Alpha rhythm depression
➥ Main article: Alpha rhythm depression
Alpha rhythm depression (lack of alpha waves) occurs when a person opens his eyes or thinks about a task that requires certain visual representations. With an increase in the functional activity of the brain, the amplitude of the alpha rhythm decreases until it disappears completely. Can also be a sign of worry, anger, fear, anxiety, causing depression; disorders associated, to one degree or another, with changes in the activity of the activating systems of the brain and, as a consequence, with an increased level of activation of the autonomic and central nervous systems.
Criteria for pathology when assessing α-rhythm
Disturbances of a functional or morphological nature primarily affect the parameters of the α rhythm.
- The constant presence of the α-rhythm (index >50%) in the frontal regions of the brain during bipolar recording from electrodes placed with small interelectrode distances (Fig. 2; 3).
- Amplitude interhemispheric asymmetry >30% (Fig. 4).
- Frequency asymmetry >1 oscillation/s (Fig. 5).
- Violation of the image: violation of sinusoidality of waves, lack of modulation, appearance of paroxysmal rhythm (Fig. 4, 6, 7). Presence of an arched α-rhythm (Fig. 6, 7).
- Changes in quantitative parameters, lack of stability in frequency, decrease in amplitude <20 μV or increase >90 μV, decrease in α-rhythm index <50% up to its complete absence (Fig. 5).
Rice.
2. Male, 45 years old. Cyst of the right temporal region. The electroencephalogram shows the constant presence of the α-rhythm (index >50%) in the frontal regions of the brain, the absence of modulation, the appearance of a paroxysmal α-rhythm, and a violation of the sinusoidality of the waves (A - monopolar montage; B - longitudinal bipolar montage)
Rice. 3. Woman, 60 years old. Panic attacks, sudden mood changes.
The electroencephalogram shows an amplitude interhemispheric asymmetry of the α rhythm >30%, a decrease in zonal differences, a violation of sinusoidality, and the presence of paroxysmal α waves
Rice. 4. Male, 16 years old. Cyst of the right anterior region.
The electroencephalogram shows amplitude interhemispheric asymmetry of the α rhythm >30%, lack of modulation, and the appearance of paroxysmal α waves
Rice. 5. Boy, 12 years old. Absence seizures.
The electroencephalogram shows a lack of stability in frequency, frequency asymmetry of the α-rhythm >1 oscillation/s, lack of modulation, disturbance of sinusoidality of waves, increased amplitude >90 μV
Rice. 6. Woman, 23 years old. Cyst of the right anterior region.
The electroecephalogram shows the constant presence of the α-rhythm in the frontal-central-parietal regions of the brain, the absence of modulation, and the appearance of an arched α-rhythm
Rice. 7. Woman, 63 years old.
Complaints of severe headaches and increased blood pressure. An electroencephalogram reveals the presence of an arched α-rhythm in the occipital regions of the brain and the absence of modulation. Doppler ultrasound revealed a circulatory disorder in the middle cerebral artery on the left
Gamma rhythm
Recently, electrophysiologists believe that most mental processes are associated with the highest frequency EEG rhythm - the gamma rhythm (30 - 40 Hz and above). It is believed that the high-frequency gamma rhythm, detected through neurophysiological studies and occurring synchronously in different areas of the brain at a certain level of functioning of neurotransmitter systems, underlies cognitive processes.
Gamma rhythm is a reflection of the formation and development of interconnected neural ensembles that play an important role in cognitive processes.
In schizophrenia, the localization of the maximum of gamma activity differs markedly from the norm. Already during the first episodes of psychosis, when performing a cognitive test, patients with schizophrenia demonstrate an excess of the spectral power of the gamma rhythm only in the prefrontal areas, which at more distant stages of the disease is replaced by its insufficiency, a reduction in power throughout the right hemisphere.
Functional interhemispheric connections in patients with schizophrenia are weakened both in the background state and when performing cognitive tests.
Of interest are works devoted to interhemispheric asymmetry and dominance of the activity of any of the brain hemispheres.
Magnetic encephalographic studies aimed at analyzing the activity of the left and right hemispheres of the brain using acoustically evoked neuromagnetic fields showed changes in dipoles in the region of the superior temporal gyrus. More pronounced deviations concerned not local changes, but the orientation of the dipoles. In men suffering from schizophrenia, distinct changes in the orientation of the dipoles were noted in the left hemisphere, in women - in the right. The results of similar studies indicate sex differences in the activity of the cerebral hemispheres in patients with schizophrenia (Sauer H. et al., 1998).
The results of electrophysiological and neuropsychological studies indicate that in schizophrenia, the pathological process predominantly involves the prefrontal and posterior frontal (premotor) parts of the brain and the associated deep structures of the reticulofrontal complex.
Complete absence of alpha rhythms
In 1949, Moizzi and Magoun first showed that stimulation of the brainstem reticular formation activates the cortex and converts high-amplitude, low-frequency EEG (ie, EEG with prominent alpha rhythms) into low-amplitude, high-frequency EEG. In a normal brain, EEG alpha rhythms have the greatest amplitude. When alpha rhythms are absent, the EEG recording appears and is called low amplitude. If higher-frequency rhythms are not suppressed compared to normal, the EEG recording is called low-amplitude high-frequency EEG. In the power spectra of such EEGs there are no significant peaks of alpha frequencies in any state (both with open and closed eyes). Empirically, low-amplitude recording, defined as recording in the eyes-open and eyes-closed states with an EEG amplitude in a montage relative to the integrated ear electrodes, is no more than 20 μV in all cortical areas. As you can see, this definition is very subjective and very broad.
Low-amplitude EEGs are found in 4–10% of healthy adult subjects, depending on the evaluation criteria, and are unlikely to be considered abnormal. Rather, low-amplitude EEGs may be associated with some individual characteristic. Low-amplitude EEGs were found in families of alcoholics and drug addicts. Alcohol consumption appears to act as a "self-medication" in this population to reduce cortical hyperactivation.
Interhemispheric connections
Numerous studies have shown disturbances in the structure and functional activity of the corpus callosum in schizophrenia . Interhemispheric interaction is largely determined by cerebral lateralization or asymmetry. It is an evolutionarily newer and highly organized function of the brain, at the same time more vulnerable to pathological processes.
As is known, interhemispheric interaction is formed on the basis of cerebral lateralization in the process of normal brain development. Here, nutrition, adequate stimulation, hormonal levels, and the absence of significant stress both in the peri- and postnatal periods of the child’s development play an important role. In addition, cerebral lateralization determines the structure and size of the corpus callosum, and later the nature of interhemispheric interactions. Analysis of coherence in the gamma range showed that the complete absence of functional interhemispheric interactions in the early stages of schizophrenia is subsequently replaced by the formation of a system of interhemispheric interactions in the posterior regions of the brain. This may indicate the development of compensatory processes in the work of neural ensembles of the brain. It is a fair assumption that in schizophrenia, interhemispheric connections (interhemispheric exchange of information) are carried out not through the corpus callosum, as is normal, but through subcortical structures (Strelets V.B. et al., 2006).
The absence of interhemispheric interactions, the phenomenon of “functional splitting of the hemispheres,” is detected already in the first episodes of the disease.
We can talk about a violation of the integrative activity of the brain in schizophrenia, which, in a limited range at distant stages of the course of the disease, is possible only in the posterior parts of the hemispheres.
During an exacerbation of schizophrenia against the background of pronounced positive symptoms, the number of coherent connections, reflecting the degree of synchronization of different areas of the cortex, is significantly reduced. Interhemispheric interaction is practically absent. With pronounced negative symptoms against the background of a sharp decrease in cortical interaction, another system of connections is probably formed compensatory - only in the posterior regions of the brain (including one interhemispheric one). Patients with schizophrenia at late stages of the disease retain the ability to perform cognitive tests, not due to interhemispheric interaction at the level of the corpus callosum, which is destroyed in schizophrenia, but due to interhemispheric interaction through subcortical structures. Therefore, patients with schizophrenia perform tasks more slowly than healthy people (Strelets V.B. et al., 2006).
The results of neurophysiological studies allow us to put forward a hypothesis according to which the brain of patients with schizophrenia operates in a distorted functional state, which is characterized by excessive fractal dimension. This can lead to impaired coordination between different areas of the cerebral cortex, sensory overload, and specific disorders of thinking and the affective sphere. In addition, patients with unfavorable schizophrenia have difficulty forming automatic responses to repeated stimuli.
α-rhythm disorganization
Disorganization is a general change in the frequency composition, shape, topography and/or number of physiological EEG rhythms in a separate recording in relation to the previous EEG recording of the same subject or rhythms in the same areas of different hemispheres of the head. Disorganization or sharpening of the alpha rhythm, dysrhythmia are considered as a manifestation of irritative disorders, which are most often associated with a reflex influence from the irritated membranes of the vascular system of the brain. In the initial and shallow stages of coma, characterized by confusion, drowsiness, partial loss of contact with the environment, sometimes defined as stupor, disappearance or significant disorganization of α-activity and the appearance of θ- and δ-waves with an amplitude of up to 50-60 μV are observed.
Electrooculography
Quite informative for schizophrenia is a test with antisaccades , determined based on the appearance of horizontal saccades when tracking the movement of a light stimulus from the periphery to the center - to a point symmetrical to the target relative to the center of the visual field.
The antisaccade test can be recorded not only during electrooculogram (EOG) recording, but also using infrared oculometry.
Normally, the eyes move smoothly and in a sinusoidal orbit. In schizophrenia, especially in patients suffering from this mental disorder for a long time, and in some chronic psychoses, eye movements are interrupted by frequent stops, and “catch-up saccades” appear.
During the examination, the patient must follow the light stimulus on the pendulum with his eyes, while the pendulum swings first slowly, then faster. The transition from sequential eye movements to saccadic - spasmodic, leading in healthy people is from 0.5 to 0.7 Hz; in patients with schizophrenia, an earlier and more noticeable appearance of saccades is observed even during remission, which is associated with attention deficit and process disorders perception - the inability to record weakly expressed and short-term signals. The inability of patients with schizophrenia to smoothly follow the movement of a pendulum is a consequence of emerging difficulties in differentiating stimuli, in particular, significant from latent ones.
In patients with schizophrenia, when performing this test, 5-6 times more errors are recorded than in healthy individuals.
| | Timely diagnosis contributes to effective treatment of schizophrenia |
Impaired smoothness and intermittency of tracking eye movements is a diagnostically significant sign of schizophrenia, noted in almost 80% of cases. According to data from researchers from different countries, to some extent, disturbances in the smoothness of eye movement differ among different nations. Due to the above, in the specialized literature one can find a wide range regarding the diagnostic significance of the results of this test (70-90%).
This test is also positive in relatives of patients with schizophrenia, which may indicate its informativeness regarding the genetic characteristics of schizophrenia (Kirenskaya A.V., 2006).
Multiple stops during eye movements are observed in 45% of first-degree relatives of patients with schizophrenia, and this test is more often positive in monozygotic twins than in heterozygous twins, and is normally recorded in only 10% of people (Mather J., 1985).
Experiments on animals in which certain areas of the frontal lobe of the brain were damaged showed that dysfunction of the frontal cortex leads to disruption of the processes of specific inhibition emanating from the frontally localized visual fields to the subcortical centers responsible for eye movements.
This hypothesis was confirmed and somewhat modified using the method of functional magnetic resonance imaging. It turned out that during saccade inhibition, when patients were asked to stop tracking a light stimulus located in the periphery, the subcortical center of the striatum did not increase its activity, as was observed normally. Based on the data obtained as a result of such an experiment, it can be assumed that in schizophrenia there is a primary dysfunction of the striatum, which locally disrupts the frontostriatal flow of information. In other words, the process of switching neural connections in the striatum is disrupted. In part, this hypothesis is confirmed by data from psychopharmacological and neurochemical studies of schizophrenia, indicating that blockade of D2 receptors in the striatum significantly improves the condition of patients with schizophrenia. In addition, the study of indicators of the level of metabolic processes in the striatum in schizophrenia indicates a decrease in the percentage of metabolism in this area.
Most likely, in schizophrenia we are dealing with damage not only to the striatum, but also to other areas of the brain. The pathological process can be represented as an extensive network disorder, manifesting itself in the form of impaired switching functions between the frontal region of the brain, striatum and thalamus. According to this hypothesis, the “inhibitory signal” is impossible due to damage to the neuronal connections between the frontal lobe of the brain and the thalamus. It should be noted that similar changes in a number of cases are observed in other mental disorders, which undoubtedly affects the boundaries of schizophrenia, even at the level of its pathogenesis.
Alpha rhythms in unusual areas
In children and young adults, alpha EEG activity can be detected in the occipital regions (O1, O2), parietal region (Pz) and in the sensorimotor zone (SZ, C4). However, the scalp distribution of alpha activity (especially in the eyes-open state) changes with age, and temporal alpha rhythms become prominent in older adults. Niedermeyer (1997) described a temporal alpha-like rhythm, found mainly in the anterior and midtemporal regions, characterized by mild abnormality, and suggested that it may be a sign of early cerebrovascular disorders. He also mentions that during puberty, this pattern, found in the temporal lobe, may obscure the focus of epileptogenesis. Rhythmic alpha activity may also mask rhythmic paroxysmal bursts without evidence of any acute components.
Figure 8. Case of abnormal localization of alpha-like rhythms
Top left: EEG fragment in the eyes-open state. Deviations from the norm of EEG spectra and corresponding topograms are presented. Below are sLORETA images of abnormal rhythm generators.
Our experience of working with healthy subjects and patients allows us to draw the following conclusion: if in an individual patient: 1) the maximum of rhythmic activity within the range of 7-13 Hz is localized in leads different from those mentioned for the norm, 2) the rhythm itself is so noticeable that there is a significant deviation from the norm in both absolute and relative power - then this rhythm can be considered abnormal. In our practice, the maximum distributions of abnormal alpha rhythms were found in the posterior temporal areas (for example, in connection with tinnitus or spinal injury), in the parietal areas of the left hemisphere (in connection with dyslexia), in the middle and anterior temporal areas (in connection with with age-related cerebrovascular disorders). Only in a few cases were abnormal alpha rhythms found in the frontal regions.
An example of the spectral characteristics of the EEG of a patient with abnormal alpha rhythms is presented in Fig. 8. The raw EEG recording shows two types of rhythms within the alpha frequencies: the first with a frequency of 9.5 Hz, located in the left middle temporal region, and the second with a frequency of 7.3 Hz, located in the Fz lead zone. The results of comparison with the normative database and sLORETA images are presented in Fig. 8 top right.
In general, changes in the normal functioning of thalamocortical pathways can result in a number of neurological disorders, such as epileptic seizures and tremor in Parkinson's disease, both of which have rhythmic components. Stimulation or destruction of the relevant part of the thalamus (for example, the ventral nucleus zones) is one of the accepted methods for alleviating tremor, apparently associated with the destruction of the rhythmic activity of thalamocortical networks. Abnormal rhythmic activity of thalamic cells (as shown in patients with implanted electrodes) can be observed in some neurological disorders associated with behavioral disorders that are not necessarily rhythmic in nature. For example, recordings of thalamic neuron activity in patients suffering from chronic pain as a result of sensory deafferentation (so-called phantom pain) demonstrate the presence of abnormal rhythmic bursts of action potentials. In this case, stereotactic lysis of the thalamic nuclei leads to a reduction in phantom pain.
Characteristics of the alpha rhythm of the electroencephalogram in patients with bronchial asthma
Approximately 300 million people in the world are diagnosed with bronchial asthma (BA) [1]. At the same time, the incidence continues to increase, and by 2025 the population of patients with asthma is expected to increase by another 100 million people [1, 2]. Prevalence in different age groups, a progressive increase in morbidity and treatment costs lead to an increase in the burden of this disease both for the health care budget and for society and the patients themselves, which makes asthma a significant medical and social problem [1-3]. At the current level of evidence-based medicine, a systematic approach to the problem of asthma is possible only on the basis of interdisciplinary research at the intersection of various fields of knowledge - pulmonology, psychiatry, physiology, psychophysiology, neuropsychology, sociology. A certain scientific and practical breakthrough is needed in this direction, which will allow us to get closer to the development of personalized medicine methods necessary for AD.
AD has been treated for many years as one of the classic psychosomatic diseases. Without delving into the history of the issue of transformation of the very concept of “psychosomatic diseases” and previous interpretations in this aspect of AD, we can state that, according to modern ideas, AD is an independent nosological form. BA is a chronic inflammatory disease of the airways, characterized by reversible bronchial obstruction and bronchial hyperresponsiveness.
The emergence and progression of AD can serve as an example of complex psychosomatic and somatopsychic relationships and interconnections [4]. In the overwhelming majority of cases, at all stages of AD development, the presence of psychopathological disorders of the affective spectrum, most often the anxiety-depressive complex, is noted to one degree or another. The degree of severity of psychopathological inclusions in the main clinical picture of the disease creates additional difficulties in the treatment of patients with AD. One of the approaches to an objective assessment of the disorganization of the functional state of the cortical mosaic of the central nervous system is the analysis of the electrical activity of the brain, especially the main EEG rhythm - alpha activity [5, 6].
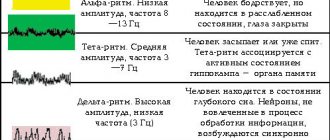
Numerous studies have shown that the development of depressive states is accompanied by disturbances in the structure of all frequency ranges of the EEG, but to a greater extent changes concern the main EEG rhythm - the alpha rhythm [7-10]. Alpha rhythm is a rhythmic oscillation with a frequency of 8-13 Hz and an average amplitude of 30-70 µV, recorded mainly in the occipital regions with eyes closed in a state of quiet wakefulness and the maximum possible muscle relaxation. The rhythm is blocked by light stimulation, concentration and mental stress.
The alpha range in depression can significantly increase or decrease, and the spatial distribution of the rhythm changes [8, 11-13]. According to modern concepts, the generation of the alpha rhythm is associated with the reverberation of impulse activity along the intercortical and thalamo-cortical neural networks, and its severity determines the synchronization of the functional activity of various brain systems, in particular, it determines the connection of information received from the afferent system of the body with the mechanisms of RAM, regulating adaptive processes.
Therefore, the alpha range of the EEG has traditionally attracted increased attention from researchers due to its high sensitivity to various external influences and subtle changes in the functional state of the cerebral cortex that accompany sensory, motor, cognitive and mnestic processes [14, 15].
The nature of changes in alpha activity in depressive disorders depends primarily on the characteristics of the depressive syndrome. Thus, an increase in the alpha rhythm index is characteristic of patients with “major depression,” and its decrease in the desynchronized type of EEG is detected in dysthymic disorders, i.e., in depression of a neurotic level [16-18]. A number of authors have proposed a neurophysiological model of depression that postulates a change in frontal asymmetry—a decrease in left hemisphere activity [19-25]. Researchers associate the features of changes in alpha activity with the dominance of melancholy, anxious or apathetic affect, thereby confirming the generally accepted position about the connection between the structure of the EEG and the functional activity of cortical zones. The observed features of the profile of the autonomic nervous system suggest that one of the mechanisms of restructuring of cortical rhythms is dysfunction of diencephalic subcortical structures [26].
Purpose of the study: to conduct a comparative analysis of the parameters of the basic human EEG rhythm - the alpha rhythm - in patients with asthma and healthy people.
MATERIALS AND METHODS
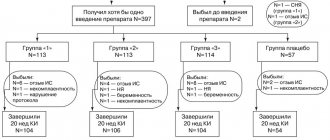
Subject to voluntary informed consent, 57 patients (38 women and 19 men) with partially controlled mild to moderate asthma and affective spectrum disorders participated in the study. The diagnosis of asthma was established in accordance with international consensus documents (Global Initiative for Asthma, 2017). The age of the patients ranged from 18 to 65 years (mean age: 53.7 ± 10.9 years). The control group consisted of 50 practically healthy individuals matched by age and gender.
A comprehensive clinical and instrumental examination was carried out: functional examination of the lungs (spirometry, respiratory function), EEG. To assess and analyze psychopathological disorders of the affective spectrum, we used a clinical-psychopathological map developed by V.N. Krasnov [27]; Hamilton Anxiety and Depression Scales; BA test control.
The general psychopathological characteristic of the examined AD patients was hypothymia with an anxious component, and there was a tendency for anxiety to transform into an anxious-melancholy state. The Hamilton Depression Scale score was 13-17.
Literary data indicate different profiles of neurophysiological indicators in right-handers and left-handers, therefore, according to the lateral traits questionnaire [28], right-handers were selected into the groups of subjects.
The EEG was recorded using a hardware-software complex for topographic mapping of electrical activity of the brain “Neuro-KM” (Russia) with a bandwidth from 0.1 to 45 Hz. EEG recordings were carried out monopolarly from symmetrical frontal (F3, F4), central (C3, C4), parietal (P3, P4), occipital (O1, O2), anterior temporal (F7, F8), middle temporal (T3, T4) ) and posterior temporal (T5, T6) cortical zones (scheme 10-20%, even lead channels are from the cortical zones of the right hemisphere, odd lead channels are from the left hemisphere). Integrated ear clips served as the reference electrode. The characteristics and topographic distribution of EEG rhythms were determined using EEG analysis using the fast Fourier transform method with averaging of at least 30 epochs of 2 seconds each, followed by mapping using the BRAINSYS system (Russia).
Spectral and coherence EEG analyzes were performed. The magnitude of coherence (COG) was calculated between all 14 leads of cortical areas in the range of 7-13 Hz, as well as in steps of 1 Hz. The value of average coherence (AmCOG) of each region with all other cortical zones was also determined - an indicator of the functional activity of the selected zone in the integral activity of the brain. In the intergroup comparative analysis of the spectral power (SP) of rhythms, we used the reduction of indicators to a normalized type through logarithmization (LnCM), and comparison of COG parameters was carried out according to the formula:
where KOG2 is the square of the KOG module.
RESULTS AND DISCUSSION
Data from visual and spectral analyzes of the electroencephalogram
The most pronounced changes in the background EEG of the examined patients were observed in the form of two variants: low-amplitude dysrhythmia and increased synchronization in the slow-wave ranges. In the first case, there was a decrease in the amplitude of bioelectrical activity, a reduction in the alpha rhythm, a smoothing of regional differences in the alpha index, and an increase in diffuse low-amplitude slow-wave activity. In the second option, there were bilateral bursts of alpha and theta waves, arising synchronously in all areas and indicating irritation phenomena at the level of brain stem structures. A characteristic feature of the alpha rhythm is the weak expression or complete absence of modulation in the spindles.
Regardless of the type of changes, EEG mapping of group spectral characteristics of the EEG revealed violations of the main rhythm topic - zonal differences in the alpha index were weakly expressed. Despite the fact that only right-handers were included in the study group, the focus of the alpha rhythm in the examined patients was unclearly defined in the right occipital region, which is typical for the norm, and in some cases dominated in the occipital region of the left hemisphere, which indicated a more significant decrease in functional activity left hemisphere.
In the spectral analysis of the EEG, the absolute SM of the alpha rhythm in patients was lower than in subjects in the control group in all EEG leads. A diffuse decrease in the SM of the alpha rhythm led to the fact that, when compared with other EEG rhythms, the SM of the alpha rhythm did not lead, but occupied a position after the SM of slow-wave rhythms, more often after the theta range.
Changes in the ratios of individual EEG rhythms in patients with AD can be especially clearly seen when analyzing %SM - the percentage of the alpha rhythm from the total SM of all EEG rhythms in a given cortical area.
Figure 1 shows the difference in %SM between the indicators in patients and subjects in the control group. In all cortical zones, the decrease in %SM of the alpha rhythm was more than 12%. The most significant reduction (about 20%) was in the occipital regions with an emphasis in the right hemisphere, which was reflected in the leveling of zonal differences in cortical zones in the severity of the alpha index.
Rice. 1. Differences between the % spectral power of the alpha rhythm in patients with bronchial asthma and the norm (p < 0.05 with a modulus of 1.7)
In patients, there was a shift in the modal value of the CM of the leading rhythm to a lower frequency range - 8-9 Hz (versus 10 Hz in healthy subjects), which reflects the transition of cortical rhythms to functioning in more energy-saving modes (Fig. 2). The next highest SM values in the alpha range were the bands 9-10 and 10-11 Hz, and the lowest were the high-frequency bands 11-12 and 12-13 Hz. The average SP for all cortical zones (SrSM) of high-frequency components of the alpha rhythm is 4 times lower than the SrSM of the dominant frequency of 8-9 Hz.
Rice. 2. Alpha rhythm structure - average values of 1 Hz bands of spectral power (SP) for all leads
Compared with the indicators of the control group (Fig. 3), in patients with asthma the 8-9 Hz band was reduced to a lesser extent than the others. The greatest reduction of the 10-11 Hz band was observed in the occipital regions with a slight emphasis in the right hemisphere. In these cortical areas, the 9-10, 11-12 and 12-13 Hz bands were reduced almost equally. In the frontal cortical zones, the pattern is different - the 9-10 Hz band is reduced to a greater extent, followed by the 10-11, 11-12 and 12-13 Hz bands. These data indicate a significant deformation of the structure of the basic rhythm in patients. Alpha rhythm generators in patients operate in a special mode, significantly different from the norm.
Rice. 3. Changes in the structure of the alpha rhythm in patients with bronchial asthma compared to the norm in the frontal (F3 on the left and F4 on the right) and occipital (O1 on the left and O2 on the right) areas of the cortex (p < 0.05 with a modulus of 1.7)
Electroencephalogram coherence analysis data
The lowest COG values in patients with asthma were found in the ranges of long-distance connections. Thus, the fronto-occipital COG values (O1-F3, O1-F4, O2-F4 and O2-F3) fluctuated in the range of 0.05-0.08. Short-distance connections had significantly higher COG values: occipital areas with parietal zones (O1-P3, O2-P4) - 0.34 and 0.48, frontal areas with nearby areas (F3-C3, F4-C4) - 0.75 and 0.74. The value of SRCOG in the alpha range in patients with AD compared with that in participants in the control group (Fig. 4) in all cortical zones was significantly reduced (p < 0.05).
Rice. 4. Comparison of the average coherence value (AmCOG) in the alpha range in patients and control group subjects
In the frontal, central and parietal zones of both hemispheres the decrease reached a factor of one and a half, and in the temporal zones it was slightly less. The largest difference between the normal group and patients was found in the occipital and posterior temporal zones, in particular in the left occipital region - the alpha band average in patients was almost 2 times lower than in healthy people.
The data obtained indicate a significant diffuse weakening of functional connections between all areas of the cortex. This also applies to interhemispheric connections; they are reduced between all symmetrical cortical zones according to the basic rhythm, although to varying degrees. Thus, between the frontal zones the differences from the norm are less pronounced than between other pairs of cortical areas. A particularly significant decrease in interhemispheric interaction is observed between the anterior, middle and posterior temporal zones. The role of individual frequency bands of the alpha rhythm in connections between cortical zones is not the same - the main role is played by the low-frequency band of 8-9 Hz. The SRCOG values of this band are greatest in the frontal, parietal-central zones, as well as in the temporal zones of the right hemisphere. Consequently, in patients with asthma, the restructuring of the basic rhythm structure into slower modes changes and reduces the functional activity of cortical zones.
The conducted clinical and neurophysiological study confirms the presence of moderate anxiety-depressive disorders concomitant with AD with a tendency to form a melancholy variant of the affective spectrum, which may be indicated by an increase in slow-wave activity, mainly in the theta range.
CONCLUSION
The study of the EEG alpha rhythm using spectral and coherence analysis made it possible to identify a special mosaic of spatio-temporal relationships between the work of various parts of the cortex and intercortical interactions in patients with bronchial asthma (BA). This allows for a differentiated approach to assessing the functional activity of various cortical zones and their participation in the integrative activity of the brain based on spectral and coherent indicators of the alpha range. These indicators can serve as additional characteristics in the diagnosis and selection of therapeutic approaches in patients with asthma.