Neurosis is the name of a mental state disorder characterized by irritability, outbursts of emotions from intense joy to depression, sudden deterioration in health - these manifestations may indicate the presence of neurosis. It is important to distinguish it from a person’s natural temper, as well as from an anxiety disorder or neurosis-like schizophrenia. Let's look at the symptoms and signs of these pathologies and find out how they differ from each other.
In this article
- Neurosis: symptoms, diagnosis, treatment
- Causes of neuroses
- Signs of neurosis
- Types of neuroses
- Neurosis and schizophrenia: differences between pathologies
- Can neurosis turn into schizophrenia?
- Neurosis-like schizophrenia: main differences from neurosis
- Treatment of neuroses
Neurosis: symptoms, diagnosis, treatment
Neurosis, as noted above, is a mental disorder characterized by destructive behavioral manifestations, hysterical and asthenic reactions against the background of decreased mental and physical performance. Neuroses are not so easy to diagnose; they often have a latent (hidden) course. Neurotics themselves are often unable to detect an anomaly, paying attention to their psycho-emotional state only at critical moments of breakdowns and hysterical attacks. The patient’s relatives also do not notice the abnormalities, since neurotic disorders occur latently, appearing from time to time. Patients often withdraw into themselves and limit their social circle, which also makes it difficult to notice unusual behavior.
Causes of neuroses
Experts believe that the main factor leading to the formation of a neurotic state is psychotrauma of various kinds. This could be a stressful situation at work, an intimate problem, even a psychological trauma that happened in childhood and manifested itself in adulthood.
In childhood, we are in a position of constant imprinting - this is the name given to fixing certain information in memory and depending on it. Many impressions and experiences experienced by a child leave an imprint on his future life.
However, almost every person finds himself in difficult situations, and few people can boast of an absolutely cloudless childhood. Why doesn’t everyone develop neuroses? The fact is that experiences and stress alone do not lead to the development of neurosis. They should lie on the prepared soil. What matters are personality traits, character, and innate temperament.
Some manifestations suggest a neurotic condition, but only a specialist can make a final diagnosis.
Diagnosis of these mental disorders
The differences and characteristic symptoms of these diseases serve as the basis for diagnosis. Neurasthenia does not require hospitalization; treatment is carried out in a free form, by mutual agreement with a psychotherapist. The work uses psychotherapy methods. In each individual case, a specialist can use different approaches, methods and techniques for treatment. After a course of psychocorrection, the patient returns to a full life, having in his arsenal auxiliary techniques and techniques for dealing with stress.
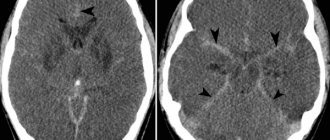
Neurosis and schizophrenia have fundamental differences; the most important thing is awareness and understanding of everything that is happening. In schizoid disorder, there is a loss of reality. The personality and mental functions of a person are destroyed. To make a diagnosis, test conversations are conducted with a psychiatrist, a special assessment is the person’s non-verbal behavior, a number of medical procedures (MRI, EEG, CT), neurological, physiological examination are carried out.
The age of the patient is of great importance; scientists often encounter the first manifestations of schizoid disorders in young people in the late stages of adolescence.
The most important indicator of how to distinguish neurosis from schizophrenia is the characteristic symptoms of these disorders. With neurasthenia, auditory hallucinations are extremely rare; rather, there may be visions in the form of images caused by severe fatigue and insomnia. Neurosthenics may have decreased mental capacity, but they do not have delusional ideas or broken speech.
Foreign scientists argue that timely treatment of schizoid manifestations can significantly improve a person’s quality of life and even in some cases lead to recovery.
Signs of neurosis
The disease manifests itself in completely different ways, but there are also common symptoms:
- increased sensitivity;
- suspiciousness and anxiety;
- sudden change of mood for an unimportant reason;
- depressed mood;
- difficulties in adapting to changed conditions;
- obsessive states.
Rarely, the following factors can lead to the appearance of neurosis:
- infectious diseases of the brain;
- alcoholism, taking psychotropic substances;
- head injuries;
- chronic fatigue;
- lack of sleep.
Due to neurosis, cardiac activity and breathing may be impaired. Problems arise with the gastrointestinal tract, pain in the spine, chills, sleep disturbances and problems in the intimate sphere (impotence, frigidity). Frequent signs of the disease are chronic fatigue, irritability, sensitivity to external stimuli (sounds, smells), dizziness.
Types of neuroses
In medical practice, neurotic pathologies are classified depending on the patient's condition. Here are the most common ones.
- Obsessive-compulsive disorders. This form of the disease is characterized by an irresistible desire to perform repetitive actions, such as clicking a pen or counting objects. The obsessive state also manifests itself in the fear of getting infected, causing harm to oneself, as a result of which it turns into an increased desire for hygiene: washing hands every half hour, brushing teeth, putting things in perfect order, and they are also afraid to touch surfaces in public places. This form of the disease greatly impairs the quality of life and affects the socialization and performance of the patient.
- Hysterical neuroses. Expressed in demonstrative behavior that violates accepted community norms. The reaction to stress in this form of the disorder can be expressed in the following factors: hysterical laughter or screaming, feigned behavior to attract the attention of others, lack of air, tachycardia, stuttering, and other psychosomatic manifestations.
- Anxiety-phobic disorders. The patient experiences unreasonable anxiety, fear due to the possibility of being in certain situations: in the center of attention, receiving a negative assessment from others, being in a confined space.
- Depressive disorders. The patient experiences a feeling of melancholy and loneliness, anxiety, apathy, feels abandoned and unnecessary to anyone. He complains of increased fatigue, impaired memory and attention.
All of the listed manifestations of neuroses are closely intertwined and can be combined. Only a doctor can understand how to distinguish them from each other and from schizophrenia after examining the patient and having a detailed conversation with him. Diagnosis is very important in such cases: the difference between the manifestations of acute neurosis and mental disorders is insignificant. In addition, it is important to distinguish the signs of a neurotic disorder from other pathologies: heart disease, hypertension, consequences of injuries.
Stages of development and forms of the disorder
In the development process, there are three main stages of the disease: latent (debut), active (manifest) stages and a period of stabilization of the patient’s condition.
During the active stage of the disease, symptoms may clearly manifest themselves in various combinations with a sluggish course or acute attacks:
- symptoms of depersonalization;
- hypochondria;
- psychoses and hysterics;
- prolonged neuroses;
- affective state.
The disease can also be accompanied by increased anxiety, various phobias, panic attacks, various rituals that involve double-checking some actions and facts, obsessive doubts, and fear of external influences.
Sluggish schizophrenia can occur in the following forms:
- psychopathic (pseudopsychopathic)
– characterized primarily by symptoms of personality disorders reminiscent of psychopathic disorders (explosive character, mannerisms, eccentric behavior, etc.); - neurosis-like (pseudo-neurotic)
- manifests itself predominantly with neurotic symptoms (phobias, anxiety, insomnia, etc.) accompanied by mild symptoms of schizophrenia. - latent
– the most favorable type of pathology, since it is characterized by the presence of vague symptoms, the disease does not progress to manifest from the debut stage of development; - asthenic
- a relatively mild form with symptoms of rapid fatigue from any type of activity, communication with representatives of asocial strata, collecting - common characteristics of this form; - without productive disorders
- characterized by the absence of productive symptoms (detecting the disease) against the background of visible negative symptoms - damage to body functions, disappearance of various abilities; - obsessive
– characterized by an obsessive state up to the point of worshiping an object or phenomenon, performing an invented ritual before certain actions; - hypochondriacal
– a persistent belief in a non-existent dangerous disease, observed most often in adolescents, women during menopause, pregnant women, when hormonal changes occur; - hysterical
– women are more susceptible, manifests itself in seizures with sudden mood swings from sobbing to laughter, the development of “magical thinking”, hallucinations, and a tendency to wander is possible; - depersonalized
– a disorder of self-perception (typical mainly for adolescents), perception of one’s body and its functions, and the outside world; - affective with a disturbance of the emotional state of 2 types
- manic or hypomanic against a background of general malaise and weakness.
Neurosis and schizophrenia: differences between pathologies
The two conditions may have similar manifestations. But neurosis, unlike schizophrenia, is reversible, that is, it is curable with appropriate therapy, which cannot be said about schizophrenia.
A neurotic breakdown can happen to anyone. It is triggered by stress or psychological trauma. Schizophrenia is a difficult disease to diagnose, the causes of which are not fully understood. External factors can contribute to the exacerbation of this pathology, but they are not its true cause. At the same time, schizophrenia is an endogenous disease, arising due to genetic disposition and personality characteristics.
The difference between the manifestations of schizophrenia and any type of neurosis is also due to differences in the prognosis of treatment. Emotional disorder goes away completely with appropriate therapy: taking medications, competent work with a psychotherapist who identifies the causes and teaches the patient new models of behavior and perception, returning to normal life. It happens that even the help of a specialist is not required if the stress factors have ceased to act and the person has recovered on his own.
If you have ever been diagnosed with schizophrenia, then observation will be required for the rest of your life - this disease, alas, is completely incurable. A period of long-term remission can be achieved, but an exacerbation can occur at any time.
The difference between schizophrenia and neuroses also lies in symptoms. Thus, mental disorder is often accompanied by delusions and hallucinations, often of a violent nature. The patient sees voices that force him to do different things. He experiences suffering and strives to get rid of it by following the instructions. With neurosis, a person may experience illusions (usually before going to sleep or waking up), but does not lose touch with reality, being aware of what is happening. This same factor contributes to the fact that neurotics themselves turn to doctors, experiencing anxiety from their condition. Schizophrenics do not have a critical attitude towards themselves: they do not realize that their behavior is deviant and violates accepted norms in society. And if the relatives and friends of a neurotic person may not be aware of his problem, then the manifestation of schizophrenia cannot be hidden from others, and besides, the patient does not try to do this.
The difference between the manifestations of neurosis and real schizophrenia also lies in changes in the brain: his study showed the presence of organic changes in schizophrenics and their absence in neurotics. As the degree of mental deviation progresses, the patient experiences a breakdown in personality: he moves away from society, becomes lethargic and unemotional. With neurotic disorders, the character and personality traits do not change.
Substance abuse
In patients with schizophrenia, substance abuse is relatively common as a mental disorder concomitant with schizophrenia . According to S. Andreassen et.al. (1987), “although psychopathological conditions predispose to the abuse of various substances, this abuse also predisposes to psychopathological conditions.” If substance abuse precedes the onset of schizophrenia, it accelerates the time of its onset.
Almost 50% (in the literature this percentage varies significantly - 15-70%) of patients with schizophrenia, most often men, demonstrate dependence on psychoactive substances. At the same time, neurotic (anxiety disorders, phobias), personality and affective disorders are more often combined with alcohol abuse than schizophrenia.
Main causes of substance abuse in schizophrenia
- Use of psychoactive substances for the purpose of self-medication: relief of depressive spectrum disorders, negative symptoms, side effects of antipsychotic therapy;
- Inadequate therapy with drugs that are dangerous in terms of the formation of addiction (benzodiazepines, anticholinergics, etc.);
- Negative suggestibility, imitation of other people;
- Conformism;
- Facilitated access to psychoactive substances.
According to K. Muesser et al., (1990), in the group of patients with schizophrenia, schizoaffective disorders and schizophrenia-like psychoses, 47% drink alcohol, 42% use cannabis, 25% use stimulants, 18% use hallucinogens, 7% use sedatives, 4% - “drugs as such.”
Substance abuse and schizophrenia
- Increased severity of positive symptoms;
- Frequent relapses of schizophrenia;
- Frequent hospitalizations;
- The need for long-term treatment in a special hospital;
- Financial difficulties;
- Viral infections caused by infection through parenteral administration of psychoactive substances;
- Criminal behavior.
It has been noted that patients with schizophrenia are more inclined to take dopaminergic drugs, which partially reduce negative symptoms, while provoking a number of productive symptoms (Steinberg J., 2001). Cocaine and amphetamine, as typical dopamine agonists, are characterized by exacerbation of symptoms of schizophrenia.
Substance abuse usually begins in the context of poor compliance and inappropriate medication treatment. In the case of a combination of schizophrenia with dependence on psychoactive substances, the prognosis is usually unfavorable, regardless of the use of certain antipsychotics.
In second place after alcoholism in patients with schizophrenia is cannabis abuse. According to various authors, the risk of schizophrenia in case of cannabis abuse is on average 6-7% of all cases of relatively regular use of this substance.
Multiple substance abuse is common in schizophrenia. Due to the above, in patients with schizophrenia it is necessary to carefully collect a drug history and, during the initial examination, check for the presence of psychoactive substances in the body by conducting toxicological screening of blood serum and urine. In terms of differential diagnosis, it should be borne in mind that drug addicts have better social adaptation, interpersonal relationships are easier to build, and sexual activity is increased compared to patients with schizophrenia.
Taking drugs can trigger the manifestation of schizophrenia and contribute to its relapse.
For patients with schizophrenia with comorbid drug addiction, it can be recommended to take fairly strong antipsychotics that simultaneously have a weak anticholinergic effect. In addition, patients with a “dual diagnosis” (schizophrenia and substance dependence) should receive antidepressants in addition to antipsychotics.
According to some data, patients with “dual diagnosis” have an increased risk of developing tardive dyskinesia during treatment with antipsychotics. On the other hand, akinesia caused by taking a neuroleptic and the resulting anergy may contribute to self-medication with psychostimulants. Note that correction of extrapyramidal disorders with the help of anticholinergic drugs can also lead to abuse of the latter. One of the first signs of dependence on drugs of this class should be considered changes in the cardiovascular system: ECG widening of the QRS complex, prolongation of the QT interval and the appearance of tachycardia.
In the presence of poor compliance, which, as we noted above, is often observed in such patients, it is possible to recommend the prescription of long-acting forms of antipsychotics, presumably suppressing the craving for a psychoactive drug. In particular, the use of flupenthixol depot was previously widely practiced in the treatment of schizophrenia combined with alcoholism. Some authors note the effectiveness of amantadine in the treatment of schizophrenia complicated by addiction to cocaine and anticholinergic antiparkinsonian agents (Kosten T., 1989).
It is known that patients with schizophrenia who abuse cannabis respond worse to antipsychotic therapy than patients without drug dependence.
The need for a cautious approach to the relief of intoxication psychosis caused by taking psychoactive substances should be emphasized. The administration of classical antipsychotics can cause epileptiform syndrome in case of overdose of stimulants.
In the process of multimodal-oriented psychotherapy for patients with schizophrenia who use psychoactive substances, it is important to improve compliance, increase motivation for treatment (“motivational interview technique”), and develop a long-term rehabilitation program for such patients, including contract therapy options with the mandatory involvement of family members in therapy sick.
Can neurosis turn into schizophrenia?
The opinion that neurosis can develop into schizophrenia is erroneous. These diseases are fundamentally different, and primarily differ in the nature of their origin. They may be united by some external manifestations, for example, the presence of phobias, obsessive states, depression, but there are much more fundamental differences - we wrote about them above.
Symptoms of a neurotic disorder disappear after psychological help, and attacks of schizophrenia have a chronic course. Sometimes it is difficult for a doctor to immediately make a correct diagnosis, and what at first seemed like a neurosis turns out to be a mental disorder. However, this does not mean that he still turns into schizophrenia - it’s just that the symptoms of mental deviation appeared gradually, resembling a neurotic disorder at the initial stage.
Neurosis-like schizophrenia: main differences from neurosis
One of the forms of schizophrenia is called sluggish, or in other words, schizotypal disorder, in which a neurosis-like form is distinguished. Unlike classical schizophrenia, which is accompanied by delusions, hallucinations, and personality disintegration, it has symptoms of neurosis, so it is sometimes difficult to distinguish them. With appropriate psychocorrection and medication, remission can be achieved for many years.
Despite the similarity of manifestations, neurosis-like schizophrenia is still different from neurosis. In this situation, it is important for the psychiatrist to establish the correct diagnosis, because under unfavorable circumstances, sluggish schizophrenia can develop into serious mental pathologies - this is its main difference from neurosis.
How to distinguish sluggish schizophrenia from neurosis? These are the symptoms of schizotypal disorder that a doctor pays attention to when making a diagnosis.
- The presence of strange, illogical, and obsessive phobias, for example, that teeth will fall into the gums or the fear of counting to 10, since after this death will occur.
- Hypochondriacal manifestations - the patient suspects that he has terrible, incurable diseases that are only a figment of his imagination.
- Dissatisfaction with some part of one’s body, which seems to the patient to be too ugly or hypertrophied, but in fact is completely normal (for example, the nose or ears).
- Obsessive states that require the repetition of certain actions: for example, going to bed strictly in one position, constantly washing your hands, checking every half hour whether the kettle is turned off, etc.
- The emergence of obsessive ideas that the patient constantly thinks about.
All of the listed symptoms are not characteristic of neurotics, with the exception of some obsessive states. But if they realize the abnormality of their behavior and seek to see a doctor, then with neurosis-like schizophrenia the person does not realize the inadequacy and meaninglessness of their actions.
Manifestations of the disease
Certain difficulties in identifying the disease are associated with the fact that at the initial stage of the disease the patient almost completely lacks such typical symptoms of schizophrenia as delusions or hallucinations. The patient expresses monotonous emotions, does not show initiative, and becomes less active. A person’s intellect becomes dull, and minor oddities and eccentricities appear in their way of thinking, interests and behavior.
Over time, speech may become incomprehensible and confused. But others may not notice these changes, since they last for several months or even years. The shallow personality disorders that can be observed in those suffering from indolent schizophrenia make it possible for them to maintain the required level of adaptation in the family and at work throughout their lives.
In this case, they give the impression of an ordinary or slightly eccentric person to others. Since the signs and symptoms of sluggish schizophrenia are similar to the manifestations of other mental pathologies (depression, neuroses, psychopathy, etc.), only constantly practicing highly qualified specialists with extensive clinical experience can diagnose this type of mental disorder.
Treatment of neuroses
If there are no ways to radically cure schizophrenic disorders in modern psychiatry, then we have learned to fight neuroses. First of all, therapy consists of eliminating the traumatic factor.
For example, if a neurotic disorder has developed against the background of a disrupted daily routine, loss of sleep, or severe emotional stress, then it is necessary to correct these circumstances, normalize the schedule, and regulate the time of sleep and wakefulness. If a severe emotional state is a consequence of psychological trauma, including childhood, negative emotions, you need to seek help from a psychotherapist or psychologist. The specialist will find out the causes of psychological discomfort and apply therapy methods to eliminate them.
Medications are also used to treat neuroses: antipsychotics, tranquilizers, antidepressants, sedatives. To relieve emotional stress, massage, aroma and herbal medicine, and various relaxation procedures are prescribed.