Phone number of the psychiatrist on duty at SCH
+7
Vascular dementia is characterized by acute or chronic decline in cognitive function, developing as a result of a general decrease in blood supply to the brain or as a result of local infarctions, which, in most cases, are associated with cerebrovascular diseases.
Dementia is a chronic, usually irreversible, decline in cognitive function that affects all aspects of cognitive activity.
Vascular dementia is the second leading cause of dementia in older people. In most cases, it develops in men, usually after the age of 70. It most often occurs in people with vascular risk factors (including arterial hypertension, diabetes mellitus, hyperlipidemia, smoking) and in those who have suffered several strokes. Many patients have a combination of vascular dementia and Alzheimer's disease.
Dementia should not be confused with delirium, although cognitive function is impaired in both conditions. The following signs allow you to distinguish them:
- Dementia primarily affects memory, is usually caused by anatomical changes in the brain, has a slow onset, and is usually irreversible.
- Delirium primarily affects attention, usually occurs during acute illness or as a result of toxic exposure (sometimes life-threatening), and is often reversible.
Other specific characteristics also help distinguish the 2 types of disorders (Differential diagnosis of delirium and dementia*).
What happens in vascular dementia
Blood circulation in certain areas of the brain can be impaired for various reasons: hemorrhage due to a stroke, thrombosis, blockage or narrowing of vascular passages by atherosclerotic plaques. As a result, many cells are deprived of oxygen supply and are deprived of the ability to fully function. Hypoxia gradually or immediately leads to their death. As a result, the structure of the brain changes and its functions are disrupted, which contributes to the development of vascular dementia.
The degree of dementia depends on the size of the affected area; symptoms can be invisible both to the patient himself and to his environment or, on the contrary, to be very striking: inappropriate behavior, neurosis, impaired orientation in time and space, aggression, increased emotionality.
The consequences of the disease are dangerous. Vascular dementia in older people (the symptoms of which we will list later) is fraught with:
- complete loss of ability to work (the patient cannot receive and transmit information, perceive and assimilate new data, establish cause-and-effect relationships);
- human helplessness (he is not able to take care of himself, cook food, go to the store, forgets the simplest household skills, may get lost);
- psychosis (a person becomes dangerous to others, aggressive, prone to inappropriate actions).
Symptoms of vascular dementia rapidly progress, and as a result, the patient’s personality changes dramatically.
Unfortunately, the disease cannot be cured; changes in the brain are provoked by massive cell death and circulatory disorders, so the affected areas are not restored. Drug therapy in this case is prescribed to maintain blood supply to the brain and eliminate the symptoms of vascular dementia (if possible), which will negatively affect the life of the patient and his loved ones.
Patients with dementia are seen by a psychiatrist and a neurologist.
Reasons that can lead to the development of vascular type dementia:
- arterial hypertension;
- diabetes;
- advanced age;
- mental pathologies;
- serious brain injuries, brain surgery;
- insufficient physical activity;
- bad habits.
We recommend
“Senile dementia: causes, symptoms, patient care” Read more
Binswanger's disease
The pathology is named after its discoverer and is subcortical atherosclerotic encephalopathy. Develops as a result of damage to small cerebral vessels and is a fairly common form of dementia: about 1/3 of all dementors.
It has been established that arterial hypertension plays a major role in the development of pathology. It was observed in 80% of patients with this form. Most often, the disease starts after 50 years and begins suddenly. The first signs of it may be a transient disturbance of cerebral circulation, accompanied by sudden paralysis, which, however, also suddenly disappears. Other signs include small strokes and parkinsonism. A magnetic gait is observed when the legs seem to stick to the floor.
Emotional incontinence appears in the form of sudden laughter or crying, speech is impaired, and control over vital functions (for example, urination) is lost. Problems with memory and thinking appear already at the beginning of the disease.
The symptoms of the pathology are quite varied. After all, the process causes extensive damage to brain tissue with ischemia, destruction of nerve cell processes, and demyelination of nerve fibers. The process is accompanied by steady progression, although cases of persistent remission are possible.
How to distinguish vascular dementia from Alzheimer's disease
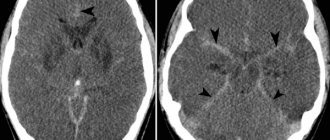
MRI or CT is used as diagnostics; without these studies, it is very difficult to obtain data about the disease and determine its type only by the symptoms that appear. Experts focus on the following indicators:
- If memory and cognitive impairment are observed after a stroke, a diagnosis of vascular dementia is made.
- With signs of Alzheimer's syndrome, the pathological process develops slowly but steadily; with vascular dementia, symptoms arise suddenly, sharply, with a gradual course, and sometimes fluctuations in the manifestation of symptoms occur.
- Often with vascular dementia, signs of focal brain damage, weakness of the limbs (hemiparesis), impaired reflexes of the right and left arms and legs, and the severity of the Babinski reflex appear.
- Gait disturbance (shuffling, slowness, unsteadiness) is also a symptom of vascular dementia. Patients often complain of dizziness, confusing it with instability.
- In chronic ischemia, a characteristic symptom of vascular dementia is incontinence. This symptom is observed in almost all patients.
It is noteworthy that one patient may exhibit both symptoms of vascular dementia and signs of Alzheimer's syndrome. Modern scientists have been able to conduct research that has shown that deformation of cerebral vessels becomes the main factor in the development of Alzheimer's syndrome and one of the main reasons for the onset of the neurodegenetic process. In this regard, many forms of dementia are mixed in nature - vascular-degenerative.
We recommend
“Products for people with dementia that will make life more comfortable and safer” Read more
Neurological disorders
In the initial stage of the disease, neurological dysfunctions manifest themselves as general symptoms. Weakness and fatigue, absent-mindedness, and irritability appear. I am bothered by systematic headaches and sleep is disturbed. There is an unstable emotional background. Depressive states are possible. The person is unrestrained, hot-tempered, and embittered. Emotional incontinence usually manifests itself in violent crying or laughter, weakness.
Among other neurological indicators, cerebellar syndrome occurs, characterized by uncoordinated movements. It seems that the arms and legs are moving chaotically. Because of this, the gait changes: it becomes shaky, slack. The person appears to be drunk. Instability of the step provokes falls.
The disease causes accentuation of personality traits. For example, if previously a person was scrupulous and meticulous, then pathology turns him into a picky grumbler.
Pseudobulbar syndrome is expressed by a triad of signs:
- dysarthria - pronunciation disorder;
- dysphonia – loss of voice sonority;
- dysphagia – problems with swallowing.
There are cases of paralysis and paresis, but quite rarely. Muscle tone and reflexes are increased.
Quite often, malfunctions in the functioning of the pelvic organs occur, and epileptic seizures occur.
In general, dementia of vascular origin is characterized by narrowness and fixation of mental processes, loss of flexibility of thinking, fading of cognitive abilities, and a narrow range of interests.
Vascular dementia and its symptoms
Dementia manifests itself as a complex of symptoms that vary in accordance with the nature of the disease and its stage. Here are common symptoms of vascular dementia:
- difficulty perceiving information;
- impaired orientation in space and time;
- depression;
- apathy;
- memory impairment;
- epilepsy attacks;
- slurred speech;
- inhibited reactions;
- lack of coordination;
- slow cognitive and psychological functions;
- changes in emotional state;
- difficulties in establishing interpersonal relationships.
1. First stage.
The main clinical symptom of vascular dementia is memory impairment. At the beginning of the development of the disease, the clinic manifests itself in a mild form, it is difficult to recognize due to the fact that even a completely healthy person sometimes observes memory problems (who has not at least once lost a phone in an apartment while holding it in their hands, or not confused salt with sugar, or did not try to open the front door with the garage key).
Next, the so-called fixation memory loss appears, when the patient cannot remember what he said or what happened recently. Similar symptoms appear in the early stages of Alzheimer's disease. For such disorders, the best remedy is keeping a diary: the patient will be able to reproduce the necessary facts by reading personal notes.
There is an exacerbation of some character traits. For example, previously a person could rarely criticize his friends, but in the acute stage he begins to literally mock his loved ones or those around him, not missing the slightest opportunity to point out their wrong actions, and becomes a grumpy cynic. The punctuality inherent in a person in previous periods of life turns into pettiness, and “creative disorder” into a real dump, etc.
The ability to make and execute plans decreases, this becomes very noticeable and is complemented by forgetfulness. Simply put, even having dinner at 18:00 for a patient can be an impossible task.
Mental work is too complex for a patient with vascular dementia; he is simply unable to perceive, summarize and analyze information. A person forgets words, repeats what was said several times, and numerous parasitic phrases appear in speech.
For reference! At the beginning of the development of vascular dementia, disturbances of consciousness are not detected.
The patient becomes irritable, tearful, prone to depression, refuses to communicate, confuses days of the week and dates, names of cities, countries, names of famous people. Can take care of himself, but still needs help from relatives.
In the case of a sudden onset of progression of vascular dementia, epileptic seizures and problems with short-term and long-term memory are characteristic.
2. Middle stage.
As the disease progresses, serious memory impairment begins, some real memories are replaced by fictitious ones, the patient reproduces moments experienced in childhood or other long-standing fragments of life very well, even better than healthy people. Fictions can be similar to reality or look like fantastic nonsense.
Sometimes pseudoreminiscence occurs - the patient's old memories move into the present. For example, a grandmother who can barely make it to another room quickly begins to get ready for school or work. Very often the patient asks to be returned to the place where he grew up or was born, and tries to meet with former friends.
Coordination and spatial orientation are severely affected; the patient should not be allowed to leave the house unaccompanied, otherwise he may get lost.
The patient cannot handle household appliances: cook food, wash clothes, clean the apartment. He is still able to take care of himself, but signs of sloppiness are already noticeable: spitting on the floor, wiping his nose with his sleeves, putting garbage in his pockets, etc.
A person loses interest in previously favorite activities; all his leisure time comes down to watching TV or humming songs he learned earlier. In the middle stage of development of vascular dementia, the patient needs outside help and supervision so that he does not cause harm to himself or others.
3. Severe stage.
The last stage of the disease is characterized by worsening symptoms. The patient speaks little, reacts to almost nothing, becomes stubborn and violent. The degradation of physical abilities begins - the patient moves little, cannot walk or move without the help of loved ones. At this stage, a complete breakdown of personal characteristics occurs - the patient does not recognize his relatives and does not remember who he is.
We recommend
“Treatment of dementia in older people: drugs for different stages of the disease” Read more
Acute psychoses
The prevalence among mental illnesses in late life ranges from 4 to 20%. In typical cases, they manifest as evening-night states of confused consciousness without a clear syndromic delineation. Episodes of confusion may recur many times. Delirious states may also occur, as well as hallucinosis, especially visual. Psychotic conditions sometimes become chronic. It happens that psychotic states are limited to pictures of amnestic disorientation and a temporary increase in nighttime anxiety.
It is not so rare that the pictures of psychosis are similar to those in senile or vascular dementia: there are signs of nighttime fussiness with “getting ready for the trip,” with a shift of the situation into the past, with particular fussy business activity. The age-related themes of delusional statements (ideas of damage, robbery, ruin, impoverishment, domestic persecution) are also noteworthy. It is indicated that in the development of psychoses, factors such as sensory deprivation (decreased visual acuity, hearing), psychogenicity (death of a loved one, retirement, etc.), as well as changes in the situation (moving, hospitalization, etc.) are sometimes important. . In addition, cardiovascular diseases, respiratory tract infections, bone fractures and other somatogenies play a significant role.
In the treatment of acute psychoses, measures to improve the somatic condition are of primary importance; among psychotropic drugs, seduxen IM or IV is most often used. Mild antipsychotics in small doses (chlorprothixene, teralen, etc.) may also be indicated. Prognosis: in the majority - this is a way out of psychosis, in some cases, apparently, with a defect in the form of an increase in psychoorganic decline. Death occurs in 27–50%.
Chronic hallucinosis
Among mental disorders of late age, they occur with a frequency of 0.1–0.5% (Shakhmatov, 1976). Nosological affiliation has not been determined. They manifest themselves as hallucinosis syndromes (verbal, visual, tactile, olfactory), transitional and mixed hallucinosis and so-called delusional hallucinosis.
1. Verbal hallucinosis . They can be a manifestation of vascular psychoses, schizophrenia, and are also associated with sensory deprivation. In the latter case, they are observed in the deaf and hard of hearing, which is why they are called hallucinosis of the Bonnet type. Described by E.A. Popov (1956). This psychosis is characterized by mono- or polyvocal true verbal hallucinations, usually unpleasant (swearing, threats, etc.), rarely with imperative content, intensifying in the evening and at night. Deceptions of hearing often seem to grow out of noise in the ears and head; during periods of influx of hallucinations, anxiety arises and criticism of them is lost. Psychosis continues for years, but organic dementia does not occur.
2. Visual hallucinosis. Manifested by chronic or wave-like visual hallucinosis by C. Bonnet. With an influx of hallucinations, criticism towards them disappears, and behavioral disturbances may occur. Consciousness is not impaired. The content of “Lilliputian” optical illusions is associated with experiences that are relevant to patients. Sometimes hallucinations of a different modality are added. In some cases, hallucinosis develops against the background of a pronounced psychoorganic decline, probably of vascular origin.
3. Olfactory hallucinosis . Three variants of psychosis have been described. Gabek's olfactory hallucinosis (1965) occurs after 40 years of age against the background of organic cerebral pathology. Patients consider themselves the source of an unpleasant odor, discover ideas of relationship; They believe that those around them reject them, are depressed, and sometimes make suicidal attempts. Some patients experience senestopathies and some tactile deceptions. Olfactory hallucinosis Shakhmatov (1972) is characterized by true olfactory deceptions, as well as delusional ideas of harm and small-scale persecution. Sternberg's olfactory hallucinosis (1977) is manifested by olfactory deceptions that occur only in a specific environment (for example, in one's room). Sometimes unpleasant tactile and visceral sensations also occur.
4. Tactile hallucinosis. They occur as part of various diseases (organic, endogenous). It was described as an independent disease by Ekbom (1938). Ekbom's hallucinosis is usually associated with delusions of skin parasites.
In the treatment of hallucinosis, mild antipsychotics (chlorprothixene, sonapax, etc.) are usually used; small doses of haloperidol and atypical antipsychotics (clozapine, risperidone, etc.) may be recommended. Prognosis: cases of recovery are rare.
Diagnosis of vascular dementia
The diagnosis is made after a psychodiagnostic study, testing according to the Khachinsky scale and the Mini-mental State Examination (MMSE) system.
Three factors support the diagnosis of vascular dementia:
- Dementia was confirmed by psychodiagnostic testing.
- There are cerebrovascular diseases identified by Dopplerography of cerebral vessels, ultrasound of the great vessels, CT, and MRI.
- The first and second factors coincide or are related.
If the patient has any characteristic symptoms, he is prescribed a differential diagnosis for Alzheimer's syndrome. A comprehensive examination is carried out, the stage of the disease is determined and a course of therapy is prescribed.
We recommend
“Caring for older people with dementia: learning to build relationships” Read more
Forecast
At the present stage of development of medicine, the prognosis for recovery for any type of dementia is unfavorable. Dementia is considered to be an irreversible condition. There is also an unfavorable prognosis for work ability (a patient with dementia is a priori disabled), a relatively unfavorable prognosis for life, but vascular dementia itself is not the cause of the patient’s death.
Death often occurs due to cancer, acute vascular accident, and infectious lesions (especially important among which are diseases of the genitourinary tract due to poor hygiene in patients with dementia).
Treatment methods for vascular dementia
- Drug treatment.
So, the symptoms and treatment of vascular dementia in older people. Considering that this is not a specific disease, but a whole set of different symptoms, a differentiated technique is used for patients. With dementia, damage to the cerebral vessels occurs, which causes the destruction of brain cells, so drug therapy prescribed to the patient is aimed at slowing down the pathological process.
Prevention consists of preventing various vascular diseases, which include damage to capillary networks. For these purposes, medications are prescribed that normalize blood pressure - they try to bring it to 120/80 mmHg.
To prevent cerebral infarctions, drugs of the class of disaggregants are used - drugs to reduce platelet aggregation and to suppress the formation of blood clots.
For heart problems, anticoagulants are used, which inhibit the activity of blood clotting processes.
The patient is prescribed calcium antagonists and peptidergics to restore mental abilities.
The treatment method may vary and depends on the condition of the patient, who must be under the supervision of medical professionals. The doctor monitors all the body’s reactions to treatment, the mental and physical condition of the patient, this approach helps to get the maximum effect from therapy.
- Features of psychotherapy.
Psychotherapeutic methods of treating vascular dementia are used as auxiliary measures. Trainings are conducted for the patient’s social adaptation, which improve important abilities:
— thinking;
- memory;
- speech;
- ability to analyze information.
There are different ways to improve your mental abilities:
- group reading of short stories, discussion of what they read, learning poems helps train memory; For the same purposes, a biographical technique is used: the patient looks at photographs and listens to musical compositions of ancient times;
— keeping a diary helps a lot - it serves as training for the mental function, restores discipline and gives you the opportunity to throw out negativity on paper;
— physical training is effective not only for motor functions, but also for psychological functions; a set of special outdoor exercises helps eliminate signs of depression.
- Lifestyle during illness.
The main thing is to eat right! Salty foods and animal fats are excluded - they are harmful. An important factor is quitting smoking and alcohol.
Under no circumstances should the patient be left alone with the disease. An elderly person must be encouraged to engage in activities and communicate with him so that the symptoms of the disease do not progress unimpeded. Outdoor walks, physical activity and body weight control are required.
After dementia passes into a severe phase, all dangerous objects and devices should be removed from the patient. If a patient has a stroke, it is important to monitor their blood pressure.
Dementia does not go away without a trace, but it is possible to slow down the process and help some brain functions recover. Complex therapy should be prescribed, taking into account the manifestation of symptoms and individual characteristics. In addition to medications, you need a diet, an active lifestyle (if possible) and verbal group communication.
Special forms of late-life psychoses
This is a polyetiological group of mental diseases that develop in connection with endogenous-organic, exogenous, symptomatic and vascular determinants, similar in their manifestations to exogenous types of reactions. In modern taxonomies of mental disorders they occupy different places; in ICD-10 they are coded under headings G06.0–G06.9. There are acute psychoses and chronic hallucinosis.
| | Read about the treatment of psychosis |
Causes of dementia
What are the causes of the death of nerve cells in the brain and the development of acquired dementia? Doctors agree that brain disorders can be caused by many different diseases and negative factors that can destroy brain vessels:
- Diseases of the vascular system Disturbances in the functioning of blood vessels lead to a lack of blood and oxygen supply to brain tissue with all the ensuing consequences;
- Infectious diseases Damage to brain tissue by various viruses, bacteria or toxins due to encephalitis, meningitis, AIDS and other viral diseases often leads to disruption of brain activity;
- Oncological diseases Various tumors, hemorrhages and inflammatory processes affecting the cerebral cortex often cause various disorders with signs of dementia...
- Traumatic brain injuries Physical destruction of brain tissue naturally leads to the death of nerve cells.
- Alcohol and drug abuse Long-term destructive effects of various toxins on nerve cells cannot but affect brain activity.
- Metabolic disorders A whole bunch of hormonal diseases, kidney and liver diseases lead to the accumulation of harmful substances in the blood that adversely affect brain activity.
There is no point in listing all the “risk factors” that, according to modern medicine, can lead a person to dementia. In such a situation, it would seem like a miracle for any person to live to be 80 years old and retain his sanity.
On the other hand, it is never possible to say exactly what exactly was the impetus for the development of senile dementia. If this misfortune happens to a loved one, be patient and contact a specialist...
Stages of dementia development
Dementia has three stages of development, the duration of which depends on the causes of occurrence and the severity of the course.
I. Easy or initial. The ability to lead an independent life is preserved, but intelligence begins to decline. Absent-mindedness and inattention, emotional instability appear, and personality traits become sharper.
II. Moderate. The patient needs partial observation. Memory impairments become more pronounced. This manifests itself in different types of amnesia. Thinking loses flexibility.
III. Heavy. Constant monitoring and help from loved ones is required. Personality destruction sets in. A person no longer controls his simplest vital functions.
Sometimes the last stage of vascular dementia is accompanied by psychosis with hallucinations and delusions, most often paranoid.
Diagnosis
An accurate diagnosis, determining the type of dementia and the degree of development of the probable causes of the disease, can only be made by a doctor (neurologist or psychiatrist). To do this, data is collected on the signs and course of the disease, the patient himself, close friends and relatives living with him are interviewed. Various medical examinations are carried out: cerebral vascular examination, blood tests, MRI... The patient is tested using neuropsychological screening scales.