Story
In 1841, the English pediatrician William James West (1793–1848) wrote a letter to the editor-in-chief of the British journal The Lancet, where it was published. The letter was entitled: “On the specific form of infantile paroxysms.” William's son suffered from an unknown illness from the age of four months.
In the letter, Dr. West described his son’s seizures as “tilts.” The child bowed his head to his knees, and then his body completely relaxed. The attack could last up to 2-3 minutes and include up to 20 “tilts”, the intervals between them lasting only a few seconds. The doctor observed such attacks in the boy up to 3 times a day. In his letter, the pediatrician asked his colleagues for help. At the time of writing the letter, the boy was about a year old, and he could no longer acquire new skills and did not know how to move his limbs, never cried or laughed, looked indifferent, could not support his body in an upright position or hold his head on his own. By 11 months, the boy’s seizures began to resemble generalized tonic ones.
Over the next 100 years, epileptologists described syndromes similar to those described by West in children, and by the middle of the last century, about 70 similar cases had accumulated in the world literature. In the early 60s, neurologists first described the EEG pattern in children with paroxysms: hypsarrhythmia, that is, erratic high-amplitude asynchronous spikes and slow-wave activity. In 1964, the term “West syndrome” first appeared.
So what is this disease? West syndrome (WS) is an epileptic encephalopathy in children, manifested by a triad:
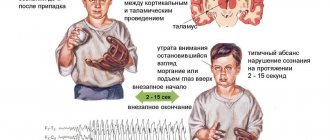
- Infantile spasms (IS). These are short, strong contractions of the muscles connecting the head to the spine and the muscles located along the spine (flexor, extensor, or mixed).
- Hypsarrhythmia - interictal changes on the EEG.
- Progressive impairment of cognitive, behavioral and neurological functions.
SV occurs in 2–6 cases per 10,000 newborns and accounts for up to 9% of epileptic syndromes in early childhood. Boys are more likely to suffer from West syndrome - up to 60% of the total number of patients.
Causes of West syndrome
The causes of this syndrome may be previous intrauterine infections, fetal hypoxia, birth trauma, asphyxia of the newborn, postnatal encephalitis, abnormalities in the structure of the brain, and genetic abnormalities. Often in children it is not possible to identify the cause of the syndrome, but when collecting anamnesis, the presence of family cases of febrile convulsions or epileptic seizures is noted, which gives the right to assume a hereditary predisposition as a risk factor for the disease. The connection between vaccination and the onset of West syndrome has not been established, but the manifestation of the disease often occurs at three to four months of age, which coincides with the beginning of DPT according to most national calendars.
The pathogenesis of this syndrome is not fully understood. As the problem was studied, it was revealed that patients with this syndrome have focal brain lesions. There are several hypotheses: some associate the occurrence of spasms with a disorder of serotonergic neurons, other researchers believe that asynchrony on the EEG is associated with a lack of myelin, which is quite acceptable for this age period. There are also hypotheses about disorders in the brain-adrenal system.
The prevalence of this syndrome ranges from 2 to 5 cases per 10 thousand newborns. The incidence in boys is slightly higher than in girls. By age 3, West syndrome usually resolves or transforms into other forms of epilepsy, such as Lennox-Gastaut syndrome.
The clinical picture of the syndrome is pronounced.
The first symptoms of the disease, as a rule, are observed against the background of delayed psychomotor development - muscle dystonia, speech disorders, crawling, walking, and ophthalmopathies. Only in 1/3 of children West syndrome debuts against a background of health.
Muscle spasms, as a rule, are symmetrical and short-term, often serial, occurring one after another with an interval of less than a minute. Spasms are divided into extensor, flexor and mixed. Most often, local mixed spasms are observed. The generalization of the process for West syndrome is atypical, but is observed in some children.
Contraction of the flexor muscles is accompanied by nodding the head, shrugging the shoulders, and bringing the arms toward the body. Common paroxysms are “jackknife-type” contractions of the abdominal muscles. The combination of this paroxysm with muscle spasms in the upper extremities is called a “salaam attack.” Non-convulsive paroxysms - disturbances in motor activity, twitching of the eyeballs, breathing problems - are also possible, but less common.
Forms
Officially, SV is divided into symptomatic (up to 85%), as well as cryptogenic and idiopathic forms (together up to 20%). But from a clinical point of view, the disease has only 2 forms, since there are practically no differences between the cryptogenic and idiopathic forms. The symptomatic form of West syndrome includes cases of the disease against the background of existing brain pathology or developmental disorders. Half of the children with the symptomatic form had a history of complicated intrauterine conditions: infections, metabolic disorders, genetic and chromosomal defects (Down syndrome, etc.), as well as impaired intrauterine circulation in the mother. Pathology of the birth period is less common. These are hypoxic-ischemic brain damage, trauma and other complications during childbirth. Postnatal causes of WS include infections, trauma, hypoxic-ischemic strokes, and tumors.
The cryptogenic, or idiopathic, form of the disease is diagnosed in children with West syndrome epilepsy for no apparent reason, with normal psychomotor development and without brain damage before the onset of the disease. This is a more favorable form of SV.
The pathogenesis of West syndrome is currently unknown. Patients have a shortened REM sleep phase (rapid eye movement phase), during which the EEG normalizes and the frequency of spasms decreases. In this regard, there is a version that with WS, dysfunction of serotonergic neurons involved in the formation of sleep cycles occurs in the brain stem. There are other hypotheses that involve genetic and immune disorders in young patients.
Treatment results in Germany
Anna (patient’s mother): “After we returned home, to our joy, after a week the trembling disappeared completely. Apparently, the hormone did not take effect immediately.”
Another pleasant moment was that after recalculation for the therapy, the German clinic returned to the family about a third of the amount that they initially paid for treatment in Germany.
Anna (patient’s mother): “A year has passed since our return, Artem is doing well. Of course, we periodically record EEG in Moscow and monitor for any deterioration.
And what’s very nice is that the employees of the GLORISMED company do not forget us: they constantly inquire about our health, help us with ordering medications, and answer our questions.
Our family is very grateful to the German doctors and hosts for the timely assistance and excellent work.”
Epilepsy
Epilepsy. Epileptology. Treatment of children with epilepsy. Epilepsy belongs to the common neurological diseases of a special type that depress human life
Let us help you find the right solution in this difficult situation with your health.
Contact us in any way convenient for you: by phone , by email , by Skype online, by filling out the contact form .
Tell us your contact phone number, our employees will call you back and will gladly answer all your questions absolutely free of charge and guide you on the correct selection of a medical institution, recommend a competent specialist - a well-known doctor from one of the serious specialized German clinics, and also tell you the approximate cost treatment program that is required specifically for you or people close to you.
The consultation is absolutely free for you!
Clinical picture
Most often, the syndrome debuts in children aged 4–6 months, and earlier symptoms are an unfavorable prognostic factor. Infantile spasms of West syndrome can occur with high frequency and be extremely varied - flexion of the body, vertical movements of the eyeballs, or eye movements similar to nystagmus, as well as “throwing up” of the arms like an oriental greeting, etc. One spasm lasts a fraction of a second, spasms grouped in series - up to 50 attacks in a series, the number of episodes per day - from one to several dozen. Often attacks develop upon awakening and falling asleep, and may be accompanied by moving the head or eyes to the side. Only half of the body may be involved in the spasm. The appearance of epilepsy attacks means a stop in the baby’s psychomotor development, and often a regression of acquired skills. In 1–2% of cases, spontaneous self-healing is possible.
Treatment methods
Treatment for West syndrome depends on the severity of the disease and the age of the child. Most often, a positive effect is achieved by taking steroid drugs, large doses of vitamin B6, and some anticonvulsants. If the presence of a pathological focus is confirmed, surgical techniques for its resection can be used. West syndrome is a serious condition with a poor prognosis. Spontaneous regression of spasms is most often observed in children with no mental retardation. With concomitant mental retardation, children experience behavioral and cognitive disorders, autism, and progressive cerebral palsy. As noted above, West syndrome most often transforms into Lennox-Gastaut syndrome. An unfavorable prognosis is also observed when the start of treatment is delayed. The lethality of West syndrome is high only in the group of children in whom the syndrome is caused by anomalies and pathologies of brain development.
Treatment
The most important goal of therapy is to completely stop or reduce the frequency of attacks and suppress hypsarrhythmia, which makes the normal development of the child impossible. Antiepileptic drugs in this case are ineffective. So is there a cure for West syndrome?
In 1958, the most important work on epilepsy and the effectiveness of corticotropin administration for infantile spasms was published in the European Journal of Neurology (authors L. Sorel and AA Duchamp-Boyol). ACTH helped in 50–90% of cases, and the cryptogenic form responded better to treatment than the symptomatic form. In a large Finnish study from 1980, the fatal complication rate of corticotropin therapy was 5% and the incidence of serious adverse events was 37%. The high risk of complications and low effectiveness of corticotropin in the symptomatic form of WS led to the need for further search for drugs to relieve spasms.
Other hormonal agents are now used: prednisolone, dexamethasone and tetracosactide. The latter drug is a synthetic polypeptide that has the properties of endogenous corticotropin and produces fewer complications than corticotropin itself. Over the past 20 years, the antiepileptic drug vigabatrin has proven itself. Susceptibility to therapy is 23–68%. The optimal dose and duration of treatment have not yet been determined for either vigabatrin or corticotropin and tetracosactide.
In addition, valproate and benzodiazepines are prescribed in the treatment of West syndrome. However, the complete disappearance of infantile spasms with these drugs occurs later than with treatment with steroids and vigabatrin. For a localized focus of epileptoid activity, surgical treatment is possible, but it is not effective in all cases.
The dynamics must be assessed by EEG monitoring, since during therapy, spasms can become subclinical, which are difficult to recognize without an EEG. In remission (a month without attacks), hypsarrhythmia may completely disappear, replaced by a normal EEG. But in 23–50% of cases of West syndrome, the prognosis is not very good - the disease transforms into other forms of epilepsy, which sometimes can only manifest themselves during puberty.
Second stage of epilepsy treatment in Germany
Anna (patient’s mother): “After a month of taking the medication, we began to gradually reduce its dosage. The attacks have partially returned. Although they were smaller and less frequent than before arriving in Germany, a decision was made to undergo hormone therapy with Cortisone. This was the second stage, which took us about a month.”
During the hormone therapy, the family spent the first two weeks in a German clinic as an inpatient. This is a prerequisite for such treatment, because there is a risk of the child having an allergic reaction to the drugs.
Anna (patient’s mother): “Already on the fifth day of therapy, almost all manifestations of epilepsy went away, the EEG was clear, Artem only had rare twitches.”
After discharge from the clinic, Artem and his parents were required to visit the clinic daily for outpatient monitoring of laboratory parameters for another 2 weeks, when the dosage of the hormonal drug was gradually reduced.
Forecast
Since William West's letter to The Lancet, the prognosis for Westies has undoubtedly improved, but remains extremely grave. Unfortunately, the mortality rate from the disease itself or complications of its treatment during the first 3 years of life reaches 11% and over the past 40 years it has remained unchanged. Normal intellectual development is preserved in 9–28% of children. Normal or close to normal intelligence in cryptogenic and idiopathic forms is preserved more often - in 38-78% of cases, whereas in the symptomatic form - only in 2-18% of children. The prognosis of each child with West syndrome is extremely individual - the quality and length of life depends both on the form of the disease itself and on the timeliness and effectiveness of treatment.
Sources
- Kholin A. A., Mukhin K. Yu. West syndrome. Etiology, electro-clinical characteristics and differential diagnosis // Mukhin K. Yu., Petrukhin A. S., Kholin A. A. Epileptic encephalopathies and similar syndromes in children. M.: Art-Service Ltd (2011): 95–133.
- Gaponova O. V., Belousova E. D. Prognostic criteria for infantile spasms // Epilepsy and paroxysmal conditions 3.3 (2011).
- Temin P. A. et al. Infantile spasms and West syndrome // Diagnosis and treatment of epilepsy in children. M.: Mozhaisk-Terra. (1997): 287–354.
The first stage of treatment in a German clinic
Because the family did not have a Schengen visa, GLORISMED employees helped them obtain an official invitation from a German clinic to obtain a medical visa to Germany.
Anna (patient’s mother): “We collected the necessary amount, borrowed money and went to Germany. We were met at the airport and helped to check into an apartment in Berlin.
The day after our arrival, we went to the clinic with an interpreter, who was also provided to us by GLORISMED. While we were registering, the child had a seizure, a stretcher was immediately brought in, several doctors came running and Artem was taken to the ward.
On the very first day, German specialists had a consultation regarding further actions and treatment of the child. About 7 doctors and junior medical staff came to us and discussed Artem’s case in detail. I just want to note that such an examination and joint discussion of the proposed treatment, of course, will not be found in our hospitals.
At the German epilepsy clinic, we immediately had confidence that these doctors would provide the most competent and timely assistance. It was very relaxing that we were in the hands of such experts.”