Radiation necrosis , which is a focal structural lesion at the site of the tumor, is a long-term complication of the central nervous system (CNS) after radiotherapy or radiosurgery.
Tissue swelling and the presence of a neoplasm cause changes in the parenchyma of the central nervous system organs located in the tumor bed, which increase the likelihood of developing radiation necrosis. Radiation necrosis can occur when radiotherapy is prescribed for primary central nervous system neoplasms, metastatic brain lesions, or head and neck tumors. Radiation necrosis can occur following any use of ionizing radiation to treat tumors or any protocol for such treatment.
Diagnosis of radiation necrosis and its treatment pose significant difficulties, since the manifestations of this complication of radiotherapy are often overlapped by symptoms of tumor recurrence. An erroneous diagnosis (recurrence of a tumor instead of radiation necrosis) can lead to the prescription of incorrect treatment, which can pose a danger to the patient’s life.
Symptoms of radiation necrosis
It is necessary to understand that radiation necrosis is a long-term complication of radiotherapy, the development of which often occurs months, or even years, after completion of treatment with ionizing radiation. It most often appears between 6 months and 2 years after completion of the last course of radiotherapy.
In modern medical literature, there are data on the incidence of radiation necrosis, which are characterized by significant variability - from 5% to 37% of all patients receiving radiotherapy for intracranial tumors.
However, some authors report that up to 10% of all cases of this complication of radiotherapy were asymptomatic and the detection of radiation necrosis in such cases is entirely due to progress in neuroimaging methods. Attending physicians need to take into account the possible absence of symptoms of radiation necrosis in patients, despite the development of the pathological process.
In cases where the development of radiation necrosis is nevertheless accompanied by symptoms, patients most often experience the following symptoms:
- headache;
- nausea;
- cognitive impairment;
- seizures;
- focal neurological symptoms associated with the localization of the necrosis focus;
- personality change;
- apathy;
- hemiparesis.
Cerebral hemorrhages during radiation necrosis are a rare phenomenon, but, nevertheless, encountered in the practice of neuro-oncologists.
Complications after radiation therapy
During radiotherapy, a general radiation reaction and local changes in the irradiated area may occur.
General radiation reaction
We are talking about the general radiation reaction to radiation. It occurs not only as a result of the damaging effects of radiation, but also as a result of intoxication of the body with tumor decay products. The severity of the reaction depends on the dose of radiation received and the technology used in treatment.
In most cases, the general radiation reaction is mild and does not require a break in radiation therapy or its cancellation. The main clinical manifestations may be:
- Headache,
- dizziness,
- fatigue,
- irritability,
- slight nausea.
Symptoms of a general radiation reaction disappear on their own soon after irradiation - within 2-4 weeks.
However, in the Tomotherapy system, using patented beam shaping technology, negative side effects are much less common than with general radiation therapy.
Local radiation complications
Local reactions can be early (up to 3 months after irradiation) and late (after many months and even years). Their clinical picture is very diverse and depends primarily on what tissues were irradiated:
| Irradiated organs | Possible complications |
| Leather | Redness, radiodermatitis, radiation ulcers, hair loss. |
| Mucous membranes | Ulcerative changes, inflammation of the larynx, pharynx, impaired salivation. |
| Abdominal and pelvic organs | Radiation damage with inflammation of the irradiated segments and corresponding symptoms: stool upset, false urge to defecate, abdominal discomfort. |
| Chest organs | Radiation pneumonia (shortness of breath, cough), inflammation of the esophagus (discomfort and pain when passing food), pericardium. |
| Spinal cord and brain | Inflammatory changes in nervous tissue. |
| Bone | Delayed bone growth and osteoporosis. |
The Tomotherapy system uses technology that minimizes the impact of radiation on healthy organs and tissues surrounding the tumor, making treatment comfortable and improving the patient’s quality of life.
The vast majority of the presented violations are temporary and can be corrected. To prevent many complications, it is enough to follow simple rules for recovery.
Radiation necrosis: diagnosis
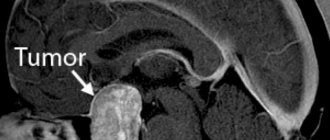
The main methods for diagnosing radiation necrosis are neuroimaging and histological examination of tissue from “suspicious” areas.
MRI is the most common method for diagnosing radiation necrosis. However, it should be noted that images of LN obtained using this method very often resemble the picture of tumor recurrence - with increased contrast in the affected area and edema located along the periphery of the pathological focus.
As a result, due to the low predictive value of conventional MRI, more modern diagnostic methods have become more important:
- magnetic resonance spectroscopy;
- perfusion MRI;
- positron emission tomography (PET).
Diagnosis of radiation necrosis using the first of these methods (magnetic resonance spectroscopy) is based on the fact that a viable tumor has an intact vascular system, as a result of which the volume of blood flow in it is greater compared to necrotic tissue.
For differential diagnosis in this case, the indicator of relative cerebral blood volume obtained using dynamic contrast MRI is used. For tumors, this figure is higher compared to radiation necrosis.
Assessing the metabolite composition of a metastatic brain tumor using magnetic resonance spectroscopy is another valuable method for differential diagnosis. Elevated choline/creatinine and choline/N-acetylaspartate ratios may indicate tumor recurrence rather than radiation necrosis.
Fluorotyrosine PET can also be considered a promising direction in the differential diagnosis of radiation necrosis. Some authors report a sensitivity of 100% and a specificity of 93% for the diagnosis of LN.
As for the use of histological examination to diagnose radiation necrosis, it must be emphasized that the volume of the biopsy specimen must be such as to be able to completely exclude tumor recurrence and at the same time not cause a clinically significant neurological deficit. When taking a biopsy, one should avoid violating the integrity of brain structures located deep in the central part of the thalamus, the motor area of the cerebral cortex, the occipital region and speech centers.
Typically, tissue samples affected by necrosis do not show a predominance of malignant cells. However, irradiated tumor tissue may contain necrotic areas, which does not always indicate radiation necrosis.
In radiation necrosis, examination of a biopsy specimen may reveal thickening of blood vessels with endothelial proliferation and/or hyalinization with fibrosis and moderate infiltration of lymphocytes and macrophages.
Hair loss
Hair loss is an unpleasant complication that affects some patients during treatment.
General recommendations: if the hair loss is severe, then it is necessary to shave the hair completely at the hairdresser. The hair will grow back. During treatment, hair coloring and bleaching should be avoided. For psychological comfort, you can use wigs, scarves, bandanas or hats.
These are the most common problems that a patient may encounter, as well as ways to solve them.
Here are some more tips based on experience in accompanying patients.
Radiation necrosis: treatment
For effective treatment of radiation necrosis, a correct diagnosis is of paramount importance, since an erroneous diagnosis of tumor recurrence and subsequent antitumor treatment can lead to undesirable severe consequences.
For patients without symptoms of radiation necrosis in whom a necrotic mass is detected by MRI during follow-up, a wait-and-see approach may be chosen. If the choice of treatment strategy does not depend on whether the patient has radiation necrosis or recurrent glioma, the patient's condition should be monitored using serial MRI.
However, treatment tactics should be different in the presence of symptoms such as space-occupying syndrome in the cranial cavity, increased intracranial pressure, and neurological disorders. In such cases, it is possible to use the following treatment methods (separately or in combination):
- administration of corticosteroids;
- if steroids are ineffective, the use of bevacizumab (a monoclonal antibody that selectively binds to and neutralizes biologically active vascular endothelial growth factor (VEGF) may be considered);
- hyperbaric oxygen therapy (oxygen supply under pressure of 2-3 atm. Per course of treatment: 20-30 sessions lasting 90-120 minutes each).
Surgical treatment of radiation necrosis has its advantages and disadvantages. Removal of the necrotic mass helps to quickly reduce increased intracranial pressure and restore neurological functions. However, such an operation is associated with a risk of serious complications and is performed mainly on patients in whom conservative treatment has failed.
3. Oral problems, hearing problems, nausea, diarrhea, sexual problems
Oral problems
Before starting radiation therapy to the head and neck, see your dentist for a thorough examination and treatment of dental and oral problems. Radiation can cause unpleasant symptoms:
- Mouth ulcers;
- Lack of saliva;
- Thickening of saliva;
- Difficulty swallowing.
It is important to tell your doctors about these side effects of radiation therapy. Most likely, they will help you cope with your problems. Among other things, to get rid of these symptoms you need to give up spicy and sour foods, as well as alcohol and tobacco. It is helpful to brush your teeth frequently with a soft brush and fluoride toothpaste.
Hearing problems
Radiation therapy can cause hearing loss. One possible cause is the thickening of the wax in the ears due to radiation. You should definitely report this problem to your doctor.
Nausea and radiation therapy
Radiation to the head and any part of the digestive tract may cause nausea and vomiting. Tell your doctor about this symptom because there are medications that can help treat the problem.
Diarrhea
Radiation therapy to the abdomen and stomach may cause diarrhea as a side effect. Diarrhea usually begins a few weeks after starting treatment. Most likely, in this case, the doctor will prescribe special medications and a special diet.
Sexual problems
Radiation therapy to the pelvis can affect fertility and sex drive. Pregnancy is contraindicated for patients undergoing radiation therapy, as the radiation can seriously harm the fetus. Radiation therapy to the pelvic area in women can stop menstrual periods and cause other menopausal symptoms.
In men, radiation to the testicular area can affect the number of sperm produced and the functionality of the sperm. This does not necessarily mean that you will not be able to have children. But in any case, the problem should be discussed with a doctor.
Radiation affecting the pelvic area can cause painful intercourse in some women. Radiation therapy can also cause scarring, affecting the vagina's ability to stretch. In men, radiation can affect the nerves and blood vessels responsible for erections.
About our clinic Chistye Prudy metro station Medintercom page!
Risk factors for radiation necrosis
To date, several risk factors have been identified that contribute to the development of radiation necrosis. According to leading experts in the field of neuro-oncology, despite the fact that these risk factors were mainly found in patients with arteriovenous malformations who were prescribed radiosurgery treatment, as well as patients with glioma, they can be extrapolated to all patients with brain metastases :
- tumor volume and absorbed dose;
- the use of chemotherapy along with radiotherapy;
- tumor localization (the risk of developing LN is maximum when irradiating the frontal cortex and is significantly lower when irradiating the brain stem region);
- histological features of the tumor.
It has also been established that radiotherapy for some metastatic brain tumors is associated with an increased risk of developing radiation necrosis, depending on the form of the primary tumor. An increase in the incidence of LN development is observed with radiotherapy of brain metastases in the following tumors:
- kidney carcinoma;
- lung adenocarcinoma;
- skin melanoma with BRAF V600 oncogene mutation;
- HER2-positive breast cancer.
In addition, increased individual sensitivity to the effects of ionizing radiation also contributes to the development of radiation necrosis.
Source: Radiation Necrosis
Pain
One of the common problems is inflammatory or ulcerative lesions of the oral cavity and the pain associated with this complication.
The patient may notice a decrease in salivation, a change in taste, pain (it can be acute), burning, ulcers on the oral mucosa, difficulty in eating and swallowing.
From the very beginning of treatment, it is recommended to maintain careful oral hygiene:
- use a soft toothbrush,
- brush your teeth after every meal,
- rinse your mouth with saline solution or other solutions as prescribed by your doctor.
- It is necessary to avoid taking hot, sour, irritating, rough foods, as well as hot drinks.
If the above symptoms develop, the attending physician will prescribe appropriate therapy, including pain relief, to alleviate the complication that has arisen.