Nerve damage can occur as a result of injury, as well as as a result of diseases, intoxication, circulatory disorders and many other reasons.
Whatever the damage is caused, the result is always a partial or complete disruption of the main function of the impulse-conducting nerve, and, as a result, peripheral paresis and sensory impairment develop in the area that the nerve innervates. The objectives of rehabilitation for nerve injuries will primarily be to create optimal conditions for nerve regeneration, maintain the functioning of denervated muscles, and, when restoring impulse conduction, train weakened muscles and restore movements.
Get advice from a rehabilitation specialist or make an appointment
+8
Record
Types of damage
Damage to the nerves of the hand is represented by the following groups.
- Complete rupture of a nerve is called neurotmesis. Surgical treatment is indicated. Recovery occurs over months or years depending on the severity of the damage.
- Partial rupture accompanied by various disorders - neuropraxia - occurs with closed injuries. A condition with preserved nerve sensitivity, when the lack of conduction is temporary.
- Neuropathy is a disorder resulting from a fracture, bruise or cut in the hand area.
- A pinched nerve occurs when the patient cannot bend the wrist. The little finger is completely immobilized, the ring finger is partially immobilized, the thumb moves with difficulty. The pain radiates to the little finger.
The article describes a clinical case of treatment of a patient with damage to the ulnar nerve using the “gold standard” of microsurgery – autoneuroplasty – supplemented by transplantation of autogenous cells of the stromal vascular fraction of adipose tissue (SVF-AT). The 5 cm long nerve defect was replaced with three autonerve inserts from the sural nerve, and then SVF-AT cells were transplanted using fibrin glue.
1 year after the operation, the patient had restoration of the function of adduction of the fingers, absence of neurogenic deformation of the hand, atrophy of the muscles of the hand, as well as restoration of sensitivity in the autonomous zone of innervation of the ulnar nerve.
Post-traumatic restoration of peripheral nerves is still an urgent problem. Despite the widespread use of various approaches and methods of treatment associated with the use of microsurgical techniques, the accumulated experience in treating this category of patients, the degree of disability of patients remains quite high[1].
As practice shows, if it is impossible to suture the nerve end to end, autonervoplasty is indicated - the “gold standard” of microsurgery. All clinical and experimental studies of new approaches in this area are compared specifically with autonervoplasty. Autonervoplasty gives satisfactory results compared to other methods of eliminating nerve trunk defects[2, 3]. The sural nerve, as well as the medial and lateral cutaneous nerves of the shoulder and forearm, and intercostal nerves are most often used as donor nerves. At the same time, depending on the thickness of the damaged nerve and the number of fasciculi, the number of donor nerves is selected. However, the disadvantage of this method is that in the presence of a nerve defect measuring 5 cm or more, necrosis and death of the graft is possible due to its insufficient vascularization, which leads to an unsatisfactory result in restoring the motor and (or) sensory function of the limb. The use of cellular technologies to stimulate revascularization and, as a consequence, regeneration of peripheral nerves seems promising [4].
The safest method of stimulation is the use of autogenous cell material without prior cultivation. In particular, these can be red bone marrow cells, various types of stem and progenitor cells from peripheral blood, as well as cells of the stromal vascular fraction of adipose tissue (SVF-AT)[5].
Conducted studies indicate the effectiveness of autotransplantation of multipotent mesenchymal stromal cells (MMSCs) of adipose tissue in the restoration of peripheral nerves in experimental studies [6, 7]. Fibrin glue “Tissucol® Kit” (Baxter AG, Austria) seems promising as a biodegradable carrier for cells, which is currently successfully used in clinical practice during operations on the parenchyma of the kidneys, liver, spleen, pancreas; skeletal bones and peripheral nerves[8].
In this article, we review a clinical case of the combined use of SVF-VT cells and autonervoplasty of the ulnar nerve.
Material and methods
Patient P., 26 years old, was admitted to the clinic on August 19, 2011 with a diagnosis of consequences of damage to the ulnar nerve in the upper third of the left forearm. On July 29, 2011, the patient received a domestic injury (cut by window glass). On the same day, primary surgical treatment of the wound was performed at the central regional hospital at the place of residence. The wound healed by primary intention, the sutures were removed after 14 days. after surgery, after which the patient was sent to a specialized department.
According to the clinical examination: the skin of the left upper extremity is of physiological color, a post-traumatic retracted irregularly shaped scar 12 cm long was identified on the anterior surface of the upper 1/3 of the forearm. On palpation in the scar area, characteristic “shooting” pains were observed radiating to the 4th and 5th fingers left hand.
Assessment of trophic disturbances
A. Condition of the skin: the color is normal, the temperature of the fingers is slightly reduced. The skin pattern on the pads of the distal phalanges of the 4th and 5th fingers is smoothed.
B. Atrophy of the muscles of the hand and forearm compared to a healthy hand: average degree – deficit of 1.5–2 cm, there was no adduction/abduction function of the 5th finger of the left hand, neurogenic flexion contracture of the 4th and 5th fingers of the left hand was observed.
B. Nail changes: no
G. secretory function (sweating): decreased.
Study of sensitivity in a patient in the autonomous zone of innervation (finger 5) To assess sensitivity in the zone of innervation of the ulnar nerve, standard methods of clinical neurological examination were used. The absence of pain, temperature, tactile, discriminatory sensitivity, the absence of stereognosis, feelings of pressure and mass were revealed. Examination of motor function It was revealed that there was no adduction/abduction of the 5th finger, and the inability to fully extend the 4th and 5th fingers of the left hand.
Additional research methods
According to ultrasound, in the upper third of the left forearm in the scar projection there was a complete break of the ulnar artery and ulnar nerve with the presence of a neuroma in the central segment measuring 1x1.5 cm. The nerve defect, presumably excluding the neuroma, was 4–4.5 cm.
According to electroneuromyography (ENMG), the following was revealed: 1) the presence of a conduction block along the ulnar nerve (it was not possible to register a motor response from the muscles of the hypothenar group in response to stimulation of the ulnar nerve at the stimulation point above and below the site of injury, the speed of propagation of excitation (SPT) along the motor fibers also failed to register); 2) local damage to the ulnar nerve; damage to the median and radial nerves was excluded. The study assessed the muscles on the injured side, as well as symmetrical muscles on the unaffected limb. To determine the degree of denervation-reinnervation process in the muscles, the amplitude-time parameters of the M-responses of the hand muscles, as well as the SRV along the motor fibers of the ulnar nerve, were studied.
Based on the anamnesis, clinical data, as well as the results of ultrasound and ENMG, a decision was made to perform an operation: autonervoplasty of the ulnar nerve with the sural nerve with autotransplantation of SVF-VT cells.
The patient signed a voluntary informed consent to perform the operation and participate in the study approved by the Ethics Committee within the framework of the theme of the State Autonomous Healthcare Institution "Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan" "Improvement and development of new treatment methods for patients with damage to the brachial plexus and peripheral nerves."
Operation protocol
Under local anesthesia, a lipotome was used to collect 100 ml of adipose tissue from the anterior abdominal region. Next, SVF-AT cells were isolated in laboratory conditions according to a previously described method [9, 10]. 5 million cells were obtained.
Simultaneously with the isolation of the fraction, the scar in the upper third of the left forearm was excised under general anesthesia, and an additional S-shaped incision was made. The ulnar nerve was visualized, its complete damage and compaction of the proximal and distal ends were revealed. The proximal end had a pronounced neuroma, measuring 1×1.5 cm. After excision of the pathologically changed ends of the damaged nerve, the diastasis was 5 cm.
Under local anesthesia, a 18 cm long sural nerve graft was harvested from the right leg. Autonervoplasty of the ulnar nerve was performed using three sural nerve inserts using Prolen 9/0 surgical thread. Then, transplantation of SVF-AT cells was performed using fibrin glue “Tissucol® Kit” (Baxter AG, Austria), applying the material to the ends of the peripheral and central segments of the nerve and to each insert (Fig. 1).
In the postoperative period, the following conservative therapy was prescribed: vitamins B1, B6 – 1.0 IM, 1 time per day, for 14 days; Prozerin 1.0 IM, 1 time per day for 14 days, Trental 10.0 + 200 ml of 0.9% NaCl solution intravenously, 1 time per day for 7 days; Ceftriaxone 1.0 1 time per day IM for 7 days. In the postoperative period, the patient was observed for periods of 6 weeks, 3 months, 6 months, 9 months, 1 year, 2 years, 3 years.
Results and discussion
The postoperative period was uneventful, the wound healed by primary intention, and the patient was discharged from the hospital on the seventh day after surgery.
At 6 weeks. the appearance of pain sensitivity was noted at the level of the main phalanx along the palmar surface of the 5th finger of the left hand. At the same time, with standard autonervoplasty, the appearance of pain sensitivity is noted for a period of at least 8–10 months. after operation. Motor function remained unchanged, but there was no progression of neurogenic contracture of the 4th and 5th fingers of the left hand.
When the patient was observed for 1 year, dynamic restoration of both sensory and motor functions of the 4th and 5th fingers of the left hand was recorded.
At 1 year after surgery, no pain was noted on palpation in the scar area. The skin had a normal color, the temperature of the fingers corresponded to the temperature on the healthy side; the skin pattern on the pads of the 4th and 5th fingers was clearly contoured. There was no atrophy of the muscles of the hand and forearm compared to the healthy hand, as well as the previously observed neurogenic flexion contracture of the 4th and 5th fingers of the left hand. There was a normalization of secretory function and the appearance of all types of sensitivity in the zone of innervation of the ulnar nerve (5th finger) (Table).
During the assessment of motor function, full extension of the 4th and 5th fingers of the left hand, adduction/abduction of the 5th finger of the left hand with overcoming some resistance were revealed; There was an adduction of the 5th finger to the palm with tension in the hypothenar muscles (Fig. 2).
According to the ENMG examination before surgery, it was not possible to register the motor response of the muscles of the hypothenar group in response to stimulation of the ulnar nerve on the side of the injury. One year after surgery, the amplitude of the motor response was almost completely restored and amounted to 81% relative to the contralateral limb. SRV along motor fibers approached normal (Fig. 3). Based on the results obtained by ENMG, we can conclude that there is reinnervation of the hand muscles, an increase in the number of regenerating motor units and a gradual restoration of the myelin sheath. Observation of the patient over the next 2 years did not reveal any changes in the function of the 4th and 5th fingers of the left hand, which indicates the completion of the recovery process within 1 year. As the results of this clinical case show, the patient experienced accelerated regeneration of the ulnar nerve. According to the classical canons of histology and our own clinical observations, such an injury, as a rule, does not lead to such a significant recovery of the hand muscles in such a short time after surgery. The first signs of reinnervation of the hand muscles and the appearance of sensitivity even with a direct end-to-end suture of the nerve are observed at a period of at least 8–10 months. after operation. We hypothesize that a heterogeneous population of SVF-AT cells plays a key role in triggering post-traumatic peripheral nerve regeneration. SVF-AT cells subjected to enzymatic treatment contain MMSCs, endothelial precursors, M2-polarized macrophages, T-lymphocytes, etc.[11], the use of which can improve the revascularization of inserts and, as a result, provide stimulation of peripheral nerve regeneration[12].
Covering the ends of the nerve and autonervous insertions with fibrin glue allows creating favorable conditions for the survival and differentiation of transplanted cells, and also prevents their uncontrolled migration [13].
It is known that the success of peripheral nerve restoration directly depends on the formation of so-called Bünger bands for the successful growth of axons from the central segment to the peripheral. However, until recently, the mechanism of their directed construction was unclear. As is known, Schwann cells, which participate in the process of myelination and do not proliferate in an inactivated state, are involved in axon regeneration. However, when neurons are damaged, the latter acquire some properties of poorly differentiated cells and form a kind of “bridge” between the damaged parts of the nerve [14]. However, as shown in the study by S. Parrinello et al. (2010), Schwann cells are not sufficient for complete nerve regeneration. The key mechanism for the restoration of peripheral nerves is the initiation of a cascade of processes leading to the expression of various growth factors, such as nerve growth factor (NGF), vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), etc., expressed by the microenvironment and Schwann cells . Fibroblasts send a specialized signal (ephrin-B signal) to Schwann cells, which, in response to it, form Bünger ribbons, which serve as the basis for axon growth in damaged areas of the peripheral nerve from the central end to the peripheral. Without this signal, Schwann cells are not capable of organized migration, as a result of which axon regeneration is incomplete. The response to the signal depends on the activity of the transcription factor Sox2, which is known for its ability to reprogram adult cells back to the stem state[14].
In other words, by introducing into the microenvironment of a damaged nerve a population of cells rich in various cell types, including MMSCs, we may thereby stimulate the process of formation of Bünger bands along which axonal growth occurs.
Interesting results were demonstrated by scientists from China who achieved restoration of a facial nerve defect in a rat using an artery allograft and autogenous SVF-VT. The experimental results confirmed the stimulating effect of SVF-VT on nerve regeneration. Thus, transplantation of autogenous SVF-VTs represents an alternative approach for reconstruction of nerve defects[15].
Cell transplantation to restore peripheral nerves is often combined with so-called tubulation of the nerve defect. This method involves overcoming the defect between the central and peripheral sections of the damaged nerve by implanting biocompatible tubes of organic or inorganic origin and filling their lumen with biodegradable solutions/carriers with cells. It seems to us that it is more logical to use a well-proven method - autonervoplasty - in combination with autotransplantation of SVF-AT cells. As the described clinical case shows, the use of a classical surgical approach in combination with cellular technologies allows one to achieve effective results in restoring lost limb function. We have patented this method of peripheral nerve restoration[16].
Diagnostics
To make a diagnosis, examination using palpation and a series of tests is important.
- Discriminative two-point test - the sensitivity of the branches is checked in turn and the reaction is compared.
- The sensory function of the radial nerve is checked by a discrimination test at two points and pricking the folds of the thumb.
- Motor branches are tested by joint extension.
- The sensitivity of the ulnar nerve is determined on the little finger; to control motor capabilities, the patient spreads his fingers with force.
- Additional tests to analyze ulnar nerve function include ring finger flexion and thumb adduction.
- Motor function of the median nerve is tested by resisting flexion of the wrist and index finger.
- A visual test of the sensitivity of the median nerve is a discrimination test with an attachment in the palm.
Statistics
Neuropathies are most often diagnosed among patients with diabetes mellitus - they develop in 60% of patients in this group.
Up to 15% of adults suffer from various manifestations of neuropathy; in reality, the numbers are supposedly higher, since most patients with initial manifestations do not see a doctor.
Between 20 and 45% of HIV-infected patients suffer from this disorder.
In 30% of patients undergoing chemotherapy for cancer, peripheral nerve damage is observed.
The prevalence of alcoholic neuropathy in different countries ranges from 10-12% to 45-52% among people with various stages of alcohol dependence. It is worth noting that neurophysiological studies reveal initial manifestations of neuropathy in almost 90% of alcoholics.
When is surgery indicated?
- Impaired sensitivity and movement function.
- Tumors.
- Painful neuromas.
- Compression by scars.
- Damage due to trauma.
- Pain syndrome.
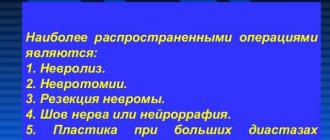
Taking into account the nature of the injury, the method of surgical treatment is selected:
- Excision of scar formations – neurolysis;
- Connecting the nerve sheath and applying a special suture;
- Carrying out plastic surgery of nervous tissue.
During surgical treatment, microsurgical techniques are used to make the comparison as accurate as possible.
On the way to freedom
Active exercises have a greater effect; They are recommended to be performed calmly, without pain, without tension or forceful elements. Then the range of movements is gradually increased. The patient must follow a consistent alternation of load on the affected area and healthy muscle groups, giving rest to the affected muscles. Gradually, free swing exercises are supplemented with exercises with weights, muscle tension, and dosed resistance.
Exercises on a gymnastic wall are useful when stretching exercises are performed for both the upper and lower extremities - mixed hangs. They must be carried out under the supervision of a doctor or rehabilitation instructor to avoid damaging muscles, nerves and tendons with sudden pressure.
In general, a timely, correct diagnosis and competent treatment, as well as the patient’s patience and perseverance in achieving the goal, lead to the restoration of the damaged nerve, a return to complete freedom of movement and an active lifestyle. But this requires a lot of time and effort.
Rehabilitation
The recovery period takes at least six months. First, touch is restored, then sensitivity when touching two points. For recovery, it is important to recognize objects by touch.
Principles of successful rehabilitation:
- Early intervention;
- Reducing the risk of complications;
- Ensuring healing;
- Restoring the functions of the nerve of the hand;
- Using a multi-stakeholder approach.
Restoration of the hand nerve is carried out at the clinic of the Central Clinical Hospital of the Russian Academy of Sciences, in the department of hand microsurgery. Everything is available here for effective treatment of a nerve rupture in the arm - experienced, highly qualified surgeons work, the most modern microsurgical equipment is used, and the staff is caring.
Registration for a consultation is carried out on the website. You can get the information you are interested in and find out the price of treatment by calling the number provided.
Important nuances
At the very beginning of the classes, passive movements are performed, during which, with the help of the patient’s healthy limb or using a gymnastic apparatus (for emphasis), exercises are performed that activate the paralyzed muscles.
Then active movements are gradually introduced. In this case, it is very important to perform the exercises symmetrically, on both sides, since in this case the healthy limb has a beneficial effect on the patient, giving her the correct pattern of movements.
To restore function to an entire arm or leg, it is necessary to train all muscles, focusing specifically on strengthening and developing the affected muscles, but incorporating others as well.
In recovery from injury, a special role is played by giving the affected arm or leg an optimal position, which is carried out by applying orthopedic splints or plaster splints.
They also perform exercises in water, in a specially equipped pool or in baths with the possibility of immersing the forearms and hands, feet and lower legs in them. In the aquatic environment, which softens the pressure of gravity, active movements with increasing amplitude begin, and passive exercises are also carried out with the help of medical personnel.
Article on the topic
Fragile age: causes of fractures in adolescents
The patient will have to overcome atypical movements that sometimes spontaneously occur in the arm or leg when nerves are damaged, as well as the tightness of certain muscles that develops after traumatic nerve damage.
Causes of damage to the central nervous system
Complete loss of movements or their weakening are caused by paralysis and paresis. In such cases, there are several types of dysfunction of the muscles of the limbs:
- tetraplegia (impaired functioning of all limbs);
- monoplegia (impaired functioning of only one limb);
- paraplegia (impaired mobility of the upper or lower extremities);
- hemiplegia (lack of strength in the muscles of the limbs located on the left or right side of the body).
Among the main causes of disruption of the central nervous system, experts indicate:
- brain or spinal cord injuries (bruises, concussions, compression);
- stroke;
- injury or pathology of nerve trunks;
- severe poisoning of the body;
- tumor processes in the brain or its membranes;
- metabolic disorder;
- infections affecting nerve cells;
- severe and frequent stress.
Regardless of whether motor activity has been partially or completely impaired, movements of the upper extremities are much more difficult to fully restore than those of the lower extremities, because fine motor skills are very important for the hands.