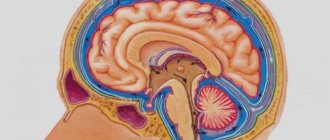
Atrophic hydrocephalus of the brain is characterized by excessive accumulation of cerebrospinal fluid in the cerebrospinal fluid cavities of the brain. The pathological process develops against the background of diseases that cause atrophy of brain tissue. Moderate asymmetric hydrocephalus occurs when one of the ventricles of the brain expands. Atrophic hydrocephalus is asymptomatic for a long time. To identify signs of the disease, neurologists at the Yusupov Hospital conduct a comprehensive examination of patients.
The Neurology Clinic has created all the conditions for the treatment of patients with atrophic hydrocephalus. The rooms are equipped with air conditioning, allowing you to create a comfortable temperature regime. Patients are provided with individual personal hygiene products and dietary nutrition. The staff of the neurology clinic is attentive to the wishes of all patients.
The Yusupov Hospital employs candidates and doctors of medical sciences, leading experts in the field of hydrocephalus treatment. Doctors of the highest category have the necessary knowledge and experience and apply individual treatment regimens for patients depending on the cause and severity of the disease. Specialists at the rehabilitation clinic use modern methods of restoring neurological functions, perform massage, conduct manual therapy and a course of physical therapy.
Causes
Atrophic hydrocephalus develops against the background of the following diseases:
- tumors of the ventricles and brain matter;
- toxic and alcoholic encephalopathies;
- infectious brain lesions (ventriculitis, encephalitis, meningitis);
- vascular cerebral pathology, including rupture of an aneurysm and intraventricular and subarachnoid cerebral hemorrhages resulting from defects in arteriovenous connections;
- pathologies of the development of the nervous system (Dandy-Walker syndrome, stenosis of the Sylvian aqueduct);
- post-traumatic conditions and brain injuries.
In atrophic encephalopathy, cerebrospinal fluid fills the space formed inside the skull as a result of a decrease in brain volume. Atrophic hydrocephalus of the brain in elderly and senile people can develop against the background of impaired blood supply to the brain due to arterial hypertension, atherosclerosis of cerebral vessels, and diabetic angiopathy.
Diagnostics
To document the presence of pathology, the doctor needs to conduct a comprehensive neurological examination. Identifying symptoms alone is not enough. The doctor checks the patient's reflexes, sensitivity, memory and attention capabilities. Instrumental diagnostic methods are prescribed in the form of:
- Neurosonography;
- Dopplerography in brain tissues and vessels;
- Computed tomography (CT) and magnetic resonance imaging (MRI), as well as positron emission scanning (PET);
- Electroencephalography (EEG).
Laboratory methods play a lesser role in establishing the diagnosis of brain atrophy.
Degrees and types
Acquired hydrocephalus develops after injury or disease of the brain. The cause of congenital hydrocephalus is infectious lesions of the brain during intrauterine development of the fetus. Internal hydrocephalus of the brain in adults is characterized by impaired distribution of cerebrospinal fluid due to the formation of blood clots, neoplasms or adhesions. Internal open hydrocephalus of the brain occurs due to the destruction of part of the brain matter, due to which the cerebrospinal fluid does not have a complete outflow of cerebrospinal fluid.
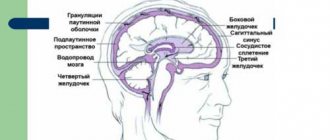
Based on the location of the cerebrospinal fluid, the following types of hydrocephalus are distinguished:
- moderate external hydrocephalus - accumulation of cerebrospinal fluid passes in the subarachnoid space;
- moderate internal hydrocephalus, characterized by the accumulation of cerebrospinal fluid in the ventricular space;
- mixed replacement hydrocephalus occurs due to the accumulation of cerebrospinal fluid both under the meninges and in the ventricular space.
Internal asymmetric hydrocephalus develops when one of the ventricles of the brain expands. According to the severity of the disease, neurologists distinguish stabilized, progressive and regressive hydrocephalus.
Symptoms
For a long time, patients may not notice signs of replacement hydrocephalus. Computed tomography or magnetic resonance imaging allows you to establish the correct diagnosis. These research methods at the Yusupov Hospital are used by all patients immediately after hospitalization at the neurology clinic.
In the presence of subacute and acute occlusive hydrocephalus of the brain, patients feel a bursting headache, which is accompanied by nausea and vomiting, which brings relief. There is a feeling of pressure on the eyeballs, a feeling of “sand” in the eyes, a burning sensation in the eyeballs. With increased cerebrospinal fluid pressure, drowsiness is noted, which is a sign of disease progression.
Patients experience a feeling of “fog” before the eyes, and vision deteriorates. In the fundus, ophthalmologists identify congested optic discs. If the patient does not promptly seek qualified medical help, then an increase in the amount of cerebrospinal fluid leads to the appearance of dislocation syndrome, which threatens the patient’s life. Depression of consciousness rapidly increases, paresis of upward gaze develops, depression of reflexes, divergent strabismus develops, and coma develops. These symptoms appear when the midbrain is compressed. In the case of compression of the medulla oblongata, the voice changes, swallowing is impaired, respiratory and cardiac activity are depressed, which can lead to death.
With chronic internal hydrocephalus of the brain in adults, intracranial pressure may be normal or slightly increased. Initially, the sleep cycle is disrupted, drowsiness or insomnia appears. Patients complain of fatigue, lethargy, and memory impairment. As the disease progresses, cognitive impairment, including dementia, develops. Patients behave inappropriately and lose the ability to self-care.
Walking is impaired, the gait becomes unstable and slow. Over time, difficulty arises when starting to move, and uncertainty in a standing position. The patient can imitate cycling or walking in a sitting or lying state, but in an upright state he loses this ability. The gait becomes “magnetic”: the person seems to be glued to the floor, and, leaving his place, takes short shuffling steps on widely spaced legs. Neurologists determine an increase in muscle tone; in severe stages of the disease, paresis of the lower extremities appears and muscle strength decreases. Balance disorders may progress and the patient may become unable to sit or stand independently over time.
Subsequently, urination becomes more frequent, especially at night. There is an urge to urinate, requiring immediate emptying of the bladder. Over time, urinary incontinence develops. Neurologists at the Yusupov Hospital use the following methods for diagnosing atrophic hydrocephalus:
- magnetic resonance or computed tomography, which allows you to determine the size and shape of the cisterns of the brain, ventricles and subarachnoid space;
- radiography of the tanks, with the help of which the type of hydrocephalus is clarified and the direction of the cerebrospinal fluid flow is determined;
- diagnostic test spinal puncture with collection of 40-55 ml of cerebrospinal fluid, accompanied by a short-term improvement in the patient’s condition;
- ultrasound examination of cerebral vessels to determine the state of arterial and venous blood flow.
After analyzing the results of a comprehensive study, individual treatment is prescribed. The tactics for managing patients with severe hydrocephalus are developed at a meeting of the expert council with the participation of professors and doctors of the highest category. Neurosurgeons determine indications for surgical intervention.
Alzheimer's disease
This is a progressive disease with increasing impairment of memory, thinking, intelligence, speech, praxis and recognition, ultimately leading to dementia.
Data on the prevalence of the disease are conflicting. According to some reports, it is 4–5% among people over 60 years of age. The main clinical forms of the disease are Alzheimer's disease itself (with onset mainly in presenile age) and senile dementia of the Alzheimer's type (with onset mainly in old age). An atypical form of the disease with a predominance of frontal lobe atrophy and Alzheimer's type dementia within Down syndrome are also distinguished. Here is a description of the main forms of the disease. 1. Alzheimer's disease . In approximately 80% of cases, it begins at the age of 45–65 years, less often - at the age of about 40 or after 65 years. The duration of the disease is on average 8–10 years, possibly protracted (more than 20 years) and catastrophic (from 2 to 4 years). There are three stages of the disease.
| | Read about diagnosing and treating Alzheimer's disease |
The initial stage includes the stage of “doubtful” dementia and the stage of “mild” dementia. The first stage is manifested by mild disturbances in memory, thinking, speech, praxis, and personality, which are noticeable mainly to the patients themselves and which they manage to hide or compensate for for some time. At the stage of mild dementia, impairments become more serious. Memory for current events decreases, chronological and spatial types of memory suffer.
Violations of various thinking operations are revealed. Disorders of speech, praxis, recognition, and psychopathic personality changes are detected. The severity of the disorders is such that patients can no longer cope independently with professional responsibilities and other types of social activities, such as shopping, paying bills, receiving guests, writing texts, etc.
Patients cope with self-care, although they need outside control and encouragement. Affective and delusional disorders are often observed at this stage. These are subdepressions, sometimes chronic and combined with anxiety, hysteriform and hypochondriacal manifestations; episodic or protracted delusional ideas of damage, theft, less often - ideas of relationship, persecution or jealousy. Some patients show increased exhaustion and headaches; the duration of the initial stage ranges from 4–8 to 15–20 years. At the same time, in some patients, memory impairments predominate, while in another, larger group, focal impairments (aphasia, etc.) prevail.
At the stage of moderate dementia, impairments in the cognitive sphere and higher cortical functions reach a degree where patients can no longer cope with professional and social responsibilities. They need help even with everyday life and self-care. Neurological disorders appear, such as muscle stiffness, akinesia, hyperkinesis, and seizures. A critical attitude towards the disease nevertheless remains. Along with deficient ones, productive disorders are sometimes observed: episodes of hallucinatory confusion, a state of psychomotor agitation, often not associated with a deterioration in the somatic condition. The aphato-apracto-agnostic syndrome (three A syndrome) characteristic of this stage is finally formed, the weakening of memory takes on the character of progressive amnesia. Confabulation and ecmnesia often do not occur.
The stage of severe dementia is characterized by the breakdown of memory, thinking and intelligence, as well as higher cortical functions. Patients need help even with basic self-care. Basically, only in Alzheimer's disease are such profound disturbances, to the point of insanity, observed, as well as fetal position, contractures, multiple violent motor phenomena, violent laughter and crying, and epileptic seizures. At the same time, there are pronounced somatic changes: weight loss, extreme decrepitness, bulimia, endocrine disorders.
2. Senile dementia of the Alzheimer's type. In approximately 80% of cases, it begins between the ages of 65 and 85 years. The duration of the disease ranges from 4 to 15 years or more. In the initial stage of the disease, significant memory impairment for current events develops, often with a revival of memories of the distant past. Thinking operations suffer, as well as intelligence (creativity, planning, forecasting, etc.). Personality changes are characteristic: egocentrism, narrowing of interests, emotional impoverishment, conflict, opposition and suggestibility. Moral decline and disinhibition of drives are also observed.
The suspicion inherent in patients later develops into a tendency to develop delusions. However, half of the patients experience psychotic episodes with low-level delusions. Subdepressive states are also observed, especially gloomy depression. In the second stage of the disease, memory impairment takes on the character of progressive amnesia. There may be scanty confabulations, as well as states of amnestic disorientation with a “shift of the situation into the past.” At the stage of moderate dementia, disorders of higher cortical functions also become clear. At the stage of severe dementia, a complete breakdown of mnestic-intellectual functions is observed, and serious neurological disorders are also detected.
The etiology of Alzheimer's disease has not been established. The role of genetic factors in the development of familial forms of the disease can apparently be considered proven. However, this role remains unclear in sporadic forms, which account for about 90% of all cases of the disease. Aging is essential.
The leading place in the treatment of patients is occupied by replacement therapy aimed at overcoming neurotransmitter deficiency. To compensate for cholinergic deficiency, tacrine, amiridine, exelon, memantine, Aricept, and reminyl may be recommended. To eliminate the deficiency of other neurotransmitter systems, other drugs are recommended, in particular Yumex and Citalopram. To increase the survival of neurons, nootropics are prescribed, especially Cerebrolysin, as well as vasoactive drugs, in particular sermion or nicergoline. Anti-inflammatory treatment such as indomethacin may be helpful. Therapy for psychotic disorders is carried out with the help of antidepressants, antipsychotics, and tranquilizers. The prognosis of the disease is unfavorable.
Treatment in an adult
For increased intracranial pressure, neurologists at the Yusupov Hospital prescribe diuretics. Mannitol, mannitol and diacarb in combination with furosemide or lasix have a diuretic effect. To prevent hypokalemia, they are used simultaneously with asparkam or panangin.
To improve the nutrition of brain tissue, Actovegin, Cavinton choline, gliatilin, Cerebrolysin, Cortexin, Memoplant, Semax are prescribed. These drugs have a nootropic effect. In case of severe atrophic hydrocephalus, neurosurgeons at partner clinics perform surgical interventions.
If the patient's condition is life-threatening, craniotomy is performed and external drains are installed to allow excess fluid to escape. Medicines are administered through the drainage system. Such an operation for hydrocephalus of the brain is traumatic.
Endoscopic ventriculocisternostomy of the ventricular fundus is a minimally invasive surgical procedure. Neurosurgeons insert a microscopic surgical instrument with a camera at the end into the ventricles of the brain, which makes it possible to monitor all procedures. An additional hole is made at the bottom of the ventricle, which is connected to the cisterns of the brain. The operation allows you to eliminate the cause of the disease and normalize the physiological flow of cerebrospinal fluid between the cisterns and ventricles.
Atrophic hydrocephalus of the brain in adults is a dangerous disease that leads to irreversible changes in the substance of the brain. At the slightest suspicion of hydrocephalus, call the Yusupov Hospital. After the examination, neurologists will prescribe treatment to slow the progression of hydrocephalus symptoms.
Clinical manifestations and diagnosis of the disease
Symptoms of cortical atrophy of the brain directly depend on the degree, site of damage and extent of the pathology. Cortical cerebral atrophy has five stages of development of the destructive process with its own characteristic features. It is also important to consider where exactly the harmful changes occur - in the cortex or in the subcortical zones. The first manifestations of the main signs of the disease depend on this. Depending on age and external factors, pathological changes may develop faster. The disease has the following stages of development:
- Grade 1 cortical cerebral atrophy usually occurs without any symptoms. From time to time there is a headache, weakness, and dizziness. This stage of the disease develops very quickly and moves into the next one.
- The second stage of pathology is characterized by the fact that a person becomes irritable, cannot calmly accept criticism, conflicts with the environment, and easily loses the thread of communication. Memory deteriorates, handwriting may change, old habits are forgotten and new ones are acquired. At the second stage of atrophy development, you can notice a disturbance in the coordination of movements and changes in gait. The patient may begin to copy other people, as his independence in thinking and movements is lost. The second stage should alert loved ones and encourage them to seek help from a specialist.
- Loss of control over behavior, sudden outbursts of anger, despondency are characteristic features of the third stage of the destructive process. Basic self-care skills are lost.
- In the last stages of the disease, a person reacts inadequately to the world around him, loses awareness of what is happening, and does not show any emotions.
A person in the last stage of pathology is often dangerous to society, and therefore such people may be isolated in a psychiatric or neurological clinic. The most famous pathology of the cerebral cortex is bihemispheric cortical atrophy (destructive changes occur in both hemispheres at once). This disease is better known as Alzheimer's disease. Another type of atrophic disease of brain tissue is Pick's disease, in which thinning of the cerebral cortex is observed. Its main symptoms include: inability to concentrate, increased distractibility, gluttony, hypersexuality. The pathology develops slowly, but progresses steadily. Unlike Alzheimer's disease, Pick's disease is treatable when detected early in its development.
Pathological changes in the cerebral cortex and the degree of damage can be diagnosed using additional studies, as well as computer or magnetic resonance therapy, the indications for which are the main symptoms of a possible disease. Dopplerography of the vessels of the neck and brain, and cognitive tests (to determine the stage of the pathology) are also performed. To identify neoplasms and lesions with structural changes, the patient undergoes X-ray examinations. The most accurate diagnostic method today is magnetic resonance therapy, which allows not only to identify pathological changes in brain tissue in the early stages of the disease, but also to monitor them over time.