of drugs that are registered for the treatment of brain diseases, as well as antibacterial and antiviral drugs, is increasing .
A little history
The famous physician and microbiologist, Paul Ehrlich, became a world celebrity thanks to the invention of salvarsan, or drug No. 606, which became the first, albeit toxic, but effective drug for the treatment of chronic syphilis. This medicine contained arsenic.
But Ehrlich also experimented a lot with dyes. He was sure that just as the dye sticks tightly to fabric (indigo, purple, carmine), it will stick to a pathogenic microorganism, as soon as such a substance is found. Of course, it must not only be firmly fixed to the microbial cell, but also be lethal to microbes. Undoubtedly, the fact that he married the daughter of a famous and wealthy textile manufacturer “added fuel to the fire.”
And Ehrlich began experimenting with various and very poisonous dyes: aniline and trypan.
By dissecting laboratory animals, he was convinced that the dye penetrated into all organs and tissues, but was not able to diffuse (penetrate) into the brain, which remained pale.
At first, his conclusions were incorrect: he assumed that the dye simply did not stain the brain because it contained a lot of fat, and it repelled the dye.
And then the discoveries preceding the discovery of the blood-brain barrier rained down as if from a cornucopia, and the idea itself gradually began to take shape in the minds of scientists. The following experiments were of greatest importance :
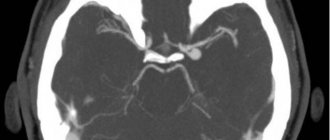
- if the dye is injected intravenously, the maximum that it can stain is the choroidal choroid plexuses of the ventricles of the brain. Then “the path is closed” to him;
- if the dye was forcibly injected into the cerebrospinal fluid by performing a lumbar puncture, the brain was stained. However, the dye did not get “out” from the cerebrospinal fluid, and the remaining tissues remained colorless.
After this, it was completely logical to assume that cerebrospinal fluid is a liquid that is located “on the other side” of the barrier, the main task of which is to protect the central nervous system.
The term BBB first appeared in 1900, one hundred and sixteen years ago. In the English-language medical literature it is called the “blood-brain barrier”, and in Russian the name has taken root in the form of the “blood-brain barrier”.
Subsequently, this phenomenon was studied in sufficient detail. Before the Second World War, evidence appeared that there is a blood-brain and blood-CSF barrier, and there is also a hematoneural variant, which is not in the central nervous system, but is located in the peripheral nerves.
History of the study of the blood-brain barrier
Paul Ehrlich
The study of the BBB began with the work of Ehrlich, who in 1885 injected a dye into a vein and did not observe staining of brain tissue. Then in 1909, Goldman observed the appearance of a dye (trypan blue) after intrathecal administration. Stern and Cautier coined the terms "blood-brain barrier" and "blood-CSF barrier" in 1921. Recently, a large number of works have been devoted to this problem. Fichman in 1980 gives morphological, physiological and biochemical characteristics of the BBB.
Blood-brain barrier - characteristics according to Fishman
- Morphological characteristics: The presence of healthy contacts between capillary endothelial cells.
- The presence of healthy contacts between cells and arachnoid membranes.
- Glial processes surrounding capillaries.
- A small number of pinocytotic vesicles in endothelial cells.
- Numerous mitochondria in endothelial cells.
- Physiological and biochemical characteristics:
Characteristics of endothelial cell permeability: the penetration of macromolecules and polar (lipid-insoluble) substances is limited, while the penetration of lipid-soluble substances is relatively unlimited.
- Differences in osmotic pressure are observed only for a short time, that is, the osmotic pressure of the brain and cerebrospinal fluid varies directly with changes in plasma osmotic pressure.
- There is two-way active transport through membranes and endothelial cells for ions, organic acids, alkalis, which stabilize the composition of the cerebrospinal fluid and extracellular brain fluid.
Structure and functions of the barrier
Our life depends on the uninterrupted operation of the blood-brain barrier. After all, our brain consumes a fifth of the total amount of oxygen and glucose, and at the same time its weight is not 20% of the total body weight, but about 2%, that is, the brain’s consumption of nutrients and oxygen is 10 times higher than the arithmetic average.
Unlike, for example, liver cells, the brain works only “on oxygen,” and aerobic glycolysis is the only possible option for the existence of all neurons without exception . If the supply of neurons stops within 10-12 seconds, the person loses consciousness, and after blood circulation stops, being in a state of clinical death, the chances of complete restoration of brain function exist only for 5-6 minutes.
This time increases with strong cooling of the body, but at normal body temperature, the final death of the brain occurs after 8-10 minutes, so only intense activity of the BBB allows us to be “in shape.”
It is known that many neurological diseases develop only due to the fact that the permeability of the blood-brain barrier is impaired, in the direction of its increase.
We will not go into detail about the histology and biochemistry of the structures that make up the barrier. Let us only note that the structure of the blood-brain barrier includes a special structure of capillaries. The following features are known that lead to the appearance of a barrier:
- tight junctions between endothelial cells lining the capillaries from the inside.
In other organs and tissues, the capillary endothelium is made “carelessly”, and there are large gaps between the cells through which there is a free exchange of tissue fluid with the perivascular space. Where the capillaries form the blood-brain barrier, the endothelial cells are located very tightly, and the tightness is not broken;
- energy stations - mitochondria in capillaries exceed the physiological need for those in other places, since the blood-brain barrier requires large amounts of energy;
- the height of endothelial cells is significantly lower than in vessels of other localizations, and the number of transport enzymes in the cell cytoplasm is much higher. This allows us to assign a large role to transmembrane cytoplasmic transport;
- the vascular endothelium in its depth contains a dense, skeletal-forming basement membrane, to which the processes of astrocytes are externally adjacent;
In addition to the characteristics of the endothelium, outside the capillaries there are special auxiliary cells - pericytes. What is pericyte? This is a cell that can regulate the lumen of the capillary from the outside, and, if necessary, can have the functions of a macrophage to capture and destroy harmful cells.
Therefore, before reaching neurons, we can note two lines of defense of the blood-brain barrier : the first is tight junctions of endothelial cells and active transport, and the second is macrophage activity of pericytes.
Further, the blood-brain barrier includes a large number of astrocytes, which make up the largest mass of this histohematic barrier. These are small cells that surround neurons and, by definition of their role, can do “almost everything.”
They constantly exchange substances with the endothelium, control the safety of tight junctions, the activity of pericytes and the lumen of capillaries. In addition, the brain needs cholesterol, but it cannot penetrate from the blood into the cerebrospinal fluid or pass through the blood-brain barrier. Therefore, astrocytes take over its synthesis, in addition to the main functions.
By the way, one of the factors in the pathogenesis of multiple sclerosis is impaired myelination of dendrites and axons. And for the formation of myelin, cholesterol is needed. Therefore, the role of BBB dysfunction in the development of demyelinating diseases is established and has recently been studied.
Where there are no barriers
Are there places in the central nervous system where the blood-brain barrier does not exist? It would seem impossible: so much effort has been put into creating several levels of protection from external harmful substances. But it turns out that in some places the BBB does not constitute a single “wall” of protection, but there are holes in it. They are needed for those substances that are produced by the brain and sent to the periphery as commands: these are pituitary hormones. Therefore, there are free areas, just in the zone of the pituitary gland and epiphysis. They exist to allow hormones and neurotransmitters to pass freely into the blood.
There is another zone free from the BBB, which is located in the area of the rhomboid fossa or the bottom of the 4th ventricle of the brain. The vomiting center is located there. It is known that vomiting can occur not only due to mechanical irritation of the back wall of the pharynx, but also in the presence of toxins that have entered the blood . Therefore, it is in this area that there are special neurons that constantly “monitor” the quality of the blood for the presence of harmful substances.
As soon as their concentration reaches a certain value, these neurons are activated, causing a feeling of nausea and then vomiting. To be fair, it must be said that vomiting is not always associated with the concentration of harmful substances. Sometimes, with a significant increase in intracranial pressure (with hydrocephalus, meningitis), the vomiting center is activated due to direct excess pressure with the development of intracranial hypertension syndrome. Therefore, so-called central or cerebral vomiting develops, which can occur suddenly, and without any signs of nausea.
Blood-brain barrier permeability
The blood-brain barrier is not equally permeable to all types of molecules . This has been proven with intravenous administration of the metalloenzyme horseradish peroxidase (M 43000), sucrose (M 360), insulin (M 5000) and albumin (M 69000). Intercellular sealed contacts do not allow horseradish peroxidase to pass through. The permeability of the substances listed above is almost inversely proportional to their molecular weight. The relatively high content of albumin compared to gamma globulin in the cerebrospinal fluid can be explained by the action of diffusion and vesicular transport. If these proteins are transported only by vesicular transport, then the mass of the molecule should not matter. Therefore, Rappoport admits the existence of two types of transport of protein molecules:
- pinocytosis for 25 nm molecules;
- diffusion and ultrafiltration through cellular pores for molecules measuring 11 nm, that is, small molecular proteins.
Thus, the permeability of the plasmatic substance into the cerebrospinal fluid depends on:
- the above-listed features of the BBB according to Fishman;
- lipid solubility, that is, whether the molecule is polar or not;
- ionization of the substance;
- molecular weight of the molecule;
- hydrodynamic radius of the molecule (Stokes-Enstein radius);
- ability to form complexes with other proteins, glycoproteins, lipids, inorganic substances, etc.;
- plasma concentration and plasma liquor gradient.
The low concentration of proteins in the cerebrospinal fluid is due to the property of the blood-brain barrier not to allow certain macromolecules to pass through. Thus, the BBB acts like a sieve in relation to proteins. However, the concentration of some proteins (prealbumin, transferrin, etc.) is higher than what would be expected, taking into account the mass of the molecules and plasma concentration.
The blood-brain barrier reflects the equilibration time of individual connections between the two fluids being compared: blood and cerebrospinal fluid. Alcohol and water freely penetrate the BBB, 97 and 93%, respectively. Carbon dioxide and oxygen, due to their good solubility in lipids, quickly penetrate the blood-brain barrier, while water-soluble polar compounds (for example, bicarbonate ions) have difficulty passing through it if there are no transport systems special for them. The combination of some calcium and magnesium ions with plasma albumin explains why only ionized compounds penetrate into the cerebrospinal fluid and the penetration of protein-bound fractions is significantly limited.
The state of the blood-brain barrier is important for the penetration and retention of a given drug. Many factors (degree of ionization, pH of the medium, size and spatial configuration of molecules, etc.) largely determine its permeability. Lipid-soluble ether, chloroform, and alcohol quickly cross the BBB, whereas ionized polar drugs do not penetrate nearly as much. Drugs that are acids or bases are found in plasma in ionized and non-ionized forms in varying proportions. The percentage of each of these forms depends on the pH of the blood and the dissociation constant of the drug. At a blood pH of 7.40 and a cerebrospinal fluid pH of 7.32, the blood-brain barrier easily allows weak alkalis to pass through. A very high concentration of the latter in the liquor increases the content of weak acids in the blood. For example, penicillin penetrates poorly into the cerebrospinal fluid even at high therapeutic doses due to poor lipid solubility. After combining with plasma albumin, penicillin is actively transported through the plexuses. This is also true to a certain extent for methotrexate, long-acting barbiturates and other drugs.
In conclusion, the blood-brain barrier (BBB) and cerebrospinal fluid are a system that maintains homeostasis in the central nervous system. Facilitates the penetration of necessary substances into it, and delays toxins of unnecessary metabolites.