More information about other various diseases: Debility, Double-wave viral meningoencephalitis, Dementia with Lewy bodies, Depressive neurosis, Dermal sinus, Cerebral palsy, Jacksonian epilepsy, Diastematomyelia (diplomyelia), Discogenic myelopathy, Dystrophic myotonia Rossolimo-Steinert-Kurshman, Diabetic encephalopathy I, Dyscirculatory encephalopathy, Diffuse axonal brain damage, Benign rolandic epilepsy.
What is Jacksonian epilepsy?
Jacksonian epilepsy is a painful condition of the human body, which is a separate form of focal epilepsy, which manifests itself in disorders of motor, sensory and mixed nature. The presented disease manifests itself in a specific area with preserved clarity of mind, after which it affects the body in a specially specified order.
This disease is determined by medical staff using various clinical tests, which include: electroencephalogram, magnetic resonance scanning and computed tomography of the brain. In order to get rid of such a pathological process, doctors resort to pharmacological therapy with the help of antiepileptic drugs, dehydration and absorbable drugs.
General information about focal epilepsy
The definition of “focal epilepsy” combines all forms of epileptic paroxysms that arise due to the presence of a local focus of increased epi-activity in cerebral structures.
Epileptic activity begins focally, but can spread from the focus of excitation to the surrounding brain tissue, which causes secondary generalization of the seizure. It is important to differentiate paroxysms of FE and attacks of generalized epilepsy with a primary diffuse nature of excitation. In addition, there is a multifocal form of epilepsy. In this form of epilepsy, there are several local epileptogenic zones in the brain. Approximately 82% of all epileptic syndromes are focal epilepsy, and in 75% of cases it begins in childhood. Most often it occurs against the background of traumatic, ischemic or infectious damage, or disorders of brain development. Secondary focal epilepsy of this nature is diagnosed in 71% of all patients suffering from epilepsy.
general information
Jacksonian epilepsy is a type of focal epilepsy, during which the anomaly manifests itself in the cortex of the pre- and / or postcentral gyrus and is usually of a local type, but in some cases it can develop causing secondary generalization of a fatal seizure. The study of this phenomenon began in the distant 19th century; multiple experiments were carried out by Dr. Bravais from France, as well as by the Englishman J. Jackson, specializing in the field of neurology. As a result of the scientific research of the second scientist, this disease acquired its name.
The presented deviation from the norm appears as a result of a cerebral anomaly of an organic nature, that is, with the formation of inflammation, benign or malignant formations, vascular aneurysms, and other things. At any age, the occurrence of such a process indicates damage to the brain.
Symptomatic frontal lobe epilepsy.
The clinical symptoms of frontal lobe epilepsy (FE) are varied. The disease manifests itself in simple and complex partial seizures, as well as, most characteristically, secondary generalized paroxysms. The following forms of LE are distinguished: motor, opercular, dorsolateral, orbitofrontal, anterior frontopolar, cingulate, emanating from the supplementary motor area. Motor paroxysms occur when the anterior central gyrus is irritated. Characteristic are Jacksonian seizures that develop contralateral to the lesion. Convulsions are predominantly clonic in nature and can spread like an ascending (leg - arm - face) or descending (face - arm - leg) march; in some cases with secondary generalization. With a focus in the paracentral lobules, seizures can be observed in the ipsilateral limb or bilaterally. Post-ictal limb weakness (Todd's palsy) is a common phenomenon of LE. Opercular seizures occur when the opercular zone of the inferior frontal gyrus at the junction with the temporal lobe is irritated. Manifested by paroxysms of chewing, sucking, swallowing movements, smacking, licking, coughing; hypersalivation is characteristic. There may be ipsilateral facial twitching, speech disturbances, or involuntary vocalizations. Dorsolateral seizures occur when the superior and inferior frontal gyri are stimulated. They manifest themselves as adverse attacks with forced rotation of the head and eyes, usually contralateral to the source of irritation. When the posterior parts of the inferior frontal gyrus (Broca's center) are involved, paroxysms of motor aphasia are detected. Orbitofrontal seizures occur when the orbital cortex of the inferior frontal gyrus is irritated and are manifested by a variety of autonomic-visceral phenomena. Characterized by epigastric, cardiovascular (pain in the heart, changes in heart rate, blood pressure), respiratory (inspiratory shortness of breath, feeling of suffocation, compression in the neck, “coma” in the throat) attacks. Pharyngo-oral automatisms with hypersalivation often appear. Noteworthy is the abundance of vegetative phenomena in the structure of attacks: hyperhidrosis, pale skin, often with facial hyperemia, impaired thermoregulation, etc. The appearance of typical complex partial (psychomotor) paroxysms with automatisms of gestures is possible.
Anterior (frontopolar) seizures occur when the poles of the frontal lobes are irritated. They are characterized by simple partial seizures with impaired mental functions. They manifest themselves as a feeling of sudden “failure of thoughts,” “emptiness in the head,” confusion, or, conversely, a violent memory; a painful, painful feeling of the need to remember something. A violent “influx of thoughts”, a “whirlwind of ideas” is possible - a feeling of a sudden appearance in the mind of thoughts that are not related in content to the current mental activity. The patient does not have the opportunity to get rid of these thoughts until the end of the attack. Cingular seizures originate from the anterior cingulate cortex of the medial frontal lobes. They manifest themselves mainly as complex, less often simple partial seizures with behavioral and emotional disturbances. Characterized by complex partial seizures with automatisms of gestures, facial flushing, fearful expression, ipsilateral blinking movements, and sometimes clonic convulsions of the contralateral limbs. Paroxysmal dysphoric episodes with anger, aggressiveness, and psychomotor agitation may occur. Seizures emanating from the supplementary motor area were first described by Penfield, but were systematized only recently. This is a fairly common type of attack, especially considering that paroxysms that occur in other parts of the frontal lobe often radiate to the supplementary motor area. Characterized by the presence of frequent, usually nocturnal, simple partial attacks with alternating hemiconvulsions and archaic movements; attacks with cessation of speech, unclear, poorly localized sensory sensations in the trunk and limbs. Partial motor seizures usually manifest themselves as tonic convulsions, occurring either on one side or the other, or bilaterally (at the same time they look like generalized ones). Characteristic is tonic tension with raising of the contralateral arm, adversion of the head and eyes (the patient seems to be looking at his raised arm). The occurrence of “inhibitory” attacks with paroxysmal hemiparesis has been described. Attacks of archaic movements usually occur at night with high frequency (up to 3-10 times per night, often every night). They are characterized by a sudden awakening of patients, screaming, a grimace of horror, a motor storm: waving arms and legs, boxing, pedaling (reminiscent of riding a bicycle), pelvic movements (as during coitus), etc. The degree of disturbance of consciousness fluctuates, but in most cases consciousness is preserved. These attacks should be differentiated from hysterical and paroxysmal night terrors in children. An EEG study for LE may show the following results: normal, peak-wave activity or slowing (periodic rhythmic or continuous) regionally in the frontal, fronto-central or frontotemporal leads; bifrontal independent peak-wave foci; secondary bilateral synchronization; regional frontal low-amplitude fast (betta) activity. Lesions localized in the orbitofrontal, opercular and supplementary motor areas may not show changes when applying surface electrodes and require the use of depth electrodes or corticography. When the supplementary motor area is damaged, EEG patterns are often ipsilateral to seizures or bilateral, or the phenomenon of secondary bilateral Jasper synchronization occurs. Treatment of LE is carried out according to the general principles of treatment of localization-related forms of epilepsy. Carbamazepine (20-30 mg/kg/day) and valproate (50-100 mg/kg/day) are the drugs of choice; diphenine, barbiturates and lamotrigine are reserved. Valproate is especially effective in cases of secondary generalized seizures. If monotherapy is ineffective, polytherapy is used - a combination of the drugs listed above. Complete resistance of attacks to AED therapy is a reason to consider surgical intervention. The prognosis of PE depends on the nature of the structural damage to the brain. Frequent attacks, resistant to therapy, significantly worsen the social adaptation of patients. Seizures originating from the supplementary motor area are usually resistant to traditional AEDs and require surgical treatment.
Main sources of occurrence
The etiological mechanism of this type of epileptic seizure is:
- Formation of volumetric intracranial objects (tumors, cerebral cysts, abscess, cysticercosis and others).
- Entry of infectious microorganisms into the human body (encephalitis virus, pachymeningitis, neurosyphilis and others).
- Traumatic brain injuries.
- Vascular pathologies.
For children, the main factors causing manifestations of this disease are various intrauterine disorders:
- Fetoplacental deficiency.
- Hypoxia.
- Infectious lesions of the fetus.
- Damage to the baby during childbirth, etc.
Some experts report that genetic predisposition should not be excluded from the list.
Pathogenesis of focal epilepsy
The causes of the development of focal epilepsy are: developmental defects that affect a limited area of the brain (cerebral arteriovenous malformations, focal cortical dysplasia, congenital cerebral cysts, etc.), traumatic brain injuries, infections (brain abscess, encephalitis, neurosyphilis, cysticercosis), vascular system disorders (previous hemorrhagic stroke), metabolic encephalopathy, brain tumors. In PE, one of the etiological factors with preserved morphology of neurons and the medulla as a whole may be acquired and genetically determined metabolic defects of neurons in a certain zone of the cerebral cortex.
Perinatal lesions of the central nervous system are the leading cause among the factors causing focal epilepsy. Such lesions are: fetal hypoxia, asphyxia of the newborn, intracranial birth injury, intrauterine infections. The appearance of a focal pathological focus in childhood may be associated with impaired cortical maturation.
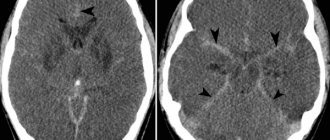
The pathophysiological basis of FE is the epileptogenic focus, in which several zones are distinguished. The zone of pathological damage corresponds to the area of morphological changes in cerebral tissue, which can be recorded using MRI.
The primary zone is the part of the cerebral cortex in which epi discharges are generated.
The symptomatogenic zone is the area of the cortex, when excited, an epileptic attack occurs. The irritative zone is an area that is recorded on the EEG during the interictal interval and is the source of an epileptic seizure.
The zone of functional deficit is the area responsible for the neurological disorders that accompany epileptic seizures.
Symptoms
This type of anomaly has multiple symptoms. The main common feature of all processes is the formation of a tumor in a specific area, often on the upper limbs and facial area, and its further progression throughout the body.
“Motor Jackson” can appear when the cortex of the precentral part of the epileptogenic plane is excited. This form is distinguished by cramps that begin in the muscle tissue of the thumb on the hand, growing to the entire limb, face and legs. In special cases, cramps may start from the first toe on the lower extremity and move upward to the entire structure of the leg, arm and facial area. Such attacks are clinically significant with an early, brief tonic phase. Seizures can end abruptly, but usually occur in the reverse order.
“Sensory Jackson” - manifests itself when the cortex of the postcentral gyrus is activated, is characterized by similar motor activity progression, but is associated with sensitivity disorders. At certain points, the disease occurs in a limited area of its occurrence and cannot spread to other areas. The described phenomenon in modern medicine is called simple Jacksonian paroxysm.
Also, the disease manifests itself with the following symptoms:
- Loss of consciousness (some moments of convulsions occur without loss of consciousness and are localized only at one point).
- The appearance of paresis of the limbs.
- Increased duration and severity of seizures.
- In rare cases, paralysis begins.
Characteristic complaints and symptoms
Jacksonian epilepsy syndrome consists of a variety of manifestations. Paroxysmal seizures differ from the classic version. Doctors at our medical center always identify the typical pathological complex characteristic of this disease.
The most characteristic feature of an attack is the local appearance of convulsive twitching. Most often, trembling or unpleasant sensations (paresthesia, lack of sensitivity) are formed in the face, hand, and fingers. Next, the paroxysmal reaction goes to the shoulder area, then to the leg from the hip to the foot. This sign is called the “Jacksonian march” in medicine. Less commonly, paroxysm comes from the toes, then to the arm and face.
Another type occurs only in the focus of occurrence without spreading. With the classic version of Jacksonian epilepsy, the patient rarely loses consciousness. Sometimes complicated episodes are observed, including status epilepticus, which consists of alternating attacks one after another.
The following processes are distinguished by complexity:
Simple seizures. In this case, convulsions and paresthesias always begin from the same place. The patient can stop their spread by fixing the painful area with his hand.- Complicated paroxysms. Convulsive areas with altered sensitivity progressively spread to different muscles. It becomes impossible to stop their development.
- Complicated with consequences. After an attack, the patient develops paresis of the painful limb. Over time it goes away. This clinical variant alarms the doctor in terms of oncological processes.
Pathological paroxysms are accompanied by additional neurological symptoms characteristic of the main causative disease.
Diagnostic measures for Jacksonian epilepsy
In order to make a specific conclusion, doctors will not need much time, since there is no particular difficulty in making a diagnosis. In fact, difficulties arise when a specialist in the field of neurology searches for the underlying disease that provokes these seizures. When examining a patient, doctors conduct thorough medical history checks, neurological tests, and monitor the patient's mental state. The most common clinical methods for assessing a person's general well-being are:
- EEG - reveals focal pathologies arising from the influence of light and sound pathogens.
- EEG-video examination - provides an image of an ictal EEG, recording peak-wave activity during the final stages of a paroxysm in a different form.
- MRI scan.
- CT scan.
Symptomatic temporal lobe epilepsy.
The clinical manifestations of symptomatic temporal lobe epilepsy (TLE) are extremely varied. In some cases, atypical febrile seizures precede the development of the disease. VE manifests itself as simple, complex partial, secondary generalized seizures, or a combination thereof. Particularly characteristic is the presence of complex partial seizures occurring with a disorder of consciousness, combined with preserved but automated motor activity. Automatisms in complex partial seizures can be unilateral, occurring on the side homolateral to the lesion, and are often combined with dystonic placement of the hand on the contralateral side. TE is divided into amygdala-hippocampal (paleocortical) and lateral (neocortical) epilepsy. Amygdala-hippocampal TLE is characterized by the occurrence of attacks with an isolated disorder of consciousness. Patients are observed to freeze with a mask-like face, wide-open eyes and gaze fixed at one point (he seems to be “staring” - “staring” in English literature). In this case, various vegetative phenomena may be observed: paleness of the face, dilated pupils, sweating, tachycardia. There are 3 types of SSP with an isolated disorder of consciousness: 1. Switching off consciousness with freezing and sudden interruption of motor and mental activity. 2. Turning off consciousness without interrupting motor activity. 3. Switching off consciousness with a slow fall (“limp”) without convulsions (“temporal syncopation”). Vegetative-visceral paroxysms are also characteristic. The attacks are manifested by a feeling of abdominal discomfort, pain in the navel or epigastrium, rumbling in the abdomen, the urge to defecate, and the passage of gas (epigastric attacks). An “ascending epileptic sensation” may appear, described by patients as pain, heartburn, nausea, emanating from the abdomen and rising to the throat, with a feeling of constriction, compression of the neck, a lump in the throat, often followed by loss of consciousness and convulsions. When the amygdala complex is involved in the process, attacks of fear, panic or rage occur; irritation of the hook causes olfactory hallucinations. Possible attacks with mental dysfunction (dreaming states, already seen or never seen, etc.). Lateral VE is manifested by attacks with impaired hearing, vision and speech. The appearance of bright colored structural (as opposed to occipital epilepsy) visual hallucinations, as well as complex auditory hallucinations, is characteristic. About 1/3 of women suffering from VE note an increase in attacks during the perimenstrual period. During a neurological examination of children suffering from VE, microfocal symptoms are often detected, contralateral to the lesion: insufficiency of the function of the 7th and 12th pairs of cranial nerves according to the central type, revival of tendon reflexes, the appearance of pathological reflexes, mild coordination disorders, etc. With age, most patients develop persistent disorders mental disorders, manifested mainly by intellectual-mnestic or emotional-personal disorders; The appearance of severe memory disorders is characteristic. The preservation of intelligence depends mainly on the nature of structural changes in the brain. An EEG study reveals peak-wave or, more often, persistent regional slow-wave (theta) activity in the temporal leads, usually extending anteriorly. In 70% of patients, a pronounced slowdown in the main activity of background recording is detected. In most patients, over time, epileptic activity occurs bitemporally. To identify a lesion localized in the medio-basal regions, the use of invasive sphenoidal electrodes is preferable. Neuroradiological examination reveals various macrostructural abnormalities in the brain. A common finding on MRI is medial temporal (incisural) sclerosis. Often there is also a local widening of the grooves, a decrease in the volume of the involved temporal lobe, and partial ventriculomegaly. Treating EV is challenging; many patients are resistant to therapy. Basic drugs are carbamazepine derivatives. The average daily dosage is 20 mg/kg. If ineffective, increase the dose to 30-35 mg/kg/day and higher until a positive effect or the first signs of intoxication appear. If there is no effect, you should abandon the use of carbamazepine, prescribing instead diphenin for complex partial seizures or valproate for secondary generalized paroxysms. The dosage of diphenine per day in the treatment of VE is 8-15 mg/kg, valproate – 50-100 mg/kg/day. If there is no effect from monotherapy, it is possible to use polytherapy: finlepsin + depakine, finlepsin + phenobarbital, finlepsin + lamictal, phenobarbital + diphenine (the latter combination causes a significant decrease in attention and memory, especially in children). In addition to basic anticonvulsant therapy, sex hormones can be used in women, which are especially effective for menstrual epilepsy. Oxyprogesterone capronate 12.5% solution 1-2 ml intramuscularly is used once on days 20-22 of the menstrual cycle. The prognosis depends on the nature of the structural damage to the brain. With age, most patients develop persistent mental disorders that significantly complicate social adaptation. In general, about 30% of patients suffering from TLE are resistant to traditional anticonvulsant therapy and are candidates for neurosurgical intervention.
Treatment Options
When the above-described symptoms of a disease called Jacksonian epilepsy are detected, specialists from all medical organizations resort to the use of two therapeutic treatment options: an antiepileptic plan and getting rid of the patient’s main painful condition. It is necessary to understand that recovery cannot be considered complete without the effective influence of the second item on the treatment list. Without treating the underlying disease, it is impossible to get rid of epilepsy.
Anticonvulsant administration is done in the form of monotherapy or a complex combination using pharmacological components such as phenobarbital, primidone, valproic acid, etc. At the same time as taking the previously listed medications, substances of a dehydrating nature (ferosemide, acetazolamide, etc.) and resorption therapy, for which hyaluronidase, aloe and other agents are suitable, are prescribed. If such an anomaly manifests itself in the formation of oncology, a cyst or other unfavorable formation, then the patient will need to undergo a consultation with a doctor involved in neurosurgery. This will help provide answers to surgical options. But it is worth understanding that in many cases, after removal of neoplasms that appeared due to an organic nature, patients experience long-term persistence of seizures. In this situation, in addition to previously administered anticonvulsant treatment and an increase in the frequency of seizures, doctors prescribe surgical intervention to get rid of episymptoms.
An operation intended to dissect various elements and remove deformed membranes is considered insufficiently effective. Therefore, specialists use radial techniques in the form of focal resection, during which the area of the cerebral cortex responsible for epiactivity is disconnected. The consequences of this decision are the paralysis of an arm or leg; the removal of the motor areas of the selected structure has been done. After a certain period of time, muscle tone in the paretic zones stabilizes, but paresis, to a certain degree of severity, remains forever.
Also, it is worth understanding that there are no guarantees that seizures will not appear with renewed vigor after some time has passed after surgical removal of the tumor, since the operation can provoke the formation of new scar deformities in the body.
Therapy for focal epilepsy
Treatment of focal epilepsy is prescribed by a neurologist and epileptologist, and includes taking anticonvulsants. Anticonvulsants include: carbamazepine, topiramate, phenobarbital, levetiracetam, etc. For the treatment of parietal and occipital epilepsy, pharmacotherapy will be sufficient. In case of focal temporal lobe epilepsy, after 1-2 years of therapy, resistance to anticonvulsant treatment may occur. If there is no effect from therapy, the doctor prescribes surgery.
The operation is performed by neurosurgeons and is aimed at complete removal of the focal formation (malformation, tumor, cyst) or partial removal of the epi-site. Focal resection is used if the focus of epileptic activity is well localized. If cells that are also a source of epileptic activity are adjacent to the epileptogenic zone, then extended resection is prescribed.