To treat nerve sprain or partial damage caused by various injuries, neurolysis is prescribed.
Neurolysis is a surgical operation during which the impaired conduction of nerves is restored, freeing them from compressive adhesions, tissues, and scars.
The procedure is performed under local or general anesthesia using a microscope and special microsurgical instruments.
After removing the structures interfering with the nerve, as well as its release from adhesions and scars, the nerve column is checked for electrical excitability.
If any disturbances occur, the affected areas are resumed, and then the nerve trunk is placed between the muscles in a specially prepared protected place. At the end of the operation, the wound is sutured, the limb is immobilized for 2-3 weeks. Special physiotherapeutic procedures and physical therapy are prescribed.
During the rehabilitation period, the following are prescribed: massage, reflexology, physiotherapeutic procedures, physical therapy. The latter helps in restoring muscle activity.
Recovery stage
Immediately after the operation, pain disappears and sensitivity is restored.
This condition is explained by relief from compression of intact axons. Further restoration of lost functions is slower. This is due to repeated remyelination and axonal growth. For effective and quick treatment, as well as a short recovery period, it is recommended to perform surgery at an early stage, when the compression of the nerve is not very deep and the degeneration process is reversible.
The effectiveness of an operation performed in a timely manner and according to precise indications is manifested in a short time:
- General characteristics of clinical observations
- Treatment
- Neurolysis of peripheral nerves of the extremities
- Neurolysis of the ulnar nerve, what it is, the course of the operation, rehabilitation are described on the website
- 4 Progress of the operation
- Nerve suturing technique
- 3 Preparation for surgery and preliminary diagnosis
- there is an improvement or complete restoration of the functionality of the affected nerve;
- vegetative-trophic pathologies and pain disappear;
- sensitivity returns;
- sweating is normalized.
Types of procedure
The procedure is carried out using the following methods:
- external (external);
- internal (internal).
External neurolysis is usually performed: using a scalpel, the surgeon excises the connecting formations that compress the nerve. It is prescribed in cases where scarring has occurred in the tissues surrounding the nerve.
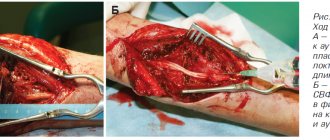
Be careful, photos of the operation! Click to open
External neurolysis of the ulnar nerve
However, in some special cases, internal neurolysis is also prescribed: when the connecting formations are located between the bundles and pass through the nerve trunk.
This procedure is considered a very complex operation that must be carried out in a timely manner, since prolonged infringement of the nerve column can lead to paralysis of the limbs.
General characteristics of clinical observations
In Nervous Diseases and Neurosurgery at the Republican Clinical Hospital, microneurosurgical operations on the trunks of peripheral nerves of the extremities were performed on 181 patients suffering from compression neuropathies, including 96 (53%) males and 85 (47%) females.
The severity of the work performed plays a certain role in the development of compression neuropathies. Most patients defined their work as hard. According to our data, compression neuropathies more often occurred on the dominant limb, i.e., the one more often used in work. In 91 (50.3%) the nerve trunks of this limb were affected, in 73 (40.3%) - in the non-dominant one, and in 17 cases (9.4%) the lesion was localized on both upper limbs.
Compression neuropathies were more often chronic. The duration of the disease was less than 6 months before contacting a neurosurgeon in 90 (49.7%) patients, 6-12 in 19 (10.5%) and more than 12 months in 72 (39.8%) patients. Most patients are diagnosed with compression syndromes in stage III of development, fewer in stage IV, and a small number of cases in stage II.
The peripheral nerve trunks of the upper limb were affected significantly more often than the lower limb. Thus, 156 (86.2%) patients suffered from compressive neuropathy of the nerves of the upper extremity, and 25 (13.8%) of the lower extremity. As can be seen in the diagram (Fig. 56), the nerves at the level of the elbow joint were most often involved in the pathological process.
At the level of the wrist joint, the median nerve in the carpal tunnel was most often affected, the ulnar nerve was affected by the ulnar nerve in the cubital tunnel, and the brachial nerve was affected by the axillary nerve in the deltoid region. At the level of the hip joint, the sciatic nerve was most often affected, and at the level of the knee joint, the common peroneal nerve was most often affected.
Data on the volume of conservative treatment received by patients indicate that the majority received medicinal and physiotherapeutic treatment for radicular syndromes of vertebrogenic etiology. During surgical interventions, we carried out a morphological study of the affected areas of the nerve trunks, as well as the nerve bed, which largely determined the tactics of microneurosurgical manipulations. According to research, paratrunk adhesions, dynamic entrapment, tumors and hematomas of paratrunk tissues (7.2%) were most often identified; sometimes the nerve bed was without pathological changes.
The tactics of microsurgical manipulations depended on the state of the nerve bed and changes in the nerve trunk in the area of compression. Based on this, patients underwent internal neurolysis, epineurotomy, external neurolysis, and a combined operation using microsurgical techniques. In 15 (8.3%) patients with multiple forms of compression neuropathies, 18 additional microneurosurgical interventions were performed.
Thus, compression neuropathies of the peripheral nerves of the extremities occur almost equally often in males and females. In the occurrence of the disease, the leading role belongs to injuries, including professional microtraumatization. Compression syndromes most often develop in people of working age engaged in moderate or heavy physical labor. The vast majority of patients (95%) turned to a neurosurgeon in stages III-IV of the disease. Compression syndromes are much more often localized on the most functionally active upper limb. The ratio of lesions on the upper extremity to lesions on the lower extremity is 6.2:1.
Microneurosurgical tactics were determined by clinical and morphological intraoperative studies, based on which 133 (73.5%) patients underwent internal neurolysis. In 15 (8.3%) cases, additional microneurosurgical operations were performed due to the presence of multiple forms of compression neuropathies.
Price fork
Neurolysis refers to a microsurgical type of surgery in which the nerve is freed from scar tissue.
The cost of the procedure is discussed during the patient’s consultation with the doctor and can vary significantly. This takes into account the severity of the pathological process, the presence of concomitant pathologies and complications, the type of planned operation and the length of stay in a medical institution.
In each city there are a number of clinics offering this procedure at different prices. In Moscow, for example, there are more than 30 medical institutions. The average cost of an operation in the capital is 50,000 rubles, so the cost of neurolysis of the radial nerve at the shoulder level ranges from 20,500 to 135,000 rubles, and intervention at the hand level will cost from 6,500 to 128,000 rubles.
In St. Petersburg, about 10 clinics offer their services, with an average cost of 25,000 rubles. The cost of surgery on the radial nerve ranges from 10,000 to 39,000 rubles, and neurolysis of the sciatic nerve will cost from 10,000 to 66,000 rubles.
In most cases, timely consultation with a doctor allows you to completely restore the conductive capacity of the nerve. Experienced doctors, modern equipment and innovative diagnostic methods will help you quickly and effectively get rid of peripheral nerve diseases.
Treatment
People with median nerve neuropathy rarely see a doctor at the first stage of the disease. Referral occurs when more alarming symptoms of neurological problems appear:
- spasms, convulsions;
- crawling sensation;
- problems with coordination;
- lack of sensitivity to temperatures.
For treatment of the median nerve of the arm to be successful, it is important to find the exact location of the lesion. It is equally important to establish the cause, which is done at the diagnostic stage
It is important to treat stage 2 IVH in newborns
For effective therapy, the doctor also needs:
- determine the degree of nerve damage;
- identify factors leading to this symptom;
- find a specific point of defeat.
Treatment happens:
- operative (using surgery);
- conservative (medicines). Often doctors turn to etiotropic therapy. This is treatment with antibiotics, antiviral agents, and vascular drugs.
- Absorption therapy has a good effect in relieving nerve compression. It involves taking various medications and enzymes, agents that absorb and soften scar tissue. If the compression is not severe, manual therapy and special massage are often sufficient.
- Nerve restoration. Special medications prescribed by a doctor help “revitalize” the nerve.
- Muscle rehabilitation. The goal of therapy is to restore their muscle volume. Treatment procedures are prescribed by a rehabilitation doctor.
- Conservative treatment of the radial and ulnar nerves may include wearing special splints.
What other means are used?
- Demixidol in the carpal tunnel area.
- Acupuncture.
- Interstitial electrical stimulation.
- Therapeutic blockades in the carpal tunnel (diprospan plus lidocaine), intramuscular injections (movalis plus novocaine)
- Non-steroidal anti-inflammatory drugs, in addition to blockades (artrosilene).
During the diagnosis, a disease may also be identified - plexitis of the median nerve. It is caused by injury or infection.
Initially, medicinal, conservative methods of therapy are always used. If physiotherapeutic treatment is ineffective, surgery is performed in the clinic. The decision in favor of surgical intervention is made when the integrity of the nerve trunk is damaged and there is severe weakness in the fingers.
It is not recommended to treat the disease with folk remedies. During therapy, the patient should not overwork or subject himself to heavy physical activity. During the acute period of the disease, you need to lie down and rest more.
Exercise therapy and special exercises are usually prescribed in the postoperative period. Physiotherapy is carried out during conservative treatment or also after surgery.
For patients with the disease, sanatorium-resort treatment may be indicated. A contraindication to it is the acute period of the disease.
Initial examination
If you feel certain ailments, it is recommended to contact the clinic for help. To prescribe treatment, the doctor must find out the root cause of certain problems and collect anamnesis.
To do this, he can prescribe the following types of diagnostics:
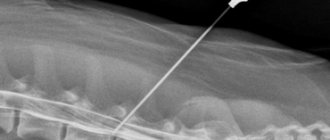
- computed and magnetic resonance imaging;
- X-ray of relevant organs and areas;
- testing for electrical excitability;
- certain tests for sensitivity and the ability of joints to perform certain motor functions.
When choosing a treatment method, the doctor takes into account the following factors:
- statute of limitations for injury;
- nature of damage;
- previous operations;
- degree of tissue scarring;
- level of nerve damage.
The specialist also evaluates the presence of concomitant pathologies.
Neurolysis of peripheral nerves of the extremities
Surgical treatment of nerve damage can be carried out at different times after injury: primary, delayed and late operations.
Neurolysis
is an effective technique for restoring damaged nerves of the limbs, allowing the limbs to return functionality and sensitivity.
In a number of situations, during neurolysis, a nerve is transposed
, that is, it is displaced or a fragment is transferred from other parts of the body for implantation at the site of the rupture.
The essence of neurolysis
– in isolating nerve fiber and eliminating factors that disrupt its conductivity. This is, first of all, compression due to scars or calluses. This kind of disruption of nerve conduction simultaneously causes loss of a number of functions of the limb and increased irritation of the nerve, manifested by pain.
Surgical manipulations for neurolysis require a significant tissue incision so that the surgeon can isolate the nerve from the surrounding tissue. Projection, non-projection, roundabout and angular access on bends is possible
Particular attention is paid to the preservation of the connection between muscle tissue and nerve fiber
During the operation, damaged sections of the nerve can be removed, after which the ends are sutured or the fragments are transposed. The surgical technique here has a number of features; special suture materials and micro-instruments are used.
Neurolysis of the ulnar nerve, what it is, the course of the operation, rehabilitation are described on the website
Nerve neurolysis
Neurolysis is a surgical operation during which excision of growths consisting of connective tissue is performed. They can compress the nerve and cause disruption of the innervation of the limbs.
Most often, the need for neurolysis arises as a result of traumatic injuries, stretching of the nerve, or its compression by scar tissue.
Neurolysis can be external (the pathological process affects the nerve trunk) and internal (the connective tissue has managed to grow inside the nerve).
Nerve neurolysis: what is it?
This operation is performed for injuries, sprains or compression (compression) of nerve nodes. Neurolysis is performed under local anesthesia or pain relief.
During the operation, the necessary conductivity of the damaged nerves is restored. To do this, interfering factors are eliminated: scars, adhesions, tissue structures that could cause compression of the nerve.
The progress of the procedure is controlled through the use of a microscope and other microsurgical instruments. After completing the manipulations, mandatory testing of the nerve for electrical excitability is carried out to check whether it will respond and work normally. If functionality is restored, the wound is sutured.
Then, in the postoperative period, rehabilitation is required, which includes physiotherapeutic techniques and physical therapy.
Indications
This surgical intervention is prescribed for any damage to the peripheral nerves to preserve their anatomical integrity. Indications for such surgical intervention:
- traumatic stretching of nerve trunks;
- deep location of the branches of the ulnar nerve;
- carpal syndrome;
- combined bone and nerve injuries;
- traumatic aneurysms where nerves are involved.
Important Axon: role in the functioning of the nervous system, structure, formation
Today, this operation is used for injuries of the brachial plexus, pseudoneuromas, partial nerve lesions, after unsuccessful nerve suturing, and for various injuries to the nerves of the digital branches.
Neurolysis is used to restore the functions of peripheral nerves in cases of:
- lesions of the median popliteal nerve, which occur with pronounced disturbances of sensory ability;
- damage to the radial nerve, which causes drop hand syndrome;
- injuries to the ulnar nerve that lead to disruptions in motor functionality;
- damage to the peroneal nerve, which is characterized by paralysis of the extensors of the foot, muscles and fingers of the lower extremities, ensuring its rotation outward;
- pinching of the sciatic nerve, which causes pain and inability to fully move.
Neurolysis of the ulnar nerve
Damage to the ulnar nerve most often manifests itself as impaired motor activity of the hand. Bending, bringing together, spreading the little finger, ring finger and half of the middle finger is difficult or impossible. Removing scar tissue allows nerve conduction to be restored. The use of microsurgical techniques helps to avoid damage to nerve bundles.
Neurolysis: progress of the operation
The neurolysis operation includes several stages:
- anesthesia of the nerve below and above the club-shaped thickening;
- opening of the epineurium along the pathological process;
- isolating individual bundles from scars;
- scar excision;
- the integrity of the epineurium is restored;
- a preserved muscle bed is created;
- nerve laying;
- after such manipulations, the constriction disappears and previously lost sensitivity appears.
Rehabilitation after surgery
Recovery from neurolysis begins with sensitivity and pain relief. This occurs by relieving pressure on the nerve. The restoration of other functions is somewhat slower. Rehabilitation will be easier if the surgery is performed sooner. After surgery, gradually:
- The functionality of the nerve improves or is completely restored.
- The pain disappears.
- The ability to feel returns.
Neurolysis of the median nerve
The median nerve innervates the thumb, index, middle and half of the ring finger. Damage to the median nerve causes impairment of their sensitivity and motor activity. This allows us to achieve excellent results without the formation of significant cosmetic defects (scars and scars).
If you contact a specialist in a timely manner, neurolysis allows you to restore the conductive ability of the nerve in most cases.
11-05-2018
Technique
Internal neurolysis takes place under anesthesia. Using a scalpel, the fibrous connective tissue that unites the nerve bundles is longitudinally opened along the entire length of the nerve.
Then individual bundles of fibers are carefully found and the scars between them are excised, thereby providing access to the nerve. The nerve is isolated from tissues slightly below and above the level of damage, palpated to determine the area of scarring, and the scar is removed.
To avoid damage to nearby vessels and branches, the excision is carried out strictly above the nerve, but not on the sides. Afterwards, 2-3 very thin sutures are applied to the fabric. The nerve is immersed in a new muscle bed.
After removing the compression, sensitivity normalizes and pain disappears. Both before and after the operation, mud therapy, electrical stimulation and physiotherapeutic treatment, and the use of neurostimulants are recommended.
The technique of external neurolysis is a bit similar to internal neurolysis. The essence of the operation is as follows: after the nerve column is freed from the surrounding tissue, longitudinal incisions are made in the connective tissue on both sides.
Each bundle of nerves is isolated using a tracheotomy hook and freed from scars either sharply (using instruments) or bluntly (using fingers).
Be careful, photos of the operation! Click to open
Be careful, video of the operation! Click to open
Nerve suturing technique
For more complete surgical treatment and examination of nerve segments, the incision boundaries must be increased to the full depth of the wound. you should not be afraid to do this, you just need to make sure that the cutting lines do not intersect the flexor lines. Skin flaps are pulled to the sides and sections of the nerve above and below the rupture site are isolated
The incision is made along the axis of the nerve carefully so as not to damage small nerve branches and adjacent structures. To excise a scar or neuroma, the incision is made arbitrarily in one direction and parallel to the nerve
The dissection is carried out through the muscle layer along the same axis. Before isolating the damaged area of the nerve, its healthy areas are exposed at a distance of 1 cm above and below the defect. If necessary, the nerve trunks are retracted using gauze loops moistened with saline solution.
After isolating the ends of the nerve using an atraumatic needle, guide sutures are placed on the epineurium of the proximal and distal ends to align the sections of the nerve. Using a small retractor covered with damp gauze, the nerve is supported before the damaged areas are cut off. The ends of the nerve are released and the damaged areas are cut off perpendicular to the axis of the nerve with a sharp scalpel until normal nerve fibers are visible.
The neuroma or combination of proximal neuroma and distal glioma is excised in the same way. It is helpful to make a series of incisions, leaving a small bridge of tissue that will facilitate further manipulation of the nerve trunk.
During this procedure, a nerve fiber of 1 cm or more can be removed. In the postoperative period, it is necessary to achieve sufficient relaxation to prevent tension on the anastomosis. Additional lengthening can be achieved by carefully mobilizing the nerve trunks a few centimeters from the incision site. To achieve greater relaxation, the proximal portion of the nerve is shortened using a graft (example with the ulnar nerve). A nerve graft is used where the ends of the nerve trunk cannot be connected without tension. Then the ends of the nerve are aligned and the nerve fibers are carefully secured to ensure normal function of the pathways. The success of the nerve suturing operation largely depends on this moment.
When the ends of the nerve are sufficiently straightened, a suture is placed across the defect on the epineurium at a distance of 1 mm from each end. The second seam is placed and tied at an angle of 120° to the first on the opposite side. These 2 sutures are now used to rotate (rotate) the nerve trunk until the edges of the epineurium are aligned using interrupted sutures placed around the line of anastomosis. It is more careful to capture only the epineurium. Sutures should be sufficient to immobilize the ends of the nerve trunk.
The tourniquet is removed, the bleeding vessels are ligated. The wound should be completely dry. Then it is irrigated with warm saline. solution to remove blood clots and organic matter. The guide seams are removed.
After suturing the nerve, the wound is sutured in layers with interrupted sutures, covered with gauze, a layer of cotton wool, and an elastic bandage is applied. Immobilization in a state of slight flexion is achieved with a splint.