Find out more about nervous diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
What is glossopharyngeal neuralgia?
If the cranial nerve is affected by a quarter on one side, and paroxysms of pain appear in the tonsils, soft palate, pharynx and ear, then the patient may have neuralgia of the glossopharyngeal nerve. With this pathology, a violation of the taste perception of the posterior third of the tongue, on the affected side, is detected. Hypersalivation and decreased reflex of the palate and pharynx are also noted. To make a diagnosis, an examination by a neurologist or dentist is required. CT and MRI of the brain are indicated as hardware diagnostic methods. In most cases, treatment is conservative, including:
- Anticonvulsants;
- Analgesics;
- Sleeping pills and sedatives;
- Vitamin therapy;
- Physiotherapy;
- General strengthening procedures.
Diagnosis and treatment of neuralgia of the cranial nerves
Neuralgia is diagnosed by a neurologist; to exclude diseases of the oral cavity, ear, nose and throat, consultations with specialized specialists may be required: otolaryngologist, ophthalmologist and dentist. In order to identify the cause of secondary neuritis, high-tech CT or MRI studies, echo and electroencephalography are prescribed.
The main method of treating cranial neuralgia is conservative therapy and in most cases recovery occurs within 2–3 weeks; in severe cases, the recovery period takes several months. If there is compression of the nerve and muscle paresis, surgery may be required.
Structure of the glossopharyngeal nerve
N. glossopharyngeus or glossopharyngeus nerve begins in the nuclei of the medulla oblongata. It is based on motor, sensory and autonomic parasympathetic fibers. Moreover, the sensory fibers begin in the sensory nucleus common to the vagus and glossopharyngeal nerves. They innervate the mucous membrane of the pharynx, soft palate, tongue, tonsils, and Eustachian tube. The sensation of taste in the anterior two-thirds of the tongue is provided by taste fibers emerging from the nucleus of the tractus solitarius. The taste fibers of the glossopharyngeal nerve are responsible for the taste sensations of the posterior third of the tongue and epiglottis.
The motor fibers originate in the nucleus ambiguus and innervate the stylopharyngeal muscle, which is necessary for raising the pharynx. Together with the vagus nerve, they form the reflex arcs of the pharyngeal and palatal reflexes.
Parasympathetic fibers originate in the salivary nucleus. Being part of the tympanic and lesser petrosal nuclei, they reach the autonomic ganglion, and with the branch of the trigeminal nerve they regulate salivation of the parotid gland.
Since the pathways and nuclei of the glossopharyngeal and vagus nerves are common, isolated pathology n. Glossopharyngeus. But more often symptoms of combined lesions are observed.
Leaders of sells
Bachelor's degree from 2014 to 2021 Printing house RUB 14,950
GOZNAK 19,950 rub.
Order
Specialist diploma from 2014 to 2021 Printing house RUB 14,950
GOZNAK 19,950 rub.
Order
Master's degree from 2009 to 2010 Printing house RUB 12,950
GOZNAK 17,950 rub.
Order
Specialist diploma from 2011 to 2013 Printing house RUB 13,950
GOZNAK 18,950 rub.
Order
Studying at an institute or college lasts more than one year. A master's degree is usually obtained after 5.5 years of hard study, and a bachelor's degree is obtained only after completing 4 university courses. This is a huge period of time, which a modern business person is always sorely lacking.
The procedure for purchasing a diploma rarely exceeds two days. This is a negligibly short period of time compared to traditional training.
Pathogenesis
There are cases of idiopathic Sicard syndrome. At the same time, it is almost impossible to establish the etiology of the disease. Provoking factors may be:
- Acute or chronic intoxication;
- Otitis;
- Pharyngitis;
- Tonsillitis;
- Sinusitis;
- Atherosclerosis;
- Viral infections incl. flu.
Secondary neuralgia occurs due to:
- Arachnoiditis, encephalitis and other infectious lesions of the posterior cranial fossa.
- TBI.
- Hyperthyroidism.
- Diabetes mellitus.
- Meningiomas, gliomas, medulloblastomas and other intracerebral tumors of the cerebellopontine ganglion.
- Compression and irritation of any part of the glossopharyngeal nerve.
- Nasopharyngeal tumors.
- Intracerebral hematomas;
- Carotid artery aneurysm;
- Hypertrophy of the styloid process.
- Overgrowth of osteophytes of the jugular foramen.
- Ossification of the styloid ligament.
In some cases, pathology may be the first symptom of cancer of the larynx or pharynx.
Symptomatic picture
Clinical signs include painful paroxysms lasting from a few seconds to three minutes. A sharp acute pain originates at the root of the tongue and instantly spreads to the tonsils, soft palate, ear and pharynx. May radiate to the eye, neck and lower jaw. Pain can be triggered by coughing, chewing food, its temperature, yawning, swallowing and even talking. During paroxysm, dry mouth is noted, immediately after hypersalivation. But dryness is not a mandatory sign of diagnosis, because the secretory insufficiency of the parotid gland can be compensated by the remaining salivary glands.
Paresis of the levator pharyngeal muscle does not cause swallowing disorders. But difficulties in chewing and swallowing associated with impaired proprioceptive sensitivity, which is responsible for the position of the tongue, may be noted by patients.
The disease has a wave-like course, worsening in autumn and winter.
Cost of purchased diplomas and certificates
Studying on a paid basis costs the student a good amount of money. At the most prestigious faculties of elite universities, tuition fees amount to tens of thousands of dollars. Not every person has the constant ability to pay the required price.
Buying a diploma is much cheaper than paying tuition. Standard prices are 20,000 rubles, prices vary slightly depending on:
- From the level of the educational institution;
- Specialties and specializations;
- Years of admission and graduation;
- Urgency of order fulfillment.
Each client needs to individually choose the terms of cooperation, but we will definitely take the main points into account when completing the order.
Who needs quick diplomas?
Studying at a university or college often has a negative impact on the health of students. We have to expend the strength of a young body:
- To study a large number of non-core subjects;
- Attending boring lectures and mandatory practical classes;
- Passing sessions and defending final works;
- Writing a thesis project and communicating with curators.
You can get a diploma with a minimum of effort. You just need to leave a request on the website and wait for contact with the company manager. Instead of tedious full-time or part-time studies, living expenses, tests and exams, many choose a different path.
The potential buyer gets the opportunity to engage in his own practical self-education. He does not need to study many related disciplines that will never be useful in the future. A failed part-time student is freed from communication with teachers who are not always adequate.
Selling diplomas is carried out without unnecessary complications. Within a couple of days, the customer receives the desired document.
How to verify the authenticity of documents
For most employers, having a diploma when hiring is a formality. It is much more important that a person has solid practical experience and outstanding personal qualities. Many companies specifically require a document from applicants for management positions in order to narrow the pool of potential applicants.
Therefore, verifying the authenticity of the provided diploma or school certificate is usually the responsibility of the personnel department employees. The employee will visually inspect the document, make a copy and attach it to his personal file. This diploma fully meets the necessary criteria of the Russian Ministry of Education.
Serious verification of documents is possible only in some cases. The most common official requests are sent to:
- From law enforcement agencies;
- Large commercial firms;
- Companies working in the financial sector;
- Oil refining industry organizations;
- State medical institutions.
Order a diploma from us - get a prestigious job in commercial structures with minimal risks of detecting a fake
Diagnostic methods
The diagnosis is made by a neurologist, who, if necessary, can involve an otolaryngologist and dentist. During the examination, the doctor determines analgesia, that is, the absence of pain sensitivity at the base of the tongue, upper parts of the pharynx, and tonsils. Taste sensitivity is also studied, for which a taste solution is applied to symmetrical areas of the tongue. The diagnosis is confirmed by isolated unilateral taste disorder in the posterior third of the tongue. Bilateral disruption is typical for diseases of the oral mucosa, such as chronic stomatitis.
The pharyngeal reflex needs to be checked. To do this, touch the back wall of the throat with a paper tube, which provokes a swallowing movement and occasionally a cough. Normally, touching the soft palate should be accompanied by a lifting of the palate and uvula. Sicard syndrome is characterized by the absence of reflexes on one side. But a similar symptomatic picture can occur with damage to the vagus nerve. If the pharynx and pharynx are strewn with herpetic rashes, the doctor can diagnose ganglionitis of the ganglionitis of the glossopharyngeal nerve nodes, which differs in almost identical n. Glossopharyngeus clinical picture.
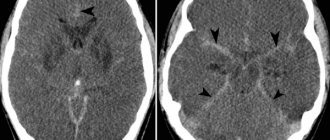
To establish the root cause of symptomatic neuritis, neuroimaging diagnostics is needed:
- MRI or CT scan of the brain;
- Electroencephalogram;
- Echo-EG;
- Ophthalmoscopy with consultation with an ophthalmologist.
It is necessary to distinguish between neuralgia of the glossopharyngeal nerve and diseases that cause painful paroxysms of the face and head. These include:
- Neuralgia of the ear ganglion;
- Trigeminal neuralgia;
- Oppenheimer's syndrome;
- Glossalgia;
- Ganglionitis of the pterygopalatine ganglion;
- Retropharyngeal abscess;
- Tumors of the pharynx.
Methods for preventing voice disorders during extrafascial operations on the thyroid gland
Fuki E.M., Trofimov E.I., Gubeev R.I.
Scientific Clinical Center of Otorhinolaryngology FMBA of Russia Contact:
Fuki E.M., e-mail:
Published
: Journal “Oncosurgery”, 2012, volume 4, no. 1.
annotation
: the article discusses voice disorders caused by damage to the motor nerves of the larynx during operations on the thyroid gland, as well as ways to prevent these complications.
Materials and methods
. We analyzed the results of treatment of 62 patients with nodular pathology of the thyroid gland who were in a state of euthyroidism, in 12 of whom well-differentiated thyroid cancer was verified. Depending on the indicators of postoperative electromyography of the larynx, patients were divided into 2 groups: 1 – with pathological signs 16 (25.8%), 2 – without pathological manifestations 46 (74.2%).
During thyroid surgery, we used electrophysiological neuromonitoring (Neurosign 100 device) and/or optical magnification using an operating microscope to detect and preserve the laryngeal nerves.
results
. The methods we used to detect the laryngeal nerves allowed us to identify the recurrent in all cases and the external branch of the superior laryngeal nerve in 62 (82.9%) of 76 cases.
Before surgery, 3 (4.8%) patients showed pathological changes in the electromyogram of the larynx, which after surgery either worsened or remained virtually unchanged. 6 months after surgery, pathological changes remained in 5 (8.1%).
Complaints after surgery about voice fatigue, loss of sonority, and hoarseness of varying degrees were noted in 12 (75%) in group 1 and in 6 (13%) in group 2. Survived for more than 6 months in 2 (12.5%) group 1.
During an acoustic study, 14 (87.5%) patients of group 1 showed a decrease in the maximum voice frequency by more than 10% from the original, a decrease in the sound pressure level at high frequencies by 5-10 dB, these phenomena persisted for more than 6 months in 6 (37, 5%) 1 group. In group 2, the maximum frequency decreased by less than 5% in 25 (54.3%), by 5-10% in 9 (19.6%), and by 10-20% in 2 (4.3%). In 5 (10.8%) – 6 months, a reduction in frequency of more than 5% persisted.
After surgery, in 4 (25%) patients of the first group, the vocal fold of the affected side was lowered, shortened, sagged during inspiration and became convex during exhalation, which indicated damage to the external branch of the superior laryngeal nerve in these patients.
conclusions
. Voice changes after thyroidectomy should not be ignored, even if standard indirect laryngoscopy remains normal. Although the clinical significance of the external branch of the superior laryngeal nerve remains overshadowed by the recurrent laryngeal nerve, the need for its preservation is obvious. During surgery, it must also be carefully identified, like the recurrent nerve, and carefully protected from traumatic factors, such as coagulation or ligation. Care should be taken to treat the cricothyroid muscle, the adjacent laryngeal joints, and the prelaryngeal muscles.
Statistically, the most reliable method for determining the condition of the external branch of the superior laryngeal nerve and the cricothyroid muscle is LEMG, while acoustic voice analysis and laryngostroboscopy are the main screening procedures for this pathology.
It is apparently impossible to avoid damage to the laryngeal nerves in absolutely all patients, however, precise performance of the operation using intraoperative neuromonitoring and postoperative phonopedic correction significantly reduces the likelihood of persistent voice changes.
Keywords:
dysphonia, laryngeal nerves, recurrent laryngeal nerve, external branch of the superior laryngeal nerve.
Introduction
In recent decades, there has been an increase in the incidence of thyroid diseases, a significant portion of which require surgical treatment [1, 2].
The most well-known specific complication of thyroid surgery is a change in voice after surgery, which is usually associated with injury to the recurrent nerve [2, 4, 5, 21]. However, maintaining the integrity of the recurrent laryngeal nerve does not guarantee the preservation of normal voice after intervention [22]. Voice changes in most cases are caused by damage to the external branch of the superior laryngeal nerve (ELBN) [11, 13, 15]. According to FH Lahey (1932), the frequency of damage to the recurrent laryngeal nerve depends on “how much one wants to notice it.” This statement is even more true for damage to the NVGN [21]. According to various literature sources, NVVGN injury during operations on the thyroid gland ranges from 0 to 58% [15, 22, 23]. The differences in results are partly explained by different surgical techniques, methods of assessing the condition of the cricothyroid muscle, and also, partly, by the desire of the surgeon to hide the complication that has arisen.
The superior laryngeal nerve arises from the node of the vagus nerve, immediately inferior to the jugular foramen. Having reached the internal carotid artery anteriorly, it divides into 2 branches [13]. The internal, sensitive branch innervates the mucous membrane of the larynx above the glottis. The external branch of the superior laryngeal nerve is motor, 60-65 mm long, follows along the inferior constrictor and enters the cricothyroid muscle [11, 15]. When this muscle contracts, the thyroid cartilage tilts anteriorly, the distance between it and the arytenoid cartilages increases, resulting in tension in the vocal folds [8]. The normal functioning of the cricothyroid muscle is especially important for the production of high tones of the female voice [9, 19].
Cricothyroid palsy can be a life-altering blow for those whose careers depend on the quality of their voice and speech. As an example, we can cite the world famous coloratura soprano – Amelita – Galli Curci (Fig. 1). A slow-growing thyroid nodule threatened her career for 15 years. In 1935, under local anesthesia with intraoperative phonation control, after careful identification, demonstration and preservation of both recurrent nerves, a goiter weighing 170 g was removed. After the operation, she noted a narrowing of the vocal range due to the loss of high notes to lyric soprano. Despite the absence of laryngoscopic signs of laryngeal paresis, slight hoarseness appeared [12]. Newspaper critics wrote that “her amazing voice was gone forever, instead of velvety it became trembling, like a sad ghost begging for reincarnation” [7].
Rice. 1
. Amelita - Galli Curci.
Damage to the NVGN cannot be reliably detected by indirect laryngoscopy or acoustic voice examination [9, 17]. For evidence-based diagnosis of paresis of the cricothyroid muscle, it is desirable to use laryngeal electromyography (LEMG) and laryngostroboscopy [6, 14, 17].
To prevent accidental damage to the NVGN, intraoperative visualization is performed [18, 22, 23]. To facilitate the detection of such a fine anatomical structure in a surgical wound, it is convenient to use the superior thyroid artery (STA) as a landmark, which crosses the nerve at various distances to the upper pole of the gland lobe. Depending on this distance, there are 3 types of relationships between this artery and the NVGN according to Cernea et al. (1995) [10] and 4 types according to Kierner et al. (1998) [20] (Table 1).
Table 1
. Classification of the relationship between the external branch of the superior laryngeal nerve and the superior thyroid artery.
| Cernea et al. | Kierner et al. | Criteria |
| Type 1 (68% small goiter, 23% large goiter) | Type 1 (42%) | Crosses the thyroid gland >1 cm upward from the upper pole of the thyroid gland |
| Type 2a (11% small goiter, 15% large goiter) | Type 2 (30%) | Crosses the thyroid gland <1 cm superior to the upper pole of the thyroid gland |
| Type 2b (14% small goiter, 54% large goiter) | Type 3 (14%) | Crosses the thyroid gland under the capsule of the upper pole of the thyroid gland |
| – | Type 4 (14%) | Descends posteriorly from the artery and crosses the branches of the VSCA directly above the upper pole |
Reports on the identification of NVVGN during interventions on the thyroid gland are rare and are found, as a rule, in foreign literature. Successful nerve isolation is observed in 33-93% of cases [10, 12, 18, 22, 23].
The purpose of the study was to determine the functional state of the NVGN after surgical interventions on the thyroid gland, performed using intraoperative neuromonitoring.
Materials and methods
62 patients with nodular pathology of the thyroid gland in a state of euthyroidism were treated, in 12 of whom well-differentiated thyroid cancer was verified. The average age of the patients was 42 years. There were 47 women. Depending on the indicators of postoperative LEMG (on days 7-10), the patients were divided into 2 groups: the first - with pathological LEMG signs (16, or 25.8%), of which 3 (4.8%) were bilateral ; the second – without pathological manifestations (46, or 74.2%).
LEMG is considered the most objective method for determining the condition of the neuromuscular apparatus of the larynx [8, 9, 14]. We carried out this study using the Neuro-MEP-2 device and the corresponding software. Bioelectric potentials were recorded using needle electrodes inserted into the cricothyroid muscle. Electromyography was performed at rest with quiet breathing, during attempts to phonate sounds of conversational frequency and the highest possible “I” (Fig. 2).
Rice. 2
. Insertion of a needle electrode into the cricothyroid muscle.
Normally, phonation is accompanied by the appearance of an accelerated series of electrical impulses, continuously following each other. Motor unit potentials from the cricothyroid muscle have an amplitude of about 500 mV and a duration of 0.7 ms. Pathological EMG signs are: decrease or absence of potentials when attempting high-frequency phonation; the appearance at rest of positive sharp waves, fibrillation, polyphasic waves. It was mandatory to compare the symmetry of the indicators of the right and left sides. Changes in the duration, amplitude, and shape of motor unit potentials were of secondary importance.
The patients underwent surgical interventions on the thyroid gland ranging from hemithyroidectomy to thyroidectomy, and, if indicated, lymph node dissection of the neck. During surgery, to detect and preserve NVGN, we used electrophysiological neuromonitoring methods (Fig. 3, 4) and/or optical magnification using an operating microscope (Fig. 5, 6). Intraoperative electroneuromyography of the cricothyroid muscle was performed using a Neurosign 100 device (UK).
Rice. 3
. External view of the Neurosign 100 neurosurgical monitor.
Rice. 4
. Electrophysiological neuromonitoring of NVVGN - needle electrodes inserted into the cricothyroid muscle.
Rice. 5
. Identification of laryngeal nerves using an operating microscope.
Rice. 6
. Microscopic visualization of the external branch of the superior laryngeal nerve.
It should be noted that surgical treatment was performed in 65 patients, but 3 patients were excluded from the analysis because they experienced laryngeal paresis due to damage to the recurrent laryngeal nerve.
A total of 76 NVGNs were at surgical risk, of which 62 (82.9%) were found. Before and after surgery (immediate results were assessed in the first week after surgery, long-term results – after 6 months), a comprehensive assessment of voice function was performed.
Voice handicap index test questionnaire developed by BH Jacobson et al. [16], includes 30 questions regarding voice disorders. Depending on the frequency of occurrence of disturbing changes, they are assessed on a five-point scale from 0 to 4 (0 - never; 1 - almost never; 2 - sometimes; 3 - almost always; 4 - always). It should be noted that this test is subjective, the results of which largely depend on the patient’s perception of his problems.
In accordance with the recommendations of the Union of European Phoniatricians, the Yanagihara scoring scale was used to assess hoarseness [24].
Multiparametric acoustic study of the voice was carried out using the Multi-Dimensional Voice Program computer program (USA). During acoustic analysis of the voice, the fundamental frequency and sound pressure level of the voice, Jitter, Shimmer, HNR, time of maximum phonation, vocal field and speech profile were determined.
Videolaryngostroboscopy allows you to evaluate not only the amplitude of movements of the vocal folds, but also the regularity of vibrations, the presence of a closing phase, displacement of the mucous membrane along the free edge of the vocal folds, symmetry, amplitude and frequency of the fundamental tone. To assess phonatory vibrations, we used a five-point system for assessing the vocal folds proposed by G.F. Ivanchenko [3].
If patients had changes confirmed by objective diagnostic methods, phonopedic correction was performed.
results
In the preoperative period, 3 (4.8%) patients had pathological LEMG manifestations, which either worsened after surgery or remained virtually unchanged (Fig. 7). After 6 months after surgery, 6 people refused repeat LEMG; pronounced pathological changes remained in 5 (8.1%) (mainly in patients with bilateral changes).
Rice. 7
. Comparison of motor unit potentials during phonation at high frequencies: a – normal electrical activity of the cricothyroid muscle, b – on the part of the operation, there is a decrease in the frequency of potentials and the absence of a complete interference pattern.
Complaints after surgery about voice fatigue, loss of sonority, and hoarseness of varying degrees were noted by 12 (75%) patients in the first group and 6 (13%) in the second. They persisted for more than 6 months. in 2 (12.5%) patients of the first group.
The Voice Quality Index before surgery averaged 19.2±3.5 points. He was assessed after 2-3 and 6 months. after operation. In the first group it was 64.5±4.1 and 26.2±3.2, respectively, in the second – 38.1±3.7 and 8.3±1.2.
During an acoustic study, 14 (87.5%) patients of the first group showed a decrease in the maximum voice frequency by more than 10% from the original, a decrease in the sound pressure level at high frequencies by 5-10 dB. These phenomena persisted for more than 6 months. in 6 (37.5%) patients of the first group (Fig. 8). In the second group, a decrease in maximum frequency of less than 5% was noted in 25 (54.3%), by 5-10% in 9 (19.6%), by 10-20% in 2 (4.3%) examined. In 5 (10.8%) patients, a reduction in frequency of more than 5% persisted for 6 months.
Rice. 8
. The results of the acoustic analysis of the voice of patient Ch. with clinical signs of postoperative paresis of the NVGN: a – before surgery; b – on the 14th day after surgery: there is a decrease in the maximum fundamental frequency of the voice (Max F0), with an almost unchanged average frequency (Ave F0), a decrease in the average and maximum strength of the voice (Ave Int) and (Max Int).
During videolaryngostroboscopy before surgery, the total index of vibration disorders was 0.4. After surgery in group 1 on day 7 – 1.6, after 6 months. – 1.1; in group 2 on day 7 – 0.9, after 6 months. – 0.2. In 4 (25%) patients of the first group, the vocal fold of the affected side was lowered, shortened, sagged during inhalation and became convex during exhalation. An oblique glottis has formed, its posterior parts are shifted to the affected side (Fig. 9). These patients had aspiratory hoarseness.
Rice. 9
. Laryngoscopic picture of paresis of the left NVGN: sagging of the left vocal fold below the level of the edge of the right one, incomplete closure of the folds during phonation, causing inferiority of the closing phase. Adduction and abduction of the vocal folds were preserved.
Conclusion
Voice changes after thyroidectomy should not be ignored, even if standard indirect laryngoscopy remains normal. Despite the fact that the clinical significance of the NVLN remains overshadowed by the recurrent laryngeal nerve, the need for its preservation is obvious. During surgery, the NVGN must also be carefully identified, like the recurrent nerve, and protected from traumatic factors such as coagulation or ligation. You should also take care of the cricothyroid muscle, the adjacent laryngeal joints and the prelarynx muscles.
According to the data obtained, the diagnosis of NVGN damage cannot be based solely on the analysis of voice disturbance or videolaryngostroboscopy. A statistically significant correlation is observed between a decrease in voice frequency and pathological LEMG. Other non-invasive diagnostic techniques correlated with LEMG statistically at the trend level. The most reliable method for determining the state of the NVGN and cricothyroid muscle is LEMG, while acoustic voice analysis and laryngostroboscopy are the main screening procedures for this pathology.
It is apparently impossible to avoid damage to the laryngeal nerves in absolutely all patients, however, precision performance of the operation using modern methods of intraoperative neuromonitoring and postoperative phonopedic correction significantly reduces the likelihood of persistent voice changes.
Literature
- Bondarenko V.O. Complex express diagnostics and tactics of surgical treatment of thyroid diseases: Abstract of thesis. dis. ...Dr. med. Sci. – M.: 1993; 38.
- Kamardin L.N., Bubnov A.N. Modern trends in the surgical treatment of thyroid diseases. Issues of clinical surgery of the endocrine system. L.: 1987; 5-21.
- Ivanchenko G.F. Functional microsurgery in patients with voice disorders due to paralysis and cicatricial deformities of the larynx: Abstract of thesis. dis. ... dr. honey. Sci. – M.: 1992; 26.
- Trofimov E.I., Ivanchenko G.F., Darmakov V.V. and others. Correction of persistent vocal and respiratory disorders after surgical interventions on the thyroid gland. Thyroid cancer and endemic goiter. Conference materials. 2007; 137-138.
- Cherenko M.P. Complications during operations on the thyroid gland. Kyiv: Health. 1977; 110.
- Abelson TI, Tucker HM Laryngeal findings in SLN paralysis: a controversy. Arch Otolaryngology Head Neck Surgery. 1981; 89: 463-470.
- Anonymous. Brave return. Time. 1936; Dec. 7.
- Arnold GE Physiology and pathology of the cricothyroid muscle. Laryngoscope. 1961; 71: 687-753.
- Beyer TE Traumatic paralysis of the cricothyroid muscle. Laryngoscope. 1941; 51: 296-304.
- Cernea CR, Nishio S., Hojaij FC Identification of the EBSLN in large goiters. Am. J. Otolog.y 1995; 16: 307-311.
- Durham CF, Harrison TS The surgical anatomy of the superior laryngeal nerve. Surgery Gynecology Obstetrics. 1964; 118: 38-44.
- Eisele DW, Goldstone AC Electrophysiologic identification and preservation of the superior laryngeal nerve during thyroid surgery. Laryngoscope. 1991; 101: 313-315.
- Furlan JC, Brandao LG, Ferraz AR Surgical anatomy of the extralaryngeal aspect of the superior laryngeal nerve. Arch Otolaryngology Head Neck Surgery. 2003; 129: 79-82.
- Haglund S. The normal electromyogram in human cricothyroid muscle. Acta Otolaryngologica. 1973; 75: 448-453.
- Hunt CJ The superior and inferior laryngeal nerve as related to thyroid surgery Am. J. Surgery. 1961; 27: 548-552.
- Jacobson BH, Johnson A, Grywalski C. The Voice Handicap Index (VHI): Development and Validation. Am. J. Speech-Language Pathology. 1997; 6: 66-70.
- Jansson S., Tisell L., Hagne I. Partial SLN lesions before and after thyroid surgery World J. Surgery. 1988; 12: 522-527.
- Jonas J., Bahr R. Neuromonitoring of the EBSLN during thyroid surgery. Am. J. Surgery. 2000; 179: 234-236.
- Kark AE, Kissin MW, Auerbach R. Voice changes after thyroidectomy: role of the external laryngeal nerve. Brit. Med. J. 1984; 289: 1412-1415.
- Kierner AC, Aigner M. The EBSLN: its topographical anatomy as related to surgery of the neck. Arch. Otolaryngology Head Neck Surgery. 1998; 124: 301-303.
- Lahey FH Operative injury to the recurrent laryngeal nerve. Surgica.l Clinics. North. America. 1932; 12: 839-848.
- Lennquist S., Cahlin C., Smeds S. The superior laryngeal nerve in thyroid surgery. Surgery. 1987; 102:999-1008.
- Lore JM, Kokocharov SI, Kaufman S. 38-year evaluation of a surgical technique to protect the EBSLN during thyroidectomy. Ann. Otology. Rhinology. Laryngology. 1998; 107: 1015-1022.
- Yanagihara N. Significance of harmonic changes and noise components in noise. J. Speech. Hearing. Res. 1967; 30: 531-541.
Therapy
To treat neuralgia of the glossopharyngeal nerve, conservative therapy is prescribed. The only exception is if the underlying cause is tumors and hypertrophy of the styloid process, leading to compression of the nerve. In these cases, surgery is indicated.
To relieve pain, a 10% solution of cocaine is prescribed, which is applied to the root of the tongue and pharynx. This allows you to eliminate paroxysms for 6-7 hours. If this remedy turns out to be ineffective, a 1-2% novocaine solution is injected into the root of the tongue. Non-narcotic analgesics and anticonvulsants are also prescribed internally. If the pain syndrome is pronounced, it is advisable to prescribe sedatives, hypnotics, antipsychotic medications and antidepressants. AFT, multivitamin complexes and FiBS are used as general strengthening agents.
Among the physiotherapeutic procedures that have proven effectiveness are:
- SMT on the area of the larynx and tonsils;
- Diadynamic therapy;
- Galvanization.