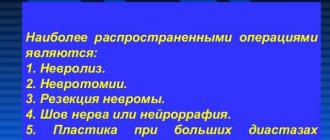
General information
The nervous system is represented by various nerve plexuses, peripheral nerves, spinal cord and brain.
Neuropathy is a non-inflammatory lesion of the nervous system. Peripheral nerves have a very thin structure and are not resistant to damaging factors. According to the level of damage they distinguish:
- Mononeuropathy. Characterized by damage to one single nerve. Mononeuropathy is considered a fairly common option. Most often, mononeuropathy of the upper limb is diagnosed (mononeuritis of the radial or ulnar nerve).
- Multiple neuropathy affecting several nerve endings.
- Polyneuropathy , which is characterized by the involvement of several nerves localized in one area.
Diagnosis by gait: features of manifestations of neuritis of the peroneal and tibial nerves
Neuritis is a pathology that is accompanied by intense pain and deterioration of mobility in the affected area. This is mainly an inflammatory disease. It can affect one, but more often several peripheral nerves.
Neuropathy of the lower extremities is included in a separate group of peripheral mononeuropathies. Since the clinical manifestations of neuritis are similar to the symptoms of injuries to the musculoskeletal system, diagnosis is jointly carried out by specialists not only in the field of neurology, but also in traumatology.
Pathogenesis
Neuropathy is usually determined by the nature of the nerve damage and its location. Most often, the pathology forms after a traumatic injury, after suffering from general diseases and during intoxication.
There are 3 main forms of neuropathy:
- Post-traumatic neuropathy. Violation of the integrity of the nerve myelin sheath occurs as a result of acute injury or severe blow. With tissue swelling, improper scar formation and bone fractures, compression of the nerve fibers occurs. Post-traumatic neuropathy is characteristic of the ulnar, sciatic and radial nerves.
- Diabetic neuropathy. Damage to nerve endings is also recorded with high levels of sugar and blood lipids in the blood.
- Toxic neuropathy. As a result of infectious diseases such as herpes , HIV , diphtheria , etc., toxic damage to the nerve plexus occurs. Poisoning with chemical compounds and overdose of certain medications can lead to disruption of the integrity of the nerve trunk.
Neuropathy can develop against the background of a disease of the hepatic system, kidney pathology, osteochondrosis , arthritis , the presence of neoplasms and insufficient levels of thyroid hormones .
LESIONS OF INDIVIDUAL NERVES, NERVE ROOTS AND PLEXUSES (G50-G59)
Excluded: current traumatic injuries to nerves, nerve roots and plexuses - see nerve injuries by body region
- neuralgia NOS (M79.2)
- neuritis NOS (M79.2)
- peripheral neuritis during pregnancy (O26.8)
- radiculitis NOS (M54.1)
Includes: lesions of the 5th cranial nerve
Includes: lesions of the 7th cranial nerve
Excluded:
- disorders of: auditory (8th) nerve (H93.3)
- optic (2nd) nerve (H46, H47.0)
Excluded:
- ongoing traumatic injuries to nerve roots and plexuses - see nerve injury by body region
- lesions of intervertebral discs (M50-M51)
- neuralgia or neuritis NOS (M79.2)
- neuritis or radiculitis: brachial NOS (M54.1)
- lumbar NOS (M54.1)
- lumbosacral NOS (M54.1)
- thoracic NOS (M54.1)
Excluded: current traumatic nerve injury - see nerve injury by body region
Excluded: current traumatic nerve injury - see nerve injury by body region
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without further clarification.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
Classification
They are classified according to localization:
- Neuropathy of the lower extremities. The most common diabetic neuropathy of the lower extremities is caused by diabetes mellitus . In this form, the peripheral nervous system innervating the lower extremities is affected.
- Peroneal nerve neuropathy. Characteristically, one peroneal nerve is affected, which is manifested by muscle weakness and impaired sensitivity in the innervated area. ICD-10 code: G57 – mononeuropathies of the lower extremities.
- Distal axonal neuropathy after cutting. Post-traumatic or axonal neuropathy develops as a result of damage to nerve endings that arise from certain structures of the spinal cord and are responsible for transmitting nerve impulses to the limbs. If nerve transmission is difficult or completely interrupted, the patient complains of tingling or complete loss of mobility. Distal axonal neuropathy manifests itself differently depending on the nature, type and location of the pathological process.
- Ischemic neuropathy develops when nerve endings are compressed in the area of the musculoskeletal joints and in the spinal column. A violation of not only innervation, but also blood circulation is recorded, which leads to the formation of ischemia. With a chronic course of the process and a long-term disorder, paresthesia and hypotrophic processes develop, which in severe cases can lead to paralysis and necrosis . Ischemic neuropathy has a wide range of symptoms and is not difficult to diagnose.
- The best known form is optic neuropathy. Anterior ischemic optic neuropathy . Characterized by damage to the anterior segment of the optic nerve, which leads to very rapid and persistent impairment of visual function, up to complete or partial atrophy of the optic nerve. Anterior optic neuropathy is also known as vascular pseudopanillia . Posterior ischemic optic neuropathy. It is characterized by damage to the retrobulbar posterior part of the optic nerve due to ischemic effects. The posterior form is also fraught with loss of visual perception.
- Ulnar nerve neuropathy. The peripheral nervous system can be affected by several causes. Damage to the ulnar nerve is most often encountered in traumatology. As a result of compression of the nerve trunk, which is located in the area of the elbow joint, the entire upper limb is affected.
- Radial nerve neuropathy. Clinically, it manifests itself as a characteristic symptom of a “dangling hand,” which is caused by the inability to straighten the hand and fingers. Damage to the radial nerve can be associated with trauma, metabolic processes, ischemia, and compression.
- Median nerve neuropathy. The nervus medianus can be affected in any area, which will inevitably lead to swelling and severe pain in the hand area and impaired sensitivity. The process of flexion of all fingers and opposition of the thumb is disrupted.
- Pudendal nerve neuropathy. It develops as a result of damage to the pudendal nerve, which is located in the pelvic area. Takes an active part in the act of urination and bowel movement, sending nerve impulses along the nerve trunks that pass through the genitals. Pathology is characterized by severe pain.
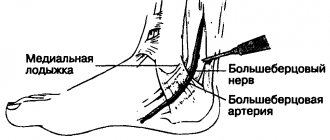
- Neuropathy of the tibial nerve. The clinical picture depends on the level of nerve damage. The tibial nerve is responsible for the innervation of the muscles of the foot and lower leg and the sensitivity of the skin in this area. The most common cause of tibial nerve neuropathy is traumatic injury to the nerve trunk.
- Femoral nerve neuropathy. The clinical picture of damage to the femoral nerve depends on the level of damage to the large nerve trunk.
- Neuropathy of the oculomotor nerve. Diagnosis of pathology requires a thorough examination and is complex. The clinical picture is represented by symptoms that occur in many diseases. When the oculomotor nerve is damaged, ptosis, divergent strabismus, etc. are observed.
What do you need to remember?
- Peroneal nerve neuropathy is a lesion of the nerve tissue in any of its areas.
- Most often, pathology occurs due to injury and compression of the nerve.
- The main manifestations are impaired expansion of the foot and fingers, impaired sensitivity of the anterior surface of the lower leg.
- The diagnosis is established after a thorough examination of the patient and a series of neurological tests.
- Complex treatment with drug therapy, physical therapy, exercise therapy and surgical correction allows you to completely restore the functioning of the affected structure.
- Often, the disease can be completely eliminated.
Literature
- Averochkin A.I., Shtulman D.R. Tunnel neuropathies // Journal. neuropathol. and psychiatrist, named after. S.S. Korsakov. -1991. No. 4. — P.3-6.
- Akimov G.A., Odinak M.M. Differential diagnosis of nervous diseases: A guide for doctors. St. Petersburg: Hippocrates, 2000. - 664 p.
- Voznesenskaya T.G. Pain syndromes in neurological practice //ed. AM V;yn. M.: Medpress, 2001. - 368 p.
- Flores LP, Koerbel A., Tatagiba M. Peroneal nerve compression resulting from fibular head osteophyte-like lesions. Surg Neurol 2005; 64(3):249-52.
- Perkins AT, Morgenlander JC Endocrinologic causes of peripheral neuropathy. Pins and needles in a stocking-and-glove pattern and other symptoms. Postgrad Med 1997;102(3):81-2, 90-2, 102-6.
Causes
It is extremely rare that neuropathy develops as a separate independent disease. Most often, nerve endings are affected against the background of a chronic pathology, which acts as a traumatic factor. The development of neuropathy is preceded by the following diseases and conditions:
- hypovitaminosis;
- metabolic disorder ;
- decreased reactivity;
- intoxication , poisoning;
- nerve fiber injury;
- neoplasms (malignant and benign);
- severe hypothermia;
- hereditary pathology;
- diagnosed endocrine diseases.
G50—G59 Lesions of individual nerves, nerve roots and plexuses
Add a comment Cancel reply
List of classes
- Class I. A00-B99. Some infectious and parasitic diseases
Excluded: autoimmune disease (systemic) NOS (M35.9)
disease caused by the human immunodeficiency virus HIV (B20 - B24) congenital anomalies (malformations), deformations and chromosomal disorders (Q00 - Q99) neoplasms (C00 - D48) complications of pregnancy, childbirth and the postpartum period (O00 - O99) certain conditions arising in the perinatal period (P00 - P96) symptoms, signs and abnormalities identified during clinical and laboratory tests, not classified elsewhere (R00 - R99) trauma, poisoning and some other consequences of external causes (S00 - T98) endocrine diseases, nutritional disorders and metabolic disorders (E00 - E90).
Note. All neoplasms (both functionally active and inactive) are included in class II. The corresponding codes in this class (for example, E05.8, E07.0, E16-E31, E34.-) can, if necessary, be used as additional codes to identify functionally active neoplasms and ectopic endocrine tissue, as well as hyperfunction and hypofunction of the endocrine glands, associated with neoplasms and other disorders classified elsewhere. Excluded: certain conditions arising in the perinatal period (P00 - P96), some infectious and parasitic diseases (A00 - B99), complications of pregnancy, childbirth and the puerperium (O00 - O99), congenital anomalies, deformities and chromosomal disorders (Q00 - Q99 ), diseases of the endocrine system, nutritional disorders and metabolic disorders (E00 - E90), injuries, poisoning and some other consequences of external causes (S00 - T98), neoplasms (C00 - D48), symptoms, signs and deviations from the norm identified in clinical and laboratory studies, not classified elsewhere (R00 - R99).Chapter IX Diseases of the circulatory system (I00-I99)
Excluded
: diseases of the endocrine system, nutritional disorders and metabolic disorders (E00-E90) congenital anomalies, deformations and chromosomal disorders (Q00-Q99) some infectious and parasitic diseases (A00-B99) neoplasms (C00-D48) complications of pregnancy, childbirth and postpartum period (O00-O99) certain conditions arising in the perinatal period (P00-P96) symptoms, signs and abnormalities identified during clinical and laboratory tests, not classified elsewhere (R00-R99) systemic connective tissue disorders (M30- M36) trauma, poisoning and some other consequences of external causes (S00-T98) transient cerebral ischemic attacks and related syndromes (G45.-)
Symptoms of neuropathy
When nerve endings are damaged, muscle fibers become thinner and their reflex function is impaired. In parallel, there is a decrease in contractility and partial loss of sensitivity to stimuli that cause pain.
The clinical picture of neuropathy can be very different, and the pathological process can be localized anywhere, causing neuropathy of the peroneal nerve, trigeminal nerve, facial nerve, ulnar and radial nerve. Damage to sensory, motor or autonomic nerve function negatively affects the patient's quality of life. Several forms of neuropathy occur in patients with diabetes
- Peripheral neuropathy. Characterized by damage to the peripheral nerves that are responsible for the innervation of the upper and lower extremities. Symptoms of neuropathy of the upper extremities manifest themselves in the form of impaired sensitivity in the fingers and toes, a tingling sensation, and a feeling of numbness in the upper extremities. The symptoms of neuropathy of the lower extremities are identical: tingling and sensory disturbances in the lower extremities are noted.
- Proximal form. It is characterized by impaired sensitivity mainly in the lower extremities (buttocks, thigh, lower leg).
- Autonomous form. There is a functional disorder of the genitourinary system and digestive tract organs.
Symptoms of alcoholic neuropathy
Most often, alcoholic neuropathy is accompanied not only by sensory disorders, but also by motor ones. In some cases, patients complain of muscle pain of various locations. The pain syndrome may be accompanied by a sensation of “crawling” in the form of paresthesia, tingling, a feeling of numbness and impaired motor activity.
At the initial stage, patients complain of muscle weakness and paresthesia. In every second patient, the disease first affects the lower extremities, and then the upper ones. There are also simultaneous lesions of the upper and lower belts.
Characteristic symptoms of alcoholic neuropathy:
- a sharp decrease, and in the future a complete absence of tendon reflexes;
- diffuse decrease in muscle tone.
Alcoholic neuropathy is characterized by disruption of the facial muscles, and in more advanced cases, urinary retention is noted. In the advanced stage, alcoholic polyneuropathy is characterized by:
- muscle weakness in the limbs: unilateral or symmetrical;
- paresis and paralysis;
- violation of surface sensitivity;
- sharp inhibition of tendon reflexes followed by their complete extinction.
Clinical manifestations
Symptoms of the disease depend on the cause of the condition. If the process taking place in the iliopsoas region, motor, sensory and vegetative-dystrophic disorders develop throughout the entire innervation zone. Impairments may occur alone or as a combined combination of motor and sensory impairments.
Absolute neuropathy is accompanied by disruptions in the activity of the iliopsoas muscles due to the possibility of alternative innervation. The ability to rotate and flex the hip is maintained. The decrease in the potential of the quadriceps extensor muscle of the knee joint is significantly pronounced. The patient strives to keep his leg straight even while walking.
It is difficult to walk, especially up the stairs, as well as running. There is a change in gait. The lower limb on the corresponding side is stable in the hyperextension position. There is no knee reflex. Tactile and pain sensations are impaired in the anterior inner area of the thigh and lower leg, and the medial area of the foot.
The process is expressed in the form of trophic and vegetative disorders, pain of an irrigation nature. The Wasserman symptom is pronounced - lying on the stomach, the patient experiences pain in the anterior part of the thigh when trying to raise the straightened leg to the maximum height, as well as the Mickiewicz symptom - the inability to bend the leg at the knee joint.
If the process takes place in the inguinal ligament area, the symptoms are similar to those described above. The most common motor disorders are those accompanied by pain when pressing on the inguinal ligament. Compression of the femoral nerve shaft in Gunther's canal is accompanied by pain and numbness of the skin of the central part of the knee joint, the anterior inner surface of the leg and the inner part of the foot.
Spontaneously occurring pain and paresthesia intensify with extension of the leg. The patient keeps his legs bent in a standing position and when walking. The knee reflex is preserved. Tinel's symptom is clearly expressed - when tapped with a hammer, paresthesia passes along the saphenous nerve, significant pain is detected at the site where the nerve exits the conductive canal.
Tests and diagnostics
Neuropathy is considered a rather difficult disease to diagnose, which is why it is so important to correctly and thoroughly collect anamnesis. The difficulty lies in the long-term absence of certain symptoms. The doctor will have to find out: whether medications were taken, whether viral diseases were suffered, or whether there was contact with certain chemicals.
The onset of the disease can occur against the background of alcohol abuse. The diagnosis is pieced together based on many factors. Neuropathy can occur in different ways: progressing over several days or years, and even lightning fast.
Using palpation, the doctor examines the nerve trunks, identifying pain and thickening along their course. A Tinnel test is required . This method is based on tapping the nerve ending and identifying tingling in the zone of sensitive innervation.
A laboratory blood test is performed to determine ESR, and sugar levels are measured. Additionally, an X-ray examination of the chest . Electrophoresis of whey proteins is also performed .
Description
Peroneal nerve neuropathy.
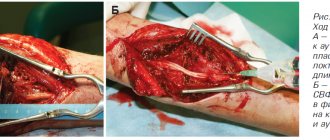
One of the mononeuropathies of the lower extremities, accompanied by foot drop syndrome - the inability to dorsiflex the foot and extend the toes, as well as sensory disorders of the skin of the anterolateral region of the leg and dorsum of the foot. The diagnosis is made on the basis of anamnesis, neurological examination, electromyography or electroneurography. Additionally, an ultrasound scan of the nerve and examination of the osteoarticular apparatus of the lower leg and foot are performed. Conservative treatment is carried out using a combination of medications, physiotherapy and orthopedic methods. If it fails, surgery is indicated (decompression, nerve suture, tendon transposition, etc.).
Treatment
Therapy for non-inflammatory damage to nerve endings is individual in nature and requires not only an integrated approach, but also regular prevention.
Treatment methods are selected depending on the form, degree and causes that contributed to the damage to neuromuscular conduction. All therapy is aimed at fully restoring nerve conduction. In case of toxic damage to the nervous system, detoxification measures are carried out (elimination of influencing factors, administration of an antidote ).
Treatment of diabetic neuropathy
In diabetic cases, measures to maintain normal blood sugar levels are recommended. At the same time, it is recommended to get rid of bad habits. Metabolic disorders in diabetes mellitus contribute to an increase in the level of free radicals circulating in the bloodstream, with impaired antioxidant activity of one’s own organs and systems. All this leads to disruption of the integrity of the inner lining of the vessel and nerve fiber.
For diabetic neuropathy, the use of medications based on alpha-lipoic acid is indicated:
- Thiogamma;
- Berlition;
- Espa-Lipon.
The traditional neurological set involves the introduction vitamins for the complete restoration of neuromuscular conduction. It is not recommended to resort to treatment with folk remedies.
Medicines
Treatment of lower extremity neuropathy includes the following medications:
- Neuroprotectors or metabolic accelerators in nerve cells. Drugs for treatment: Mildronate ; Piracetam .
- Anticholinesterase medications , the action of which is aimed at optimizing the sensory functioning of nerve endings. The drugs improve neuromuscular conduction of the lower extremities. These include: Prozerin ; Ipidacrine .
- Antioxidants. Prevent negative consequences from the influence of free radicals on the functioning of the nervous system. A high concentration of free radicals has a destructive effect on the tissues of the peripheral nervous system. Preparations: Cytoflavin ; Mexidol .
- Alpha lipoic acid. The drugs help restore neurocytes and speed up metabolism. High effectiveness is observed in diabetic neuropathy.
- Other medications. The use of B vitamins has a good effect; in particular, B1 , B6 , B12 . Vitamin complexes help restore neuromuscular conduction. There are tablet and injection forms: Milgamma ; Neuromultivitis ; Combilipen .
Self-treatment at home is not recommended.
Treatment of neuropathic pain in adults
Neuropathic pain - what is it?
Neuropathic pain occurs when the transmission of impulse signals along the nerves is disrupted. In adults, neuropathic pain syndrome is described as stabbing, burning, shooting and is often associated with electric shock.
Therapy begins with the simplest painkillers ( Ibuprofen, Ketonal ). If they are ineffective and the pain syndrome is severe, antidepressants and antiepileptic drugs (for example, Tebantin ) are prescribed.
Tricyclic antidepressants
Drugs in this group are often used to relieve neuropathic pain. It is believed that the mechanism of their action is based on preventing the transmission of nerve impulses. The most commonly prescribed medication is Amitriptyline . The effect may occur within a few days, but in some cases, pain therapy is extended for 2-3 weeks. The maximum effect of therapy is recorded at 4-6 weeks of intensive treatment. A side effect of therapy is drowsiness , which is why treatment begins with the smallest doses, gradually increasing the dosage for better tolerability. Drinking plenty of fluids is recommended.
Anticonvulsants, antiepileptic drugs
If it is impossible to use antidepressants, anti-epileptic drugs ( Pregabalin, Gabapentin ) are prescribed. In addition to the treatment of epilepsy, medications are excellent for relieving neuropathic pain syndrome. Treatment begins with the smallest doses, identical to antidepressant therapy.
Procedures and operations
In addition to drug therapy, neuropathy of the peroneal nerve also includes physiotherapeutic procedures:
- Magnetotherapy. It is based on the effect of a magnetic field on the human body, which helps relieve pain, restore nerve cells, and reduce the severity of the inflammatory reaction.
- Amplipulse. It is based on the effect of modulated current on the affected area, due to which nerve cells are restored and swelling is reduced. Has an anti-inflammatory effect.
- Electrophoresis with drugs . It is based on the influence of an electric field, due to which medications enter the site of inflammation.
- Ultrasound therapy. When exposed to ultrasound, blood circulation is stimulated and the severity of pain is reduced. Has a tonic and anti-inflammatory effect.
- Electrical stimulation. Restoration of neuromuscular conduction occurs under the influence of electric current.
Radial nerve neuropathy is treated in the same way. A course massage is also recommended to restore the radial nerve.
Prevention
Preventive measures include timely treatment of infectious and systemic diseases, normalization of general metabolism. It is important to understand that pathology can become chronic, which is why timely and competent treatment is so important.
In case of a mild course of the disease and a chronic form of neuropathy, sanatorium-resort treatment is indicated, where the following is carried out:
- aromatherapy;
- laser and light treatment;
- magnetic therapy;
- massage, exercise therapy;
- acupuncture;
- psychotherapy.
Consequences and complications
There are many complications from peripheral neuropathy and they depend primarily on the causative factor that led to damage to the nerve trunk. Main complications:
- Diabetic foot. It is considered one of the most terrible complications of diabetes.
- Gangrene . The cause of the putrefactive process is the complete lack of blood flow in the affected area. The pathology requires emergency surgical treatment: excision of necrotic areas, amputation of a limb.
- Autonomic cardiovascular neuropathy. It is characterized by disturbances in various autonomic nervous functions, including sweating, bladder control, heart rate, and blood pressure .
Factors in the formation of the disease
Muscle spasms, injuries and hemorrhages in the psoas muscle lead to compression of the femoral nerve at the iliopsoas border. The cause of compression may be abdominal tumors or hematomas. Hematomas are the result of thrombocytopenia, hemophilia, complications during treatment with anticoagulants in patients with thrombosis, and abdominal aortic aneurysm. Femoral nerve neuropathy can result from damage to the nerve during operations for appendicitis, on the ureters and kidneys, with abscesses of the iliopsoas muscles, and bursitis.
Compression of the femoral nerve in the groin area is caused by femoral hernias, lymphogranulomatosis inguinal, or prolonged forced positioning of the hip. The condition of neuritis occurs as a complication after operations on the hip joint, surgical treatment of inguinal hernias.
In the area of Gunther's canal, femoral neuropathy occurs when the adductor muscles are tense during sports or professional work. Pathologies and instability of the knee joint can also cause muscle tension. The result of knee surgery is iatrogenic femoral neuropathy. Neuropathy of the infrapatellar part of the femoral nerve is associated with the development of thrombophlebitis, varicose veins, and knee injuries.