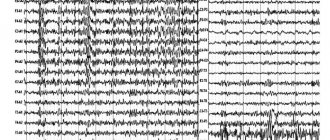
Electroencephalogram of the brain
The research in question is a literal recording of the activity (namely, electrical) of certain brain structures. The results of the electroencephalogram are recorded on paper specially designed for this purpose using electrodes. The latter are applied to the patient's head in a certain order. Their task is to record the activity of individual parts of the brain. Thus, the electroencephalogram of the brain is a record of its functional activity. The study can be carried out for any patient, regardless of his age. What does the EEG show? It helps determine the level of brain activity and identify various disorders of the central nervous system, including meningitis, polio, encephalitis and others. It also becomes possible to find the source of damage and assess its extent.
When performing an electroencephalogram, the following tests are usually necessary:
- Blinking of varying speeds and intensity.
- Exposure of the patient's completely closed eyes to periodic bright flashes of light (so-called photostimulation).
- Deep breathing (rarely inhaling and exhaling) for a period of three to five minutes (hyperventilation).
The tests listed above are carried out for both children and adults. Neither diagnosis nor age affects the testing composition.
Additional studies that the doctor conducts, depending on certain factors, are the following:
- sleep deprivation for a certain period of time;
- passing a series of psychological tests;
- clenching the palm into a fist;
- monitoring the patient throughout the entire period of night sleep;
- taking certain medications;
- the patient is in the dark for about forty minutes.
Clinical picture
Story
The first mention of depression called “melancholy” (from the Greek μελανχολία - black bile) is found in Hippocrates 24 centuries ago. At the end of the 19th century, Emil Kraepelin created a new nosological system for classifying mental disorders, in which the term “involutional melancholia” was introduced. Looking back, we see great variations in classification systems, from descriptive strategies in Kraepelin to interpretive approaches such as Freud's, who viewed depression as a manifestation of underlying fear or loss. In most Western countries, Kraepelin's descriptive methods are more popular.
Symptoms
Major depression is a disorder of the emotional system characterized by a triad of symptoms:
- low or depressed mood;
- anhedonia (loss of interest and pleasure in any activity);
- low energy levels or fatigue.
Other symptoms include sleep and psychomotor disturbances, pessimism, guilt, low self-esteem, suicidal thoughts, appetite and weight problems. The prevalence of depression is high worldwide, affecting approximately 7–18% of the population at least once in their lifetime before age 40. The disease is more common in women—the female/male ratio can reach 5:2. Depression is characterized by a relapsing course; periods of developed symptoms alternate with periods of remission. Because suicide is a common consequence of this disease, depression is one of the 10 leading causes of death worldwide.
Types of depression
According to generally accepted views, the symptomatology of depression is based on more than one structure, and, depending on the entities involved, several types of depression are distinguished. PET and fMRI studies have revealed heterogeneity in brain structures that exhibit dysfunction in this disease. This heterogeneity is reflected in the diversity of symptoms, variability in course, and highly individualized response to treatment. The heterogeneity of major depression allows most experts to view the disorder not as a disease but as a syndrome, suggesting that different neural circuits are involved in the occurrence of its symptoms.
Heredity
Depression is a highly heritable disease with a genetic risk of 40-50%. However, specific genes underlying this disorder have not yet been identified. The other 60-50% risk is also not well understood. Presumably, non-genetic risk factors may include mental trauma at an early age, emotional stress, somatic diseases, and even viral infections.
The need for an objective diagnostic system
A key diagnostic problem is that the current classification system is based only on subjective descriptions of symptoms. This detailed phenomenology includes descriptions of multiple clinical subtypes, but does not identify the biological features that distinguish one subtype from another. The distinction between depression and ordinary sadness is based on the persistence of depressive symptoms and the resulting disability. Because none of the symptoms of depression are of the same quality as the experiences each of us sometimes experiences in life, depression is often unrecognized, misdiagnosed, and sometimes unnecessarily overdiagnosed. A method for objectively diagnosing depression is needed.
What does an electroencephalogram show?
What is this examination? To find out the answer, it is important to understand in detail what the EEG shows. It demonstrates the current functional state of certain structures that make up the brain. It is carried out in a variety of patient conditions, such as wakefulness, active physical work, sleep, active mental work, and so on. An electroencephalogram is an extremely safe research method, painless, simple, and one that does not require serious intervention in the functioning of the body. It allows you to accurately determine the location of cysts, tumors, mechanical damage to brain tissue, and diagnose vascular diseases, epilepsy, inflammatory diseases of the brain and its degenerative lesions.
Types of human brain activity recorded during EEG recording
The main types of activity that are recorded during the procedure and subsequently subjected to interpretation and further study are wave frequency, amplitude and phase.
Frequency
The indicator is estimated by the number of wave oscillations per second, recorded in numbers, and expressed in a unit of measurement - hertz (Hz). The description indicates the average frequency of the activity being studied. As a rule, 4-5 recording sections with a duration of 1 s are taken, and the number of waves in each time interval is calculated.
Amplitude
This indicator is the range of wave oscillations of the eclectic potential. It is measured by the distance between the peaks of waves in opposite phases and is expressed in microvolts (µV). A calibration signal is used to measure the amplitude. If, for example, a calibration signal at a voltage of 50 µV is determined on a record with a height of 10 mm, then 1 mm will correspond to 5 µV. In deciphering the results, interpretations are given to the most common meanings, completely excluding rare ones.
Phase
The value of this indicator evaluates the current state of the process and determines its vector changes. On the electroencephalogram, some phenomena are assessed by the number of phases they contain. Oscillations are divided into monophasic, biphasic and polyphasic (containing more than two phases).
Rhythms of brain activity
The concept of “rhythm” in the electroencephalogram is considered to be a type of electrical activity related to a certain state of the brain, coordinated by appropriate mechanisms. When deciphering the EEG rhythm indicators of the brain, its frequency corresponding to the state of the brain region, amplitude, and its characteristic changes during functional changes in activity are entered.
Characteristics of brain rhythms depend on whether the subject is awake or asleep
Electroencephalogram rhythms
The examination in question allows us to evaluate the following types of brain rhythms:
- alpha;
- theta rhythm;
- beta;
- delta.
Each of them has certain characteristics and help assess different types of brain activity.
- The normal frequency of the alpha rhythm is in the range from 8 to 14 Hz. This should be taken into account when determining pathologies. The EEG alpha rhythm in question is recorded when the patient is awake, but his eyes are closed. As a rule, this indicator is regular. It is most quickly registered in the area of the crown and back of the head. In the presence of any motor stimuli it stops.
- The frequency of the beta rhythm ranges from 13 to 30 Hz. As a rule, it is registered above the frontal lobes. Characterizes the state of depression, anxiety, anxiety. It also reflects the use of sedatives.
- Normally, the theta rhythm has an amplitude from 25 to 35 μV, and a frequency from 4 to 7 Hz. Such indicators reflect the state of a person when he is in a state of natural sleep. For the child, the rhythm in question is prevalent.
- The delta rhythm in most cases demonstrates the state of natural sleep, but it can also be recorded to a limited extent during wakefulness. Normal frequency is from 0.5 to 3 Hz. The normal value of the rhythm amplitude does not exceed 40 μV. Deviations from the specified values indicate the presence of pathologies and impaired functioning of the brain. By the location of the appearance of this type of rhythm, one can determine exactly where dangerous changes occur. If it is noticeable in all areas of the brain, this indicates a violation of consciousness and that systemic damage to the structures of the central nervous system is developing. This is often caused by liver dysfunction.
Other indicators in the conclusions
How to learn to independently interpret expert opinions? Decoding of EEG indicators is presented in the table:
| Index | Description |
| Dysfunction of midbrain structures | Moderate disturbance of neuronal activity, characteristic of healthy people. Signals dysfunction after stress, etc. Requires symptomatic treatment. |
| Interhemispheric asymmetry | A functional disorder that does not always indicate pathology. It is necessary to organize additional examination by a neurologist. |
| Diffuse alpha rhythm disorganization | The disorganized type activates the diencephalic-stem structures of the brain. A variant of the norm, provided that the patient has no complaints. |
| Center of pathological activity | Increased activity in the area under study, signaling the onset of epilepsy or predisposition to seizures. |
| Irritation of brain structures | Associated with circulatory disorders of various etiologies (trauma, increased intracranial pressure, atherosclerosis, etc.). |
| Paroxysms | They talk about decreased inhibition and increased excitation, often accompanied by migraines and headaches. Possible tendency to epilepsy. |
| Reducing the threshold for seizure activity | An indirect sign of a predisposition to seizures. This is also indicated by paroxysmal brain activity, increased synchronization, pathological activity of midline structures, and changes in electrical potentials. |
| Epileptiform activity | Epileptic activity and increased susceptibility to seizures. |
| Increased tone of synchronizing structures and moderate dysrhythmia | They do not apply to severe disorders and pathologies. Requires symptomatic treatment. |
| Signs of neurophysiological immaturity | In children they talk about delayed psychomotor development, physiology, and deprivation. |
| Residual organic lesions with increased disorganization during tests, paroxysms in all parts of the brain | These bad signs are accompanied by severe headaches, attention deficit hyperactivity disorder in a child, and increased intracranial pressure. |
| Brain activity disorder | Occurs after injuries, manifested by loss of consciousness and dizziness. |
| Organic changes in structures in children | A consequence of infections, for example, cytomegalovirus or toxoplasmosis, or oxygen starvation during childbirth. They require complex diagnostics and therapy. |
| Regulatory changes | Fixed for hypertension. |
| Presence of active discharges in any departments | In response to physical activity, visual impairment, hearing loss, and loss of consciousness develop. Loads must be limited. In tumors, slow-wave theta and delta activity appears. |
| Desynchronous type, hypersynchronous rhythm, flat EEG curve | The flat version is characteristic of cerebrovascular diseases. The degree of disturbance depends on how much the rhythm hypersynchronizes or desynchronizes. |
| Slowing down the alpha rhythm | May accompany Parkinson's disease, Alzheimer's disease, post-infarction dementia, groups of diseases in which the brain can demyelinate. |
We recommend reading: Midlife crisis in women - advice from a psychologist
Online consultations with medical experts help people understand how certain clinically significant indicators can be deciphered.
Treatment
Cognitive behavioral therapy
Cognitive behavioral therapy is a psychological treatment that dates back to the era of Freud. Today, psychotherapy is usually recommended as a treatment for mild forms of depression or as an adjunct to drug therapy for more severe forms of the disease. This type of treatment is based on the idea that depressive symptoms are based on destructive beliefs and thoughts that arise early in development. Such patterns are activated by situations or events that have special meaning for the individual. Thus, cognitive behavioral therapy focuses primarily on identifying negative automatic patterns and suppressing them. Several studies have demonstrated the superiority of cognitive behavioral therapy over other psychological techniques and placebos.
ECG and psychosurgery
Currently used physical treatments for depression date back to 1937, beginning with the introduction of electroconvulsive therapy, which, despite public and professional concern, remains the most effective treatment for depression. The main objections to the use of ECT are related to the cognitive impairment it provokes. However, a recent meta-analysis of ECT performed in the UK and published in the Lancet in 2003 found that the damage after ECT consisted predominantly of short-term anterograde and retrograde amnesia.
In the 1940s and 1950s, psychosurgery, more precisely frontal lobotomy, began to be used to treat depression. Later, in the 1960s, the first drugs were discovered that could reduce the symptoms of major depression. The invention of antidepressants and the study of their pharmacology led to fundamental changes in this area. In addition, psychosurgery, which entails massive destruction of brain tissue, has been replaced by a modern stereotactic method, which allows precise insertion of electrodes and is a tool for deep brain stimulation. A group of researchers from the University of Toronto, Canada (Maybeig et al., 2005), used electrodes inserted into the white matter lateral to the subgenual portion of the anterior cingulate gyrus in the treatment of six patients with severe, treatment-resistant depression. The authors report strikingly durable disease remission in four of six patients. PET scans showed a decrease in the initially elevated metabolism in the subgenual region in these patients compared to healthy subjects.
Antidepressants
Antidepressants are a heterogeneous group of drugs that increase the content of monoamines in the synaptic cleft. Understanding their pharmacology allowed the formulation of the monoamine hypothesis of depression and expanded the possibilities for the development of new drugs such as selective serotonin reuptake inhibitors.
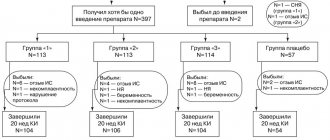
The effectiveness of many known antidepressants is about 60%. At present, it is not possible to confidently predict the clinical effect of individual drugs. Thus, if a patient does not respond to one drug, he is switched to another, usually from a different class, and so on until different classes of drugs have been tested. Since the clinical effect appears after 6-8 weeks, it may take several months to find an effective drug. This process requires a lot of time and money. Moreover, it leads to an increase in the likelihood of suicide, since a partial effect may be manifested in increased psychomotor activity while maintaining depressive symptoms. Finally, despite the trial-and-error approach used in drug treatment for depression, many patients remain resistant to all known drugs.
The lack of effectiveness of pharmacotherapy has prompted medical science to search for alternative treatment methods, such as EEG biofeedback, transcranial micropolarization, deep brain stimulation, and transcranial magnetic stimulation. All these approaches (along with traditional methods) require reliable objective assessment of the disease for diagnosis and monitoring of the treatment process.
In table presents most of the currently available treatments for major depression.
| Type of intervention | Mechanism of action |
| Tricyclic antidepressants | Suppression of serotonin and norepinephrine reuptake |
| Monoamine oxidase inhibitors (MAOIs) | Inhibition of MAOA and associated inhibition of biogenic amine reuptake |
| Lithium | Unknown |
| Atypical antidepressants | Unknown |
| Selective serotonin reuptake inhibitors (SSRIs) | Selective inhibition of serotonin reuptake |
| Norepinephrine reuptake inhibitors (NSRIs) | Selective inhibition of norepinephrine reuptake |
| Serotonin and norepinephrine reuptake inhibitors (SNRIs) | Suppression of serotonin and norepinephrine reuptake |
| Electroconvulsive therapy | Global electrical activation of neural networks with intense release of various neurotransmitters |
| Transcranial magnetic stimulation | Aftereffect of local electromagnetic activation of neural networks |
| Deep brain stimulation | Constant stimulation of the cingulate cortex in the subgenual region |
| Cognitive behavioral therapy | Unknown |
| Intrapersonal therapy | Unknown |
TMS
Transcranial magnetic stimulation was first used as a potential treatment for depression in the late 1990s. However, the initial enthusiasm has given way to a more moderate assessment of the method today. A meta-analysis of all available data conducted in 2006 (Ebmeier et al., 2006) indicated a trend towards a significant decrease in effect sizes from 1996 to 2004.
EEG biofeedback
EEG biofeedback in the treatment of depression is based mainly on Davidson's theory of the asymmetric distribution of alpha activity in the lateral frontal regions. Based on this theory, Rosenfeld developed an EEG biofeedback protocol to normalize abnormal asymmetry in depression. The so-called ALAY protocol (created for alpha asymmetry) uses the ratio (F4 - F3)/(F3 + F4) as a feedback parameter. Preliminary results using this protocol in some cases are encouraging, but control studies have not yet been conducted. For example, Bayer and his colleagues, having studied a 1-5 year follow-up of patients who used the ALAY protocol, found that changes in the clinical picture after training remained persistent and that frontal alpha asymmetry not only changed at the end of treatment, but also remained in the opposite direction. physiological level over a long period of observation. Unfortunately, there have been no studies using placebo control and double-blind methods, as in proving the effectiveness of pharmacological treatment.
Alpha rhythm value
Alpha rhythms were recorded using EEG, which were suppressed by beta rhythms. Beta waves only appeared if the patient opened his eyes during the diagnostic process. With the help of EEG, doctors today can also detect disorganization of the alpha rhythm, which is already a pathological condition.
The human brain operates on a relatively small amount of electricity, but this allows it to be the main control center and regulate the functioning of the central nervous system and internal organs. Therefore, he needs regular stimulation of electrical activity, which is important for both children and adults.
Alpha brain activity, which occurs when a person is in a relaxed state, is most interesting to scientists. For example, it is recorded in a state of drowsiness, when the observed person is not yet asleep, but has not woken up, and it cannot be said that the person is alert and has completely recovered from sleep.
When the brain works in alpha mode, a person has the opportunity to receive a huge amount of information. It is customary to distinguish between slow and fast variants of alpha rhythms.
Neuronal model
Monoamine hypothesis of depression
The monoamine hypothesis of depression arose early in the quest to understand the mechanisms of this disorder. According to this hypothesis, depression reflects a deficiency or imbalance of norepinephrine (or serotonin) in the brain. The hypothesis was based on observations showing that some antidepressants increased synaptic concentrations of norepinephrine or serotonin, and that reserpine (a catecholamine depleting drug) could cause symptoms similar to depression.
Medicines that affect catecholamines begin to affect the corresponding neurotransmitter systems no later than an hour after taking the drug, but positive changes may not appear earlier than several weeks after the start of treatment! One theory that attempts to explain this discrepancy points to the slow development of adaptive changes in the functioning of synaptic autoreceptors in the brainstem, resulting in their desensitization. Another hypothesis states that depression is caused by damage to the neuronal circuits of the emotional system, and not by dysfunction of neurotransmitters. Reorganization of these pathologically altered circuits requires long-term modification, as does the involvement of circuits responsible for procedural memory.
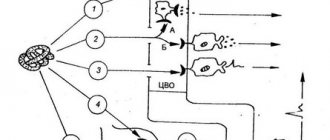
Neural circuits in depressed mood
Fig.2.
Neural Model of Depressed Mood Outputs from the amygdala (At), papillary bodies of the hypothalamus (MB) and hippocampus (Hip) project through the anterior nucleus of the thalamus to the insula, orbitofrontal cortex (OF) and anterior cingulate cortex (ACC). Sad events are likely mapped to the popliteal cingulate gyrus (represented by a dot pattern), such that hypoactivation of this region results in depressed mood.
According to experimental neuroimaging, in depression, which is a multisymptom disorder, both the executive and emotional systems of the brain are involved. In major depression, elements of the emotional system such as the orbitofrontal and medial cortices, the insula, the amygdala, and structures of the hypothalamic-pituitary complex are involved. Elements of the control system include the anterior cingulate cortex and the corresponding basal ganglia-thalamus-cortex loop. Let me describe the circles involved in depressed mood (Figure 2). Remember that this symptom is the most common manifestation of depression and pharmacotherapy is most often aimed at correcting it.
A large body of neuroimaging work shows that sadness and depressed mood are associated with abnormal activation of neurons in the medial prefrontal cortex, including the anterior cingulate and orbitofrontal cortices. These cortical areas receive inputs from the hippocampus, amygdala, and mamillary bodies of the hypothalamus through the anterior nucleus of the thalamus. The activity of these areas is mediated predominantly by serotonergic innervation from the raphe nucleus of the midbrain and partially by noradrenergic innervation from the locus coeruleus. Antidepressants, which reduce symptoms of sadness and depressive mood, affect these neurotransmitter systems and normalize the activity of these areas. Long-term deep brain stimulation of the subgenual part of the anterior cingulate cortex has a similar effect.
In contrast to depressed mood, which is associated with hyperactivity of the medial frontal cortex, executive dysfunction in major depression is likely reflected in hypoactivation of the dorsolateral prefrontal cortex. This hypoactivity may be the result of mutual suppression of the control system and the emotional system. The neuronal basis of this suppression may be provided by lateral inhibitory connections in the striatum. Remember that the localization of the parts of the striatum that receive inputs from the cortical areas of the emotional system differs from the localization of the parts that receive inputs from the control system. As we know, the control system controls a wide range of cognitive operations, including working memory, attention, and social motivation. Thus, cognitive symptoms of depression are associated mainly with the dopaminergic innervation of the control system and may be the target of appropriate drug therapy. Suppression of the control system occurs mainly in the dominant hemisphere and is reflected by alpha asymmetry in the background EEG (more alpha activity in the left hemisphere) and a decrease in the components of cognitive EP associated with the control system.
Positive Impact
When the human brain functions in the alpha activity mode, its state is characterized as calm, the most optimal, so its importance is difficult to overestimate. The human central nervous system has two important mechanisms in its work: self-regulation and self-healing. Due to these functions, brain activity increases and the mental resistance to irritants is supported.
When normal, the alpha rhythm of the brain causes many positive effects:
- There is an improvement in blood supply to the brain structures, therefore the saturation of the organ with useful microelements and oxygen is accelerated.
- There is an increase in the rate of recovery of the human body as a whole, which is important, for example, after suffering serious illnesses.
- Increased energy circulation occurs.
- There is an increase in intuitive mental activity, which allows you to spend less energy on solving assigned problems.
- The brain, working in alpha activity mode, can reprogram consciousness, resolve many psycho-emotional problems and remove the following interference: tension, anxiety, stress, insomnia, etc.
- The manifestations of negative conditions are reduced: childhood traumas, life difficulties.
Ways to stimulate alpha waves
On the EEG, alpha rhythms can be observed only in cases when the human body is completely relaxed. Those observed in this state are distracted from problems, so stress is relieved. A slowdown in mental activity has also been noticed, so the consciousness is “cleared”. This allows you to create new ideas, increases the creativity of mental activity, and gets rid of the creative crisis.
If a person experiences severe and prolonged brain activity for some time, then the normal activity of the organ stops. The solution to this problem is to increase alpha waves and relieve mental stress.
There are many techniques that allow you to have a stimulating effect on alpha waves:
- Sound waves. A simple and accessible technique in all respects, with the help of which alpha activity increases, and the process itself brings a “dose of pleasure” to a person. The technique consists of listening to special music, which consists of stereo sounds.
- Yoga. Long-term yoga exercises, provided the exercises are performed correctly, act as a powerful activator of alpha activity in the brain, which can moderately and not dramatically increase the necessary indicators.
- Meditation. With the help of meditation, you can teach your body to relax automatically, but this will require spending a lot of time going through a huge number of practical sessions.
- Breathing exercises. The method implies that the person will have to constantly maintain deep breathing. This process saturates the brain cells and internal organs with oxygen. If you do breathing exercises systematically so that it becomes a habit, the creation of alpha waves will occur automatically.
- Hot baths. Relaxation almost always occurs after taking a hot bath, which also eliminates fatigue. The production of alpha waves is the main reason for the relaxation of muscle structures.
- Alcohol. Not a recommended method, which, oddly enough, also allows you to activate production and get an increased level of alpha waves. Alcohol is used by many people to relieve stress. Immediately after drinking alcohol, alpha waves begin to form, which allows a person to enter a state of relaxation, detachment from the world and relaxation.
Pathological indicators
To clarify the current meanings of rhythms, electroencephalography is used as the main diagnostic technique. On EEG, the normal alpha wave index is in the range of 80-90%. If such indicators are absent or are below 50 percent, then this characteristic will indicate the presence of pathology.
It has long been proven that in pre-retirement and retirement age the amplitude of alpha activity begins to decrease significantly, which is due to the deterioration of blood supply to the brain and organs as the body ages.
Normal amplitude values during EEG are in the range from 25 to 95 μV. Research conducted in the middle of the 20th century made it possible to derive such a concept as “brain dysrhythmia.” But further research has shown that not in all cases dysrhythmia will indicate the presence of pathology in the observed person. The EEG can also show special types of BEA (bioelectric activity), epileptiformity and diffuse changes.
Abnormal and insufficient alpha activity values are usually detected in certain diseases:
- Epilepsy (various forms of this disease, including those associated with drug use). With this pathology, the patient develops direct or interhemispheric asymmetry in the cerebral hemispheres of the head. Both frequency and amplitude suffer. This may indicate disturbances in interhemispheric integration.
- Oligophrenia. There is an abnormal increase in total alpha wave activity.
- Problems with blood circulation. Pathology of alpha activity almost always develops with circulatory disorders, narrowing or dilation of cerebral vessels. If the severity of the disease is high, then there is a significant decrease in average activity and frequency indicators. Problems are also observed with beta-lactamase activity of bacterial agents.
- Hypertonic disease. This pathology can weaken the rhythm frequency, which is not enough for normal relaxation of the body.
- Inflammatory processes, cysts, tumors on the corpus callosum. Diseases of this type are considered extremely severe, therefore, when they develop, the asymmetry between the left and right hemispheres can be very serious (up to 30%).
To assess the activity of alpha rhythms, EEG is regularly performed in many pathological conditions: dementia (acquired or congenital), VSD, traumatic brain injury. The data obtained will allow us to choose the right treatment for diseases that will correspond to the existing rhythms.
When deciphering the EEG, in some cases the presence of disorganized alpha activity may be noted. Disorganization or complete absence of alpha activity may indicate acquired dementia. Alpha rhythms are also disorganized when psychomotor development is delayed in children.
Possible reasons
Signs of pathological changes in fluctuations of this index in an adult patient are:
- asymmetry of the human brain hemispheres by more than 30%;
- violation of sine wave indicators;
- delta and theta rhythms;
- unstable parameters.
During an EEG study, fluctuations in the forehead area should be clearly visible when the eyes are opened, and should disappear when closed. If this does not happen, then there is a high probability that there is an injury in this place. Clear asymmetry of the hemispheres may be a sign of brain cancer or various lesions as a result of a heart attack or stroke.
These indicators may also indicate changes in the brain as a result of injury. If a malfunction is observed in children, this may be a sign of some kind of mental pathology. It is more difficult to determine fluctuations in children, because a small child cannot close or open his eyes on command.
The violation is a sign of the presence of epileptic brain damage, drug addiction, severe deviations of the organ hemispheres, and hypertension. High fluctuations indicate that the patient may have mental retardation.
What is alpha rhythm depression?
Electroencephalography (EEG) shows the alpha rhythm as a rhythmic wave in the cortex with a frequency range of 8-12 Hz. Unlike other frequencies, this wave has an unusual sinusoidal, smoother shape. From a physiological point of view, this means how inactive the visual system of the brain is; from a psychological point of view, it is a kind of connection between a person’s consciousness and the subconscious.
Alpha rhythm is often associated with inhibited brain activation. The greater the range of fluctuations in the indicator, the less the brain works in the area where it was recorded. The index has clearer indicators when examining the occipital and parietal regions, as well as the posterior wall of the temple. Alpha rhythm depression is the replacement of alpha with beta rhythm.
We recommend reading: Can depression be recognized by blood tests?
The meaning of the alpha rhythm for humans
For a person, the normal functioning of the alpha rhythm is extremely important, because responsible for the following brain actions:
- analysis of information received during the day;
- activation of the parasympathetic nervous system to restore the body's resources;
- normal cerebral circulation;
- stabilization of the limbic system;
- normalization of post-traumatic syndrome due to a stressful situation.
Disruption of the alpha rhythm can lead to alcohol or drug addiction. This disorder also causes excessive eating and bulimia, because... there is a failure in normalizing the basic needs of the body. There is also incomplete depression of the alpha rhythm, which provokes disruptions in the human cardiovascular system. Incomplete depression leads to a large number of negative thoughts and a person becoming fixated on some problems.
What to do?
Now there are a large number of methods for treating the disorder:
- medicinal;
- light therapy;
- psychotherapy.
Biofeedback therapy is quite common and involves constant monitoring of physiological parameters of the body over time. During the treatment course, physiological indicators are adjusted, for example, the functioning of the muscular system, blood circulation, and brain activity. This treatment allows people to cope with fears, panic attacks, and excessive muscle tension.
This method is most often used for headaches, spastic torticollis, stuttering, constantly shaking hands, high blood pressure, impotence caused by a psychological problem, and epilepsy.
Secrets of the alpha rhythm
Sergey Gusev 2020-01-14T19:57:14+03:00 Neurofeedback neurofeedback, brain rhythms
Since we're talking about alpha, perhaps we should talk a little about this rhythm, especially since I have already accumulated a lot of recordings and excerpts that need to be organized, at least in the form of a structured post.
The alpha rhythm is usually associated with meditation, a feeling of inner peace and tranquility. Alpha is also often surrounded by an aura of mysticism and associated with states of enlightenment, healing possibilities, and even the potential to connect to a higher mind. Many different techniques offer ways to increase the alpha rhythm and even methods to achieve constant alpha level. But let's figure out whether these frequencies are always useful, and is it always necessary to increase them?
The alpha rhythm appears as a rhythmic 8-12 Hz wave that has a fairly specific sine wave shape that is much smoother than other frequencies. Physiologically, alpha is associated with inactivity of the brain's visual system. From a mental point of view, alpha is considered to be a bridge between consciousness (beta) and the subconscious (theta). People who cannot produce the alpha rhythm effectively are usually locked on one side or the other of the dividing line between the conscious and the subconscious. Theta processors are often labeled ADHD because they have difficulty concentrating, learning new material, organizing their activities, etc. Beta processors, on the other hand, are often locked away from their feelings and deep-seated memories. The inability to enter the alpha state (the inner observer state) prevents them from being effectively aware of their feelings and emotions.
Alpha rhythm is associated with decreased brain activation. The greater the alpha amplitude in any area of the brain, the less active the brain is in that area. At their core, alpha and beta rhythms are antagonists. Neurons not involved in work can resonate with the thalamus and produce alpha rhythm. And when performing a task, neurons produce beta. They cannot generate both rhythms at the same time.
The alpha rhythm is most pronounced in the occipital, parietal and posterior temporal regions. In some sources, the alpha rhythm in adults is sometimes called the occipital dominant rhythm. In the front part of the head, the amplitude of the alpha rhythm should normally be lower than in the back. High frontal alpha is commonly seen in children, as well as in adults in cases of ADHD, depression and other disorders.
Increasing the alpha level, usually in the parietal and occipital regions, is indicated when its level is insufficient in order to reduce anxiety. Sometimes training to increase occipital alpha is accompanied by training to increase theta, which is called A/T training and is used to achieve deep trance states. For this purpose, single-channel training is usually used in O1, O2, Oz, Pz or P4. Deep trance states are successfully used in neurofeedback to treat post-traumatic syndrome and various types of addictions.
Frequency histogram during training to increase the alpha rhythm using the 4-channel Windowed Squash protocol.
Alpha rhythm blocking.
Normally, the amplitude of the alpha rhythm increases when the eyes are closed and drops significantly (by at least 30%) when the eyes open. This is called alpha blocking. The opposite behavior of the alpha rhythm usually accompanies chronic sleepiness. If there is no change in alpha amplitude when you close your eyes, especially at the back of your head, this may be a sign of one of the following problems:
- Inability to produce alpha with eyes closed. This suggests that neurons are not ready or able to jump off beta processing speeds, even when there are no tasks that require such active activity.
- Inability to block alpha when opening eyes or solving problems. This suggests that the neurons are unable to emerge from their state of inactivity and are actually ignoring attempts to get them to do things.
You can figure out what exactly is happening by looking at the alpha/theta amplitude ratios. If the ratio is low with the eyes closed and normal when the eyes are opened and problems are solved, then this indicates that point 1 occurs. In this case, neurofeedback usually trains an increase in alpha in the parietal leads. If the ratio is normal with eyes closed and high with eyes open or when solving problems, then this suggests point 2. In this case, alpha blocking training with eyes open in the frontal and central parts of the brain is indicated.
The alpha/theta ratio can be disrupted due to a low peak alpha frequency (as seen in children, for example). Therefore, when conducting an assessment, it is worth paying attention to whether there are activities at neighboring frequencies, the amplitude of which is high when the eyes are closed and decreases when the eyes are open.
Alpha rhythm is also suppressed when solving complex tasks, such as reading difficult-to-understand texts. In contrast, children with ADHD often have difficulty focusing due to an inability to effectively suppress the alpha rhythm.
Alpha rhythm asymmetry.
Alpha asymmetry, especially in the frontal lobes, is important for overall mood. Normally, the alpha amplitude in the left hemisphere should be 10-15% lower than in the right (with the only exception - in O1 it can be greater than in O2), which is important for normal mood control. In the case of depression, often the alpha amplitude in the left hemisphere, on the contrary, exceeds the amplitude in the right, so brain training in this case is aimed at restoring the correct asymmetry of the alpha rhythm.
The explanation for this principle is that the left frontal lobe is responsible for positive judgments and uplifting mood, while the right frontal lobe, on the contrary, is responsible for negative judgments and emotional decline. For a normal mood, the negative (right) side should be less active than the positive (left) side. In addition to decreasing alpha, increasing beta in this brain region can also be used to increase activation of the left frontal lobe.
In depression, the standard protocol for neurofeedback is a decrease in alpha in the left hemisphere, as well as a decrease in the level of frontal alpha.
Peak alpha frequency.
The peak frequency of the alpha rhythm in adults should be around 10 Hz. This frequency is due to the signal transit time in the thalamus-cortex-thalamus loop, which is approximately 100 ms. However, with old age, the frequency of the alpha rhythm gradually decreases. Also, a decrease in the alpha rhythm is observed in depression and may be evidence of the presence of certain brain dysfunctions.
But if a significant slowdown in alpha is commonly associated with a decline in cognitive abilities, then a general slowdown in alpha with age may simply indicate that more information processing occurs at the end points of the thalamo-cortical cycle, which introduces additional delay into the cycle and thereby slows down its frequency. Well, since a slowdown in the alpha rhythm is also observed in experienced meditators, in this context this may well indicate the acquisition of higher knowledge and perhaps even wisdom.
We recommend reading: What is chronic fatigue syndrome?
A high alpha frequency in the back of the head often corresponds to better memory performance and better scores on IQ tests, while a high peak frequency in the front may be associated with increased anxiety. However, an alpha peak that differs in only one specific area may indicate the presence of injury there.
Slow and fast alpha rhythm.
The alpha rhythm in neurofeedback is usually divided into slow (8-10 Hz) and fast (10-12 Hz). Fast alpha is usually an occipital resting rhythm. It reflects background memory processes and a state of inactivity without loss of attention. Slow alpha tends to be more prominent in the front and is associated with emotional processing.
A general slowing of alpha can result in all kinds of cognitive problems: semantic memory, working memory, feelings of depression, decreased energy, sleep and learning abilities (related to working memory) are impaired. Also, when alpha slows down, somatic effects often begin to appear.
One way to determine if this problem is present is to look at the ratio between fast (10-12 Hz) alpha and slow (8-10 Hz) alpha. If the ratio of fast alpha to slow alpha is 1 or slightly higher, then this is good. If it is below one, then you may have some of the problems listed above, as well as age-related cognitive decline that occurs in many people after 50. In particular, in senile dementia (senile dementia), the alpha peak is around 8 Hz or even lower. Training to increase peak alpha in neurofeedback is one of the core elements of brain training for older adults.
According to many studies, the best way to reduce slow alpha is to increase fast alpha in the parietal/occipital region. This can be achieved by training to reduce 2-9.5 Hz activity and promote 10-14 Hz activity in P4 or Pz or even in O1 or Oz.
High amplitude alpha.
Too much alpha can be just as problematic as too little, especially if the alpha isn't blocking. In assessment, this can manifest as high alpha/theta ratios, poor blocking, and high levels of slow alpha. If we continue the analogy with the bridge between consciousness and subconsciousness, then low levels of alpha correspond to the absence of this bridge (a person cannot be aware of subconscious processes), and excessively high levels can represent a bridge stuck in an open state. For the latter, alpha is a kind of anesthesia, which also interferes with the awareness of deep feelings, and often leads to the somatization of emotional material.
High amplitude alpha may be the brain's response to emotional trauma that has not been integrated by the brain. In this case, the brain actually uses alpha as an anesthetic to help keep it from becoming aware of it. As a result of elevated alpha levels, a person may be emotionally insensitive. Apparently, this pattern is often chosen by the brain as a way of protecting itself from any stressful events. Most people with fibromyalgia, chronic pain, and chronic fatigue have this pattern, often accompanied by a low alpha peak and alpha predominance at the front of the head.
Long-term experience with meditation can also result in high levels of alpha, especially if it is synchronous. But for the most part, this applies to the back of the head, in which case alpha is effectively blocked when opening the eyes and solving problems.
High levels of slow alpha may relate to long-term marijuana use. High alpha in the temporal lobes, especially if it remains high with the eyes open, can cause impaired memory function and difficulty maintaining emotional stability.
If alpha is particularly high at certain points, both with eyes open and closed, and when solving problems, then this may be a sign of damage to the gray matter due to head trauma. Large alpha spikes in the occipital leads also indicate closed head trauma or a traumatic experience - usually visual - that has been dissociated.
In neurofeedback, decreasing alpha amplitude is usually trained to the left or towards the front - where the brain needs to work faster. In this case, brain training is carried out with open eyes, although with closed eyes can also sometimes be useful. First of all, this type of training is chosen if the alpha/theta ratio with eyes closed is greater than 2.5 in leads P or O, especially if when the eyes are opened the ratio does not become less than 1 or increases again when solving problems.
A.F. Iznak
A brief review presents hypotheses and facts indicating a close connection between depression and metabolic disorders of a number of monoamines, dysfunction of the inhibitory systems of the cortex and diencephalic parts of the brain, desynchronization of biological rhythms, in particular, mechanisms of regulation of the sleep-wake cycle, with hemispheric specialization in the control of positive and negative emotions. These data can be used to develop new methods for refining the diagnosis and optimizing the treatment of depressive disorders.
The paper presents a brief review of the available hypotheses and data suggesting a close relationship between depression and the impairment of some monoamines metabolism, dysfunction of neocortex and diencephalic inhibitory systems, desynchronization of biological rhythms, in particular, the mechanisms of the sleep-wakefulness cycle regulation and functional brain asymmetry. This data may be used for the development of the new diagnostic methods and for optimization of depression therapy.
Emotions play a vital role in the life of animals and humans, providing an integral subjective assessment of external and internal stimuli in terms of their biological significance for the individual and, thereby, participating in the organization of expedient adaptive behavior. Various types of disturbances in the normal functioning of the brain mechanisms of emotions—emotional or affective disorders and, above all, depression—disorganize adaptive behavior and are a severe syndrome in a number of mental illnesses [16].
Anatomical substrate of emotions
It is usually accepted that the anatomical substrate of emotions is the brain structures included in the so-called limbic system: the hippocampus with its pathways, the septum pellucidum, the nuclei of the amygdala complex, the hypothalamus, as well as a number of nuclei lying in the reticular formation of the brainstem, pons and midbrain. This set of structures is often called the limbic-reticular complex. In addition, the structures involved in the organization of emotions include the cingulate gyrus, prefrontal, orbital and temporal zones of the cerebral cortex [see. 3]. Thus, taking into account the fact that for the emotional assessment of stimuli it is necessary to first carry out their sensory analysis, including the involvement of memory mechanisms and probabilistic forecasting, almost the entire brain can be considered the morphological substrate of emotions.
Neurochemical basis of depression
The results of numerous multidisciplinary studies in the field of neuroscience indicate that the basis of endogenous mental disorders appears to be disturbances in synaptic transmission, that is, ionic processes occurring at the level of the membranes of nerve cells [see. 6].
According to the monoamine hypothesis, the neurochemical basis of depressive states is the deficiency (depletion) of norepinephrine and serotonin. Two types of depression have been described: one associated with norepinephrine depletion and more responsive to treatment with desipramine or imipramine, and another associated with serotonin deficiency and more successfully treated with amitriptyline [24].
It is assumed that antidepressants exert their therapeutic effects by potentiating (facilitating) synaptic transmission at noradrenergic and serotonergic synapses. There are two main groups of antidepressants, some of them are inhibitors of monoamine oxidase (MAO - type A), an enzyme that ensures the metabolism of these monoamines in the synaptic cleft, and others inhibit their reuptake by presynaptic structures [see. 28].
Norepinephrine and serotonin are neither inhibitory nor excitatory neurotransmitters in the classical sense - rather, they have a neuromodulatory effect on the integrative functions of central neurons, reducing their reactivity to weak excitatory and inhibitory influences and enhancing responses to strong (suprathreshold) excitatory signals, due to the participation in the systems of GABAergic direct and recurrent postsynaptic and presynaptic inhibition, thereby increasing the signal-to-noise ratio in the nervous network [39].
The neuromodulatory interaction of monoamines and the GABAergic system in depression is complex and bilateral.
Depression is often associated with anxiety, and most both antidepressants and tranquilizers have a “dual” effect, reducing both anxiety and depression. Therefore, in the clinic of depressive conditions, complex treatment of depression with a combination of these drugs is often used, especially if anxiety is strongly expressed in depression of a psychotic level [24] or in cases of “masked” (somatized) depression [22].
The most common tranquilizers are benzodiazepines, which increase the effectiveness of GABAergic inhibitory synapses [27]. The wide distribution of benzodiazepine receptors in various brain structures, with their particularly high concentration in the hippocampus, argues in favor of the hypothesis of their antidepressant effect through the GABAergic mechanism. Interestingly, in therapeutic doses, benzodiazepines do not have a direct effect on non-autonomic functions; however, they have been shown to modulate the reactions of the autonomic system to external stimuli, for example, they reduce the response to an increase in the concentration of norepinephrine and, even to a greater extent, epinephrine in the blood plasma in response to painful stimulation [28].
Possible neurophysiological mechanisms of depression
Despite the impressive successes of cellular and molecular neurobiology, which led, in particular, to the creation of a number of psychotropic drugs (for example, highly specific selective serotonin and norepinephrine reuptake inhibitors), without additional information it is quite difficult to imagine how ionic processes on cell membranes (and not only neurons, but even cellular elements of peripheral blood, for example, platelets) can influence the behavior and mental state of a person.
A kind of “bridge” or “missing link” for such an understanding may be modern neurophysiological ideas about the structure and function of the nervous networks of the brain that process information.
According to these ideas [see 4, 5, 21], the main organizing role in the integrative activity of the brain is played by inhibition processes, providing spatial and temporal contrast, highlighting a useful signal against a background of noise, distinguishing, analyzing and synthesizing external and internal stimuli, organizing motor commands and regulatory sendings. Inhibitory systems ensure the interaction of the two halves of the brain (including the right and left hemispheres of the neocortex), cortical-subcortical relationships (neocortex with the basal ganglia, limbic-reticular structures), serve reciprocal inhibition at the level of the hypothalamic centers for the regulation of autonomic functions (sympathetic and parasympathetic systems ).
At the same time, the main disorders of synaptic transmission identified in affective mental pathology primarily relate to inhibitory GABAergic systems. As a consequence, the normal mode of interaction of neurons in the nerve networks that process sensory (extra- and interoceptive) and intercentral information, as well as the integration of motor and regulatory activity, is disorganized. Moreover, depending on the localization and degree of generalization of functional disorders, various disorders of mental activity arise with corresponding neurological and autonomic correlates.
Another thing is that identifying these disorders and unambiguously comparing biological and clinical data in order to clarify diagnosis and optimize individual therapy is quite difficult, despite the extensive arsenal of modern instrumental methods of biological psychiatry.
Electrophysiological correlates of depression
The electroencephalogram (EEG) reflects the current functional state of the brain with very good temporal resolution and therefore (despite all the limitations and methodological problems) remains an important tool for studying the brain mechanisms of higher brain functions.
Of particular importance is the fact that EEG rhythms, which are the most informative components in assessing the functional state of the brain, are generated by the same neuronal systems of excitation and inhibition that are involved in information processing, with the greatest contribution to the EEG picture being made by the inhibitory systems of the cortex and thalamus [see. 5].
Frequently used autonomic indicators: galvanic skin responses (GSR), electrocutaneous resistance (ECR), heart rate (HR), electromyogram (EMG) and others, allow indirect assessment of the functional state of the central parts of the autonomic nervous system, primarily hypothalamic structures [8 ].
Due to the fact that there are several clinical (and, possibly, biochemical) types of depression, there is significant variability in data on the electrophysiological correlates of depression with different severity of certain syndromes.
In an extensive study specifically devoted to this issue, E.S. Mikhailova [10, 13, 15] analyzed the spectral power and coherence of the background EEG, as well as the reactivity of the EEG and a number of autonomic indicators (GSR, HR) to emotiogenic stimuli in 3 groups patients with endogenous depression with a predominance of melancholy, apatho-abulic and anxious affect in the clinical picture.
In patients with melancholy depression, electrophysiological signs of increased tone of the parasympathetic system were revealed both in the background and in responses to indifferent and emotiogenic sensory stimuli. In accordance with the above ideas, this type of depression is more likely associated with the predominance of the activity of the serotonergic system.
In a group of patients with anxious depression, the nature of electrophysiological indicators indicated increased sympathetic tone, although signs of its functional insufficiency were noted. This type of depression appears to be associated with deficits in both the serotonergic (to a greater extent) and noradrenergic systems, and an imbalance in their interaction.
In patients with apathetic depression, judging by EEG and vegetative indicators, the nature of the response was close to normal, but with a weakening of its intensity.
In general, these and other data [3, 8, 16] confirm the presence of dysfunction of diencephalic subcortical structures (like inhibition deficit) in depressive disorders.
T. Itil et al. [29], using the most modern methods of computer analysis and topographic mapping of the EEG, also identified three types of quantitative EEG patterns: patients with major depressive disorder demonstrated higher alpha rhythm indices than normal; “dysthymic” disorders were associated with desynchronized EEG; with an “unusual” EEG pattern, an affective disorder of an “organic” nature was more often diagnosed.
Different groups of antidepressants also had different EEG profiles: sedative (tri- and tetracyclic) antidepressants reduced alpha activity and increased the content of high and low frequencies in the EEG, while “stimulant” ones, MAO inhibitors and new serotonin- and noradrenergic antidepressants, increased the content of alpha -rhythm and reduced other types of EEG activity. A method has been developed for predicting course therapy based on the EEG response to a single test dose of an antidepressant [29].
Depression and biological rhythm disorders
One of the theories of the nature of affective disorders operates on data on disturbances of biological rhythms, which manifests itself in a violation of the rhythmic structure or discorrelation of many physiological functions - desynchronosis [see. 1]. The morphofunctional basis for the regulation of biorhythms are the structures of the anterior hypothalamus (primarily the suprachiasmatic nucleus), which are part of the parasympathetic part of the autonomic nervous system and are closely connected with the serotonergic nuclei of the brain stem [see. 3].
It is well known that depression causes sleep disturbances, which manifest themselves in difficulty falling asleep and frequent awakenings, especially in the early morning. During the daytime, patients experience feelings of lethargy and weakness due to lack of sleep, and their performance decreases sharply. Sleep disturbances are not specific to depressive disorders; they also occur in other mental illnesses. However, for depression, sleep disturbances are one of the most common syndromes.
Subjectively noted sleep disturbances are confirmed by the results of polysomnographic studies. Depressed patients are characterized by a decrease in the total duration of night sleep and a significant reduction in the duration of slow-wave stages of sleep. At the same time, the rapid eye movement sleep phase (REM sleep) is not suppressed; on the contrary, there is a reduction in the latency period for the onset of the REM phase, which is perhaps the only reliable biological marker of depression [32, 34, 37].
According to the monoaminergic theory of regulation of the sleep-wake cycle [31], such a ratio of sleep phases should indicate a decrease in the activity of the serotonergic system, which regulates slow-wave phases of sleep, while maintaining the functions of the noradrenergic system, which controls the REM phase of sleep.
On the other hand, all drugs commonly used clinically as antidepressants have the same effect on sleep structure, selectively suppressing the REM phase and the phasic EEG correlates of this sleep phase - the so-called pontogeniculo-occipital (PGO) waves, which in experimental animals can be caused by norepinephrine or serotonin depletion [see 28].
Disturbances in the duration and structure of sleep may not only be an epiphenomenon, but also play an important role in the pathogenesis of affective disorders. It has been shown that in healthy people, lack of sleep or disturbances in its frequency (associated, for example, with shift work or transmeridian flights) can cause the development of depressive symptoms [see. 1]. On the other hand, complete sleep deprivation for 40 hours can significantly reduce depressive symptoms in depressed patients and even transfer them into a hypomanic state [36].
Jet lag affects more than just the sleep-wake cycle. It has been shown that in patients with depression, the normal gradient of changes in the frequency spectrum of the EEG during the day is distorted [14], which corresponds to a subjectively more severe condition of patients in the morning hours. Moreover, it turned out that patients with a greater degree of severity of this gradient are more sensitive to psychopharmacotherapy with antidepressants. Depression also disrupts the rhythmic structure of the excretion of a number of hormones [32], fluctuations in blood pressure and body temperature, and the menstrual cycle is often disrupted.
One of the main external factors synchronizing the brain's biorhythm control system is changes in illumination as day and night and seasons change. The perception of these changes is provided by direct retino-hypothalamic pathways, and an increase in illumination has an inhibitory effect on the hypnogenic zones of the anterior hypothalamus, the serotonergic nuclei of the brainstem and their projections. This system appears to play an important role in seasonal changes in animal behavior and may mediate seasonal affective disorder in humans [38]. Based on these ideas, as well as taking into account the important role of serotonergic projections in the activity of the posterior areas of the cortex, various methods of phototherapy for depressive states have been developed [see. 20].
Interhemispheric brain asymmetry and emotional disorders
Based on clinical data from local brain lesions, the literature has developed the idea that the hemispheres of the brain are specifically associated with the regulation of emotions, with the left hemisphere being “responsible” for positive emotions, and the right hemisphere for negative ones.
In one of the most complete reviews of the problem of interhemispheric asymmetry, Bragina N.N. and Dobrokhotova T.A. [2], regarding the consequences of local brain lesions, note that with selective lesions of the temporal part of the right hemisphere in different patients (right-handed), along with other mental disorders, the following were described: on the one hand, melancholy depression; sleep disorders (in particular, an increase in the number and duration of dreams); periodic changes in hypomanic and depressive states; and on the other hand, euphoria, anosognosia, motor and speech disinhibition, decreased criticism.
On the contrary, with damage to the left hemisphere the following were observed: anxious depression; reduction or disappearance of dreams; delusions of relationship; speech impairment and impoverishment; avolution (with damage to the frontal areas), anxiety and confusion (with damage to the temporal areas), affect of suffering (with damage to the posterior areas).
Many of the listed symptoms are in good agreement with the idea of the leading role of the right hemisphere in the occurrence of negative (depression), and the left hemisphere in the regulation of positive emotional states.
The apparent inconsistency of a number of other data presented with hypothetical ideas about the emotional specificity of the hemispheres can be explained by the fact that a local lesion, depending on the volume and location, can cause both irritation (with more or less generalized hyperactivation of the epileptiform type) and functional inactivation of the affected hemisphere (with disinhibition structures of the contralateral half of the brain).
Springer S. and Deutsch G. [18] also note that symptoms of mood disorders (depression) are more likely to appear after damage to the right side of the brain.
EEG studies have repeatedly shown that both in terms of background EEG indicators and the asymmetry of EEG reactions when depressed patients perform various tasks [8, 9, 15, 30], a relatively higher level of activation of the right hemisphere is revealed. Apparently, due to disruption of the interhemispheric balance and hyperactivation of the right hemisphere, patients with depression develop changes in a number of “right-hemispheric” higher cortical functions. Thus, depressed patients exhibit a sharply different character of reactions from the norm to emotiogenic musical fragments [11], they also have difficulty visually perceiving the emotional expressions of faces [12, 23], and there are disturbances in the perception and emotional assessment of smells [30] and colors [7, 17 ]. The latter phenomenon has found practical application in the form of the Luscher test [7].
The functional specialization of the hemispheres is also confirmed by their neurochemical asymmetry. Thus, a predominance of the content of norepinephrine and serotonin was revealed in the right hemisphere cortex, and dopamine, acetylcholine and GABA in the left hemisphere [25]. In the thalamus, an asymmetry in the content of norepinephrine has also been described, but of a more complex type: in the anterior regions of the thalamus (closely connected with the limbic system), its concentration is higher on the right, and in other areas - on the left [33].
Data on interhemispheric asymmetry in relation to emotion regulation and emotional disorders have formed the basis for many non-drug treatments for depression.
In studies of the therapeutic effects of left- and right-sided unilateral as well as bilateral electroconvulsive therapy (ECT) in reducing symptoms of depression, right-sided ECT was found to be more effective than left-sided ECT [19, 26].
A wide range of lateralized physiotherapeutic methods (lateral electrical stimulation, cold exposure, audio stimulation, constant, rhythmic and color photostimulation) were developed by A.P. Chuprikov and co-authors [20] to relieve a number of psychopathological conditions, including affective disorders, as when used in isolation , and in combination with psychopharmacotherapy.
It should be noted that many of the developed methods of non-drug therapy for depression give encouraging results (at least judging by the results given by their authors). It cannot be excluded that in these cases the psychotherapeutic factor is also important in the form of increased attention of doctors and researchers to patients included in the study, more frequent communication with them, which should lead to the activation of “left-hemisphere” verbal mechanisms with a corresponding change in the affective status of patients towards positive emotions. Conversely, more or less pronounced social isolation (for example, older people or people who have lost loved ones) may result in the development or worsening of depression due to a deficit in “left-hemisphere” verbal activation.
Conclusion: problems and prospects
The facts and hypotheses presented in the review indicate a close (and possibly cause-and-effect) connection between depression and metabolic disorders of a number of monoamines, dysfunction of the inhibitory systems of the cortex and diencephalic parts of the brain, and desynchronization of biological rhythms, in particular, mechanisms regulating the sleep-wake cycle , with hemispheric specialization in the control of positive and negative emotions. These data can be used and, in some cases, are already used in practice for the diagnosis and treatment of depressive conditions. They also point to much greater complexity in the interaction of neurochemical and neurophysiological systems in depression than is implied by the simplified “bipolar” models commonly discussed: serotonin/norepinephrine, sympathetic/parasympathetic, right/left hemisphere.
There are serious problems in studying the mechanisms of depression. First, there are no (or have not yet been discovered) experimental models of spontaneous depression in laboratory animals. Conditions induced by reserpine or other drugs that lead to monoamine depletion relate to locomotor activity and sympathetic tone rather than emotional state (mood), and do not show selective interaction with serotonin. Other models, such as learned helplessness, conditioning, self-reinforcing brain stimulation, and social withdrawal, are too complex for drug screening and produce highly variable results when testing even standard antidepressants [28].
Secondly, disturbances may not affect all parts of a particular neurochemical system and, therefore, may not be reflected in all parameters available for research. For example, it is not just the concentration values of the corresponding neurotransmitters or drugs in the blood plasma or cerebrospinal fluid that are informative, but some integral parameters that take into account various characteristics of their metabolism.
Third, it should be borne in mind that clusters of neurons that produce neurotransmitters are very narrowly localized. Thus, nerve cells that synthesize serotonin are located in the raphe nuclei of the medulla oblongata, noradrenergic neurons in the locus coeruleus, dopamine-producing cells in the substantia nigra and mesolimbic region. These human brain structures are inaccessible to invasive research methods and, due to their small size and deep location, do not themselves make any noticeable contribution to the electrical activity of the brain (EEG), so it is not possible to directly identify their dysfunction using electrophysiological methods (the only promising An alternative is intravital positron emission tomography (PET).
On the other hand, the axonal projections of these neurons are distributed very widely throughout the brain. Therefore, any disorders leading to blockade or deficiency of the synthesis of biologically active substances involved in synaptic transmission: neurotransmitters, enzymes, receptor proteins, etc. (genetic, minimal local lesions of brain tissue, or disturbances of local cerebral blood flow in the area of stem nuclei), acting directly on very small volumes of nervous tissue, can lead to a significant change in the functional state of a wide range of brain structures that play a critical role in the implementation or provision of both many individual higher brain functions and the integrative activity of the brain as a whole, i.e. to one or another type of neuropsychiatric pathology.
Only for some neurotransmitter systems is there a more or less defined (but not narrowly local) spatial topography in the cerebral cortex (for example, serotonergic projections are directed predominantly to the parieto-occipital, dopaminergic - to the frontotemporal zones of the cortex, while noradrenergic projections are almost diffuse) . This also complicates indirect topical diagnosis of neurochemical disorders using electrophysiological methods.
Moreover, it is assumed that the key neurotransmitters that play a primary role in the origin of depressive disorders have not yet been found, and drug effects on the norepinephrine and serotonergic systems only modulate the sensitivity of intracellular messengers (cyclo-AMP) to these hypothetical compounds, which may include : some amino acids (primarily glycine), peptides (endorphins, delta sleep peptide), prostaglandins, as well as hormones (ACTH, adrenaline, melatonin) and other monoamines [35].
It is possible that for the selection, monitoring and prediction of the effectiveness of different types of therapy for depression, it will also be important to take into account the individual profile of lateral relationships, the degree of interhemispheric asymmetry and the severity of “left- and right-hemisphere” psychopathological symptoms and syndromes [20].
Finally, due to the presence of a large number of clinical variants of depression, the variability and inconsistency of data on their biological correlates is very high (except in cases of special selection of particularly homogeneous clinical groups), which leads to difficulties in meaningful interpretation of the results of clinical and biological studies and in understanding the mechanisms depression.
Thus, on the one hand, many questions remain unresolved, and on the other hand, new prospects are opening up for further clinical and neurophysiological research with the ultimate goal of approaching the understanding of the etiology and pathogenesis of depressive disorders and optimizing their individual therapy.
Bibliography.
- Ashoff Yu. In the book: Biological rhythms M 1984; 1:54-69.
- Bragina N.N., Dobrokhotova T.A. Functional asymmetries of man, ed. 2nd M 1988; 240.
- Gelgorn E., Lufborrow J. Emotions and emotional disorders. Neurophysiological research. M 1966; 672.
- Glezer V.D. Vision and thinking. L 1985; 256.
- Guselnikov V.I., Iznak A.F. Rhythmic activity in sensory systems. M 1983; 214.
- Seidel K., Ubelhak R. In the book: Guide to Psychiatry / Ed. G.V.Morozova. M 1988; 1: 273-286.
- Klar G. Luscher test. Per. from English M 1975; 199.
- Melnikova T.S., Nikiforov A.I. Vestnik RAMS 1992; 8:45-48.
- Melnikova T.S., Nikiforov A.I., Koptelov Yu.M. et al. Journal of Neuropathol and Psychiatrist 1992; 1: 88-92.
- Mikhailova E.S. Neurophysiological characteristics of various types of endogenous depression. dis. Ph.D. biol. Sci. M 1984.
- Mikhailova E.S. Human physiology. M 1992; 18; 6: 68-76.
- Mikhailova E.S., Vladimirova T.V., Iznak A.F., Tsutsulkovskaya M.Ya. J. Neuropathol and Psychiatrist 1994; 5:55-59.
- Mikhailova E.S., Kamenskaya V.M. J. Neuropathol and Psychiatrist 1982; 9: 1337-1342.
- Mikhailova E.S., Chakhava V.O. J. Neuropathol and Psychiatrist 1992; 1: 95-99.
- Puchinskaya L.M., Krasnov V.M., Korchinskaya E.I. and others. The use of electrophysiological research methods in the clinic of depressive states. Guidelines. M 1988; 21.
- Simonov P.V. Emotional brain: Physiology. Neurophysiology. Psychology of emotions. M 1981; 214.
- Sokolov E.N., Vuchetich G.G., Izmailov Ch.A. In: Emotions and behavior: a systematic approach. M 1984; 275-277.
- Springer S., Deitch G. Left brain, right brain. Per. from English M 1983; 256.
- Traugott N.N. (Ed.). Unilateral electroconvulsive seizure. L 1979; 171.
- Chuprikov A.P., Linev A.N., Martsenkovsky I.A. Lateral therapy. Kyiv 1994; 176.
- Eccles J. Inhibitory pathways of the nervous system. Per. from English M 1971; 170.
- Azzi E. In: R. G. Priest, U. Vianna Filho, R. Amrein and M. Skreta (Eds.) Benzodiazepines Today and Tomorrow. England 1980; 143-146.
- Chayanov NV, Iznak AF, Monosova AJ Proc. of the 6th International Congress of Psychophysiology Berlin (Germany) 1992.
- Costa e Silva JA In: R.G.Priest, U.Vianna Filho, R.Amrein and M.Skreta (Eds.) Benzodiazepines Today and Tomorrow. England 1980; 131-142.
- Flor-Henry P. Cerebral Basis of Psychopathology. Boston 1983; 357.
- Galin D. Arch Gen Psychiat 1974; 31: 572-583.
- Haefely W. In: R. G. Priest, U. Vianna Filho, R. Amrein and M. Skreta (Eds.) Benzodiazepines Today and Tomorrow. England 1980; 19-45.
- Haefely W. In: P. Pichot, P. Berner, R. Wolf, and K. Thau (Eds.) Psychiatry. The State of Art. 1985; 2: 105-110.
- Itil TM, Le Bars P, Eralp E. Neuropsychopharmacology 1994; 10:310.
- Iznak AF, Monosova AJ, Chayanov NV Proc.of the 19th CINP Congress Satellite Symposium on Quantitative EEG & Brain Mapping in Psychopharmacology Washington 1994; 16.
- Jouvet M. Excerpt med 1961; 37: 80-81.
- Linkowski P., van Cauter E., Kerkhofs M., Mendlewicz J. Neuro-psychopharmacology 1994; 10: 16-21.
- Oke A., Keller R., Mefford I., Adams RN Science 1978; 200: 1411-1413.
- Souetre E., Salvati E., Belougou JL et al. Psychiat Research 1989; 28: 263-278.
- Turner P. In: P. Pichot, P. Berner, R. Wolf, and K. Thau (Eds.) Psychiatry. The State of Art. 1985; 2: 151-158.
- Wehr TA JAMA 1992; 267:548-551.
- Wehr TA, Wirz-Justice A. Pharmacopsychiatry 1982; 15:31-39.
- Wehr TA, Moul DE, Barbato G. et al. Neuropsychopharmacology 1994; 10:865.
- Woodward DJ et al. Fed Proc 1979; 738:2109-2118.
19
Functions
What function do alpha rhythms perform?
- Leveling the effects of stress (decreased immunity, narrowing of blood vessels).
- Analysis of all the information that was received by the brain during the day.
- Excessive activity of the limbic system is not allowed.
- Blood circulation in the brain improves significantly.
- All the body’s resources are restored, spurred by the activation of the parasympathetic system.
How does alpha rhythm disorder affect everyday life? Patients whose generation of alpha waves is significantly reduced, as a rule, are more likely to focus on their own problems, they tend to think negatively. Such disorders lead to decreased immunity, the development of various cardiovascular diseases and even oncology. Often there are malfunctions in the glands that synthesize hormones, irregularity of the menstrual cycle, the development of various addictions and a tendency to various types of abuse (for example, alcoholism, drug addiction, overeating, smoking).
A well-established alpha rhythm ensures the normal course of restoration processes in the tissues of the body. It plays a vital role in maintaining the life of an individual.
Signs of Depression
Manifestations of depressive disorder are numerous, varied and can affect not only the emotional sphere, but also the physical one.
Symptoms of depression include:
- sadness, depressed mood for 2 weeks or longer;
- general fatigue;
- pessimism;
- apathy, lethargy;
- irritability;
- tearfulness;
- guilt;
- unstable appetite, weight changes (loss, gain);
- sleep disorders;
- decreased libido;
- attacks of anxiety, fear;
- decreased performance;
- inability to concentrate, memory impairment;
- loss of interest in previously loved things;
- somatic illnesses (complaints about physical ailments, often not previously bothered).
In advanced cases, slow speech, delusional ideas, a noticeable decrease in intelligence, obsessive thoughts about death, and alcohol and drug abuse are common.
1 Diagnosis and treatment of depression
2 Diagnosis and treatment of depression
3 Diagnosis and treatment of depression
Parents of children and adolescents should be alert to the appearance of such signs of depression as:
- sleep disorders;
- decreased appetite, weight loss, slow growth;
- frequent headaches;
- manifestations from the gastrointestinal tract (frequent vomiting, diarrhea, constipation, etc.);
- cardiopalmus;
- inadequate reaction to the ordinary;
- irritability, aggression;
- stubbornness, isolation;
- defiant behavior;
- anxiety, fears;
- decline in academic performance.
Reasons for violations
Electrical impulses ensure rapid transmission of signals between neurons in the brain. Violation of conduction function affects health. All changes are recorded in bioelectrical activity during an EEG. There are several reasons for BEA violations:
- injuries and concussions - the intensity of the changes depends on the severity. Moderate diffuse changes are accompanied by mild discomfort and require symptomatic therapy. Severe injuries are characterized by severe damage to impulse conduction;
- inflammation involving the brain and cerebrospinal fluid. BEA disorders are observed after meningitis or encephalitis;
- vascular damage by atherosclerosis. At the initial stage, the disturbances are moderate. As tissue dies due to lack of blood supply, the deterioration of neural conduction progresses;
- irradiation, intoxication. With radiological damage, general disturbances of the BEA occur. Signs of toxic poisoning are irreversible, require treatment, and affect the patient's ability to perform daily tasks;
- associated disorders. Often associated with severe damage to the hypothalamus and pituitary gland.
EEG helps to identify the nature of BEA variability and prescribe appropriate treatment that helps activate biopotential.
Sources
- https://www.syl.ru/article/325781/alfa-ritm-golovnogo-mozga-norma-i-narushenie-elektroentsefalogramma-golovnogo-mozga
- https://apkhleb.ru/funkcionalnaya/rasshifrovka-eeg-golovnogo-mozga
- https://EtoMigren.ru/head/abate/eeg-golovnogo-mozga
- https://vsepromozg.ru/diagnostika/alpha-activnost
- https://eustress.ru/depression/chetkaja-depressija-al-fa-ritma
- https://neuro-fitness.ru/nejrofidbek/sekrety-alfa-ritma.html
[collapse]