Classification
Subdural hematomas are classified according to the speed of development of clinical signs. There are the following types of hemorrhages:
- acute subdural hematoma: manifestations occur within seventy-two hours from the moment of injury;
- subacute subdural hematoma is defined when symptoms develop within four to fourteen years after injury;
- chronic subdural hematoma is characterized by the onset of symptoms several weeks or months after injury (usually more than three weeks).
Subacute and chronic types of hemorrhages occur more often as a result of vascular damage under the influence of various factors; acute – as a result of traumatic brain injury. Subdural hemorrhage occurs with equal frequency both on the side of injury and on the opposite side according to the biomeanical principle of counter-impact (the brain is displaced to the side opposite to the impact and can be injured when colliding with the bone skull on the opposite side).
Heart attacks
This is an acute condition characterized by blockage of the lumen of the artery or its sharp spasm, followed by impaired circulation and the appearance of an area of tissue necrosis (scientifically called necrosis).
Code 63 corresponds to the ICD 10 code for stroke of ischemic type, the gradation is as follows:
- thrombosis of arteries in the neck and base of the skull - corresponds to the number 0, embolism - 1, unspecified rupture - 2;
- thrombosis of cranial arteries - coded 3, embolism - 4, unspecified etiology - 5;
- vein rupture – 6;
- unknown and other heart attacks are marked with numbers 8 and 9.
All of the listed sub-clauses of the classification are placed after the dot; if, for example, the veins are damaged, the code will look like this: I 63.6. Heart attacks are very dangerous; according to statistics, about 80% of all strokes are ischemic. Such patients are hospitalized in the intensive care unit and are under the supervision of a doctor.
Symptoms
The symptoms of a subdural hematoma are extremely variable. Manifestations of hematoma are caused by local, cerebral and brainstem disorders. A “light” period is characteristic - the time period immediately after the injury, when there are no manifestations. The duration of the “light” interval can vary from minutes and hours to several days. In chronic forms, this period can be months or years.
Subdural hematomas are characterized by an undulating course, while other patients may suddenly fall into a coma.
Focal symptoms depend on the location of the hemorrhage, general cerebral symptoms depend on its volume and the amount of compression of the brain, brainstem symptoms depend on the nature of the lesion in the brainstem and the percentage of its wedging into the foramen magnum.
Intracerebral hematoma (Intraparenchymal hematoma of the brain)
General cerebral symptoms
In most cases, intraparenchymal hematoma is accompanied by severe cerebral symptoms. Patients experience dizziness, intense headache, nausea and vomiting. More than half of cases of intracerebral hematoma are characterized by impaired consciousness from stupor to coma. Sometimes depression of consciousness is preceded by a period of psychomotor agitation. The formation of an intracerebral hematoma can occur with the presence of an erased light gap in the patient’s condition, with a longer light gap or without it.
Focal symptoms
The focal symptoms of intracerebral hematoma depend on its volume and location. Thus, with small hematomas in the area of the internal capsule, a more pronounced neurological deficit occurs than with significantly larger hematomas localized in areas of the brain that are less functionally significant. Most often, intracerebral hematoma is accompanied by hemiparesis, aphasia (speech disorder), sensory disturbances, asymmetrical tendon reflexes of the right and left extremities, and convulsive epileptic seizures. Anisocoria, hemianopsia, frontal symptoms may be observed: a disorder of criticism and memory, behavioral disorders.
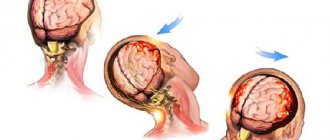
Dislocation syndrome
An extensive intracerebral hematoma quickly leads to the appearance of dislocation syndrome, which occurs as a result of displacement of brain structures. Causing an increase in the volume of the contents of the cranium, an intracerebral hematoma leads to a displacement of brain structures in the caudal direction and herniation of the cerebellar tonsils into the foramen magnum. The consequence of this is compression of the medulla oblongata, clinically manifested by stem symptoms: nystagmus, impaired swallowing (dysphagia), respiratory rhythm disorder, diplopia, hearing loss, vestibular ataxia, hypo- or anosmia, strabismus and drooping of the upper eyelid, bradycardia, hyperthermia and increased blood pressure.
Hemorrhage into the ventricles
Intracerebral hematoma with a breakthrough of blood into the ventricles is characterized by hyperthermia, rapidly developing depression of consciousness up to coma, the presence of meningeal symptoms, hormetonic convulsions - a paroxysmal increase in the tone of the muscles of the limbs, as a result of which the arms are bent and brought to the body, and the legs are extended as much as possible.
A delayed intracerebral hematoma is clinically manifested by a lack of improvement in the patient’s condition or a sharp deterioration in his condition a day or more after the injury.
Variants of the course of the disease
There are three main variants of the clinical picture of subdural hemorrhages:
- Classic clinic. A change in the state of consciousness occurs in three phases: loss of consciousness at the time of injury, a clear “bright” interval, and repeated loss of consciousness. During the recovery period, the patient reports severe headaches, nausea, dizziness, and possible memory loss. Focal symptoms manifest themselves later, during the period of deepening stunning. At the same time, a sharp increase in headache occurs and vomiting develops.
Focal symptoms: most often these are mydriasis, sensitivity disorders, contralateral pyramidal insufficiency (lack of brain function appearing on the opposite side from the side of the lesion).
From stem symptoms
: secondary stem syndrome (decrease in heart rate, respiratory dysfunction, tonic convulsions).The three-phase clinical pattern is more common for the subacute form than for the acute form. In these cases, euphoria and decreased criticism of one’s condition may occur.
- Option with an erased picture of the “light” gap. Primary loss of consciousness can reach the level of coma. Stem and focal symptoms are clearly expressed. Then there is a partial restoration of consciousness (usually to the point of stunning). After some time, the patient again falls into stupor or coma, and the disturbances in vital functions deepen. Epileptic seizures may develop, and hemiparesis increases.
- Option without a “light” gap. Occurs with multiple, severe brain injuries. The patient is in a stuporous state or in a coma. Moments of clarity of consciousness are either erased or absent; there is practically no positive dynamics noted.
Blockages and spasms of blood vessels without heart attack
In clinical practice, there are often cases where disruption of blood flow does not cause necrotic changes. According to ICD 10, such conditions are included in two large groups:
- I 65 – includes damage to the carotid, vertebral and basilar arteries emerging from it;
- I 66 – this code indicates spasm or embolism of the cerebral and cerebellar arteries.
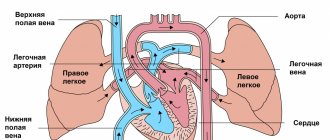
Nerve cells are very sensitive and quickly die due to oxygen starvation and lack of nutrients. But the brain is structured in a unique way; it contains the so-called “Circle of Willis” - these are “spare” connections between arteries, thanks to which blood can flow through bypass vessels. That is why sometimes obstruction does not lead to cerebral infarction.
Let us note the main reasons that can create an obstruction in the artery:
- Spasm is a narrowing of a vessel due to contraction of its muscles, resulting in a decrease in its capacity. Usually the cause is neurogenic;
- Narrowing - differs from the previous version by violating the anatomical integrity of the vascular wall in a certain area. Such changes are irreversible;
- Thrombosis is the formation of a blood clot on the artery wall, which gradually increases in size and creates an obstruction;
- Embolus - circulates along with the blood, enters a vessel of a smaller caliber and causes its blockage. Usually this is a detached blood clot or atherosclerotic plaque.
The listed reasons often lead to cerebral infarctions or the development of severe conditions after stroke, having a certain code according to ICD 10.
Consequences of subdural hematoma
The occurrence of subdural hemorrhage is accompanied by rapid displacement of the brain and infringement of its stem structures. Subdural hematoma usually develops against the background of severe damage to the skull and brain, and therefore has an unfavorable prognosis.
The outcome and consequences of a subdural hematoma of the brain depend on the speed of recognition of the hemorrhage and the competently chosen treatment method. The prognosis is based on other factors: the patient’s age, the volume of hemorrhage, somatic complications. Statistics today indicate a high mortality rate among such patients and disability among survivors.
Treatment
It is performed conservatively or surgically, depending on its type, volume, as well as the individual characteristics of the patient. In the acute form, removal of the subdural hematoma is often indicated. Detection of displacement and compression of brain structures is a stimulus for surgery as soon as possible from the moment of injury (or rupture of a vessel).
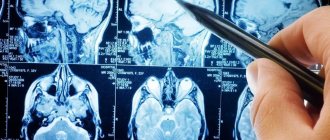
a) With MRI without contrast, the image reveals areas of fluid accumulation indicated by white arrows - subacute subdural hematomas. b) MRI visualizes foci of increased signal intensity (indicated by white arrows), as well as foci of reduced MRI signal intensity (indicated by black arrows), these signs are characteristic of acute subdural hematomas.
The absolute indication for surgical treatment of a subdural hematoma is the thickness of the accumulated blood more than one centimeter, determined by imaging studies (MSCT, MRI). The postoperative period should be accompanied by the maintenance of vital functions and control of intracranial pressure.
The operation is also indicated for subacute subdural hemorrhage, if there is an increase in focal symptoms and the appearance of signs of intracranial hypertension.
Remaining classification
We have listed the main gradation of cerebrovascular disorders, which are often encountered in clinical practice. Let us note the remaining pathologies, concomitant diseases and conditions after stroke, which correspond to their code according to ICD 10:
- I 64 – set when it is not possible to distinguish hemorrhage from ischemia;
- I 67 – cerebrovascular pathologies not related to strokes and heart attacks;
- I 68 – cerebrovascular accident in other diseases;
- I 69 – complications of stroke.