Polyneuropathy is a disease that affects many peripheral nerves. Neurologists at the Yusupov Hospital determine the cause of the development of the pathological process, the localization and severity of damage to nerve fibers using modern diagnostic methods. Professors and doctors of the highest category take an individual approach to the treatment of each patient. Complex therapy of polyneuropathies is carried out with effective drugs registered in the Russian Federation. They have a minimal range of side effects.
The following types of neuropathies are registered in the International Classification of Diseases (ICD), depending on the cause and course of the disease:
- inflammatory polyneuropathy (ICD code 10 - G61) is an autoimmune process that is associated with a constant inflammatory reaction to various stimuli of a predominantly non-infectious nature (includes serum neuropathy, Guillain-Barré syndrome, a disease of an unspecified nature);
- ischemic polyneuropathy of the lower extremities (ICD code also G61) is diagnosed in patients with impaired blood supply to nerve fibers;
- drug-induced polyneuropathy (ICD code G.62.0) – the disease develops after long-term use of certain drugs or against the background of incorrectly selected doses of drugs;
- alcoholic polyneuropathy (ICD code G.62.1) – the pathological process is provoked by chronic alcohol intoxication;
- toxic polyneuropathy (ICD10 code – G62.2) is formed under the influence of other toxic substances, and is an occupational disease of workers in the chemical industry or those in contact with toxins in the laboratory.
Polyneuropathy, which develops after the spread of infection and parasites, has the code G0. The disease with the growth of benign and malignant neoplasms is encrypted in ICD 10 with code G63.1. Diabetic polyneuropathy of the lower extremities has an ICD 10 code G63.2. Complications of endocrine diseases and metabolic disorders in ICD-10 are assigned code G63.3. Dysmetabolic polyneuropathy (ICD 10 code - G63.3) is classified as polyneuropathies in other endocrine diseases and metabolic disorders.
Treatment
Treatment usually gives positive results with partial atrophy. However, it is impossible to completely restore vision with its help. The main task in this case is to stop the progressive degradation of tissues and fibers, and subsequently the decrease in severity.
By medication
Medicines can play a big role in the treatment of pathology. As a rule, in this case, ophthalmologists prescribe the following categories of medications to their patients:
- Drugs that dilate blood vessels (Dibazol, Papaverine). Necessary to restore normal blood circulation.
- Improves metabolism (Pyrogenal). Promotes resorption and elimination of pathological processes.
- Stimulating the restoration of tissues and fibers (vitamins, Peat, ginseng).
Surgically
In advanced stages of complete or partial nerve degradation, two types of surgical operations are used:
- Tissue transplantation. In this case, healthy human tissue with good capillaries is transplanted to the site of the affected areas. As a result, metabolism and blood circulation improves.
- Reduced blood flow to healthy tissue. The purpose of this operation is to redistribute the blood supply. Some healthy vessels are blocked, resulting in blood flowing to the affected tissue areas.
Hardware treatment methods are also used as additional therapy:
- Magnetic stimulation. With the help of a special device that generates a magnetic field, blood supply, oxygen transfer and tissue nutrition are improved.
- Oxygen therapy. The method is aimed directly at improving metabolic processes and oxygen nutrition.
- Electrophoresis. The method involves dilating blood vessels in order to improve metabolism, using a low current.
- Laser therapy. Uses laser beams to stimulate the affected areas.
- Ultrasound. Used to improve blood flow.
Classification
Depending on the location of inflammation, pathology is divided into:
- Axial, characterized by damage to the axial fascicle with deterioration of central vision and the formation of scotomas. This form of the disease is registered in most patients.
- Peripheral, in which the pathological process occurs in peripheral structures, accompanied by the formation of intrathecal contents, provoking painful sensations. In this case, central vision is preserved, but the visual field is narrowed.
- Transversal, starting in both peripheral and axial structures. In the future, inflammation spreads throughout the nerve trunk, which can result in complete blindness.
Depending on the etiology, neuritis is divided into the following types:
- toxic, caused by toxic substances;
- parainfectious, associated with the penetration of a viral infection or the consequences of vaccination;
- autoimmune, caused by the presence of autoimmune diseases;
- infectious, provoked by cryptococcal meningitis, syphilis, Lyme syndrome.
The disease can occur in:
- An acute form, which is characterized by a rapid onset and rapid loss of vision. Occurs in the primary form of neuritis.
- The chronic form, when the main symptoms increase slowly, with periods of remission and exacerbation. It is possible that neuritis may flow from acute to chronic form.
Forms of neuropathy depending on the prevalence of symptoms
The classification of polyneuropathy according to ICD 10 is officially recognized, but it does not take into account the individual characteristics of the course of the disease and does not determine treatment tactics. Depending on the predominance of clinical manifestations of diseases, the following forms of polyneuropathies are distinguished:
- sensory – signs of involvement of sensory nerves in the process (numbness, burning, pain) predominate;
- motor – signs of damage to motor fibers prevail (muscle weakness, decrease in muscle volume);
- sensorimotor – symptoms of damage to motor and sensory fibers are simultaneously present;
- autonomic – there are signs of involvement of the autonomic nerves in the process: dry skin, rapid heartbeat, tendency to constipation;
- mixed - neurologists determine signs of damage to all types of nerves.
With primary damage to the axon or neuron body, axonal or neuronal polyneuropathy develops. If Schwann cells are affected first, demyelinating polyneuropathy occurs. In the case of damage to the connective tissue sheaths of the nerves, they speak of infiltrative polyneuropathy, and if the blood supply to the nerves is impaired, ischemic polyneuropathy is diagnosed.
Polyneuropathies have various clinical manifestations. The factors that cause polyneuropathy most often first irritate the nerve fibers, causing symptoms of irritation, and then lead to disruption of the function of these nerves, causing “prolapse symptoms.”
Structure of the eye and optic nerve
In order for a person to see something, the light that is reflected from all objects in the surrounding world must reach the receptors of the optic nerve (cones and rods). However, before this, it passes through several structures of the eye. Let's list them, starting with the most superficial:
- The conjunctiva is a thin membrane that covers the eyelids and the outer surface of the eye. It is not of great importance in the transmission of light, however, infectious processes (conjunctivitis) can transfer from it to the nerve;
- The cornea is a slightly convex transparent plate that is located in the front of the eye. Lies most superficially (immediately under the conjunctiva);
- Pupil and iris - under the cornea there is a cavity filled with liquid, and behind it is the iris. This part is shaped like a ring. The hole inside is called the pupil. The iris can narrow or expand, depending on this, the amount of passing light changes;
- The lens is the “lens” of the eye, which can change its shape with the help of the ciliary muscle (body). Thanks to the lens, a healthy person can see distant and nearby objects equally clearly;
- The vitreous body is a jelly-like mass. The last structure that refracts light in the eye;
- The retina is represented by rods (responsible for twilight vision) and cones (perceive color). This is the initial section of the optic nerve. They form an impulse and send it further along the visual path.
All these structures are mainly nourished by the choroid, which is located directly behind the retina. Diseases of the parts of the eye that conduct light develop slowly and lead to vision loss only in the later stages. Neuritis occurs much faster and primarily impairs visual function.
In order to promptly suspect inflammation of the optic nerve, you should know the most common causes that can lead to this condition.
NEUROPATHY OF THE PUDENTAL NERVE (nervus (n) pudendus) - pudendoneuropathy
The nerve provides sensitivity in the anus and perineum, is responsible for the work (innervates) the muscles of the perineum, bladder (located in the bladder) and urethral (in the urethra) sphincters (muscles responsible for holding urine).
Neuropathy is manifested by: unilateral pain in the perineal area, sometimes in its anterior parts: in women - in the vaginal area, in men - in the scrotum; sometimes in the posterior regions - in the area of the anus and rectum (anorectal), in the coccyx and buttocks.
In addition to pain, unpleasant sensations of numbness, tingling, and burning may occur in these same areas. Pain and discomfort increase when sitting and decrease when standing.
There may be short delays in urination.
Upon examination, no changes in the perineal area are detected.
Optic neuritis - description, causes, diagnosis.
Short description
Optic neuritis (ON) is a disease characterized by rapid (within several days), often reversible, loss of vision caused by demyelination of the optic nerve; Predominant age: 18–50 years; The predominant gender is female.
Code according to the international classification of diseases ICD-10:
H46 Optic neuritis
Classification • Intracranial - damage to the intracranial part of the optic nerve • Retrobulbar - the process is localized behind the eyeball • Retrobulbar axial - the process is localized in the maculopapillary bundle of the optic nerve • Retrobulbar interstitial - from the nerve sheaths spreads inward along the glial and connective tissue elements • Retrobulbar orbital - caused by an inflammatory process in orbital cavity; localized in the orbital part of the optic nerve • Retrobulbar transverse - involvement of fibers along the entire diameter of the optic nerve.
Causes
Etiology • Idiopathic NND - etiology unknown • Multiple sclerosis • Viral infections (measles, chickenpox, mumps, mononucleosis, herpes zoster, encephalitis) • Infectious diseases of the central nervous system, paranasal sinuses, orbits • Granulomatous inflammation (syphilis, tuberculosis, cryptococcosis, sarcoidosis) • Uveitis • Fungal infections. Clinical picture • Sharp decrease in visual acuity (over hours or days) of one or both eyes • Pain in the orbital and brow ridge, especially with eye movements • Central, paracentral or arcuate visual field defect • Decreased color vision • Decreased perception of light intensity • Increased symptoms with increased body temperature (Uthoff's sign) • Relative afferent pupillary defect (Marcus Gann pupil: weakening of the direct reaction of the eye to light as a result of a violation of the afferent innervation of the eye: the pupil of the eye being examined, having narrowed significantly when illuminating the other eye, dilates slightly when illuminated).
Diagnostics
Research methods • Ophthalmological examination • MRI or CT scan of the head and orbit is indicated in atypical cases (ineffectiveness of drug therapy) or in the absence of improvement after 10-14 days and negative results of other tests.
Differential diagnosis • Anterior ischemic optic neuropathy • Hypertensive neuroretinopathy • Toxic optic neuropathy • Orbital tumors compressing the optic nerve, intracerebral tumor (development of congestive optic disc) • Leber congenital optic neuropathy. Treatment • Antibacterial therapy - antibiotics, sulfonamides • To improve blood supply - nicotinic acid, pentoxifylline • Dehydration therapy • Desensitizing therapy • GK - local injections, intravenous administration, orally •• Prednisolone 1 mg/kg/day 2 weeks, then reduced for 1 –2 weeks •• Pulse therapy: methylprednisolone 30 mg/kg IV over 30 minutes every 6 hours (total 12 doses), then oral prednisolone 1 mg/kg/day for 11 days, followed by a dose reduction over 1–2 weeks •• Methylprednisolone 20 mg retrobulbar at intervals of 1–5 weeks.
Course and prognosis • Visual activity begins to recover 2-3 weeks after the onset of the disease • Recovery within several months • Vision often returns to normal or almost normal levels • 74% of women and 34% of men with a history of NLD develop absent-mindedness in the long term sclerosis.
Synonyms • Papillitis • Leber's retinitis • Leber's retinopapillitis • Retrobulbar neuritis Abbreviation. NON - optic neuritis
ICD-10 • H46 Optic neuritis
Short description
Optic neuritis (ON) is a disease characterized by rapid (within several days), often reversible, loss of vision caused by demyelination of the optic nerve; Predominant age: 18–50 years; The predominant gender is female.
Code according to the international classification of diseases ICD-10:
- H46 Optic neuritis
Classification • Intracranial - damage to the intracranial part of the optic nerve • Retrobulbar - the process is localized behind the eyeball • Retrobulbar axial - the process is localized in the maculopapillary bundle of the optic nerve • Retrobulbar interstitial - from the nerve sheaths spreads inward along the glial and connective tissue elements • Retrobulbar orbital - caused by an inflammatory process in orbital cavity; localized in the orbital part of the optic nerve • Retrobulbar transverse - involvement of fibers along the entire diameter of the optic nerve.
Prevention
Many preventive measures are carried out at home. Compliance with the recommendations of a neurologist and ophthalmologist is necessary not only to prevent the development of pathology, but also to reduce the risk of relapse after treatment.
Medical recommendations for patients and people at risk:
- Strict control of blood glucose levels in diabetes mellitus.
- Taking general strengthening medications as prescribed by a doctor. These are Semax and various neuroprotectors.
- Control of blood pressure in cerebrovascular diseases.
- Timely treatment of acute and chronic infections.
- Quitting alcohol and smoking.
- Proper nutrition and avoidance of fatty foods.
After drug therapy, ophthalmologists prescribe special methods for accelerated restoration of visual acuity. This can be gymnastics for neuritis of the eye, necessary to improve blood supply to the organ. If you have risk factors for the disease, you should periodically visit a doctor and undergo examinations.
For somatic diseases
Diabetic polyneuropathy (ICD10 code G63.2.) is one of the most common and studied forms of somatic polyneuropathies. One of the manifestations of the disease is autonomic dysfunction, which has the following symptoms:
- orthostatic arterial hypotension (decrease in blood pressure when changing body position from horizontal to vertical);
- physiological fluctuations in heart rate;
- disorders of gastric and intestinal motility;
- bladder dysfunction;
- changes in sodium transport in the kidneys, diabetic edema, arrhythmias;
- erectile disfunction;
- skin changes, impaired sweating.
With alcoholic polyneuropathy, paresthesia in the distal limbs and pain in the calf muscles are noted. One of the early characteristic symptoms of the disease is pain, which intensifies with pressure on the nerve trunks and compression of the muscles. Later, weakness and paralysis of all extremities develop, which are more pronounced in the legs, with predominant damage to the extensors of the foot. Atrophy of paretic muscles develops rapidly, periosteal and tendon reflexes are strengthened.
In the later stages of development of the pathological process, muscle tone and muscle-joint sensation decrease, and the following symptoms develop:
- surface sensitivity disorder of the “gloves and socks” type;
- ataxia (instability) in combination with vasomotor, trophic, secretory disorders;
- hyperhidrosis (increased skin moisture);
- swelling and pallor of the distal extremities, decreased local temperature.
Treatment
Treatment tactics depend on the cause that caused the disease. If it cannot be found out, complex therapy is carried out. The patient is indicated for hospitalization. In the hospital, the doctor will be able to monitor the patient’s condition and adjust the treatment of inflammation of the nerve tissue.
For a viral infection, antiviral agents (Amiksin) are prescribed; a bacterial infection is treated with broad-spectrum antibiotics. In parallel, the use of antihistamines is indicated. The consequences of poisoning are relieved with detoxification drugs. Hemodez is used.
To reduce inflammation and swelling, glucocorticosteroids (Prednisolone, Dexamethasone) are used. In case of significant impairment of visual function, the drugs are administered with a syringe behind the eyeball.
Actovegin and Trental help improve nutrition and normalize the supply of oxygen to the brain and optic nerve tissues. Vitamins PP, B1, B6 normalize metabolism.
To improve the transmission of nerve impulses, cholinesterase inhibitors, for example Neuromidin, are prescribed.
If optic neuritis accompanies multiple sclerosis, interferons (Extavia, Betaferon), Glatiramer acetate, and immunosuppressants are used.
During the recovery period, the use of traditional medicine is recommended. A few aloe leaves are cut and placed in the refrigerator. After three days, peel them and chop them finely. Add 5 g of medicinal eyebright, the color of cornflower, as well as 200 g of honey. Pour the resulting mixture with 700 ml of dry red wine, stir, place in a water bath for 40 minutes, and strain. Drink one tablespoon before meals.
Causes of optic neuritis
Multiple sclerosis is considered the main cause of optic nerve damage. This is an autoimmune disease in which the body's defense systems destroy the myelin sheaths of the nerves in the central nervous system. Destroyed myelin is replaced by connective tissue. A variety of neurological disorders occur. Optic neuritis may be the first manifestation of this serious illness. About 15% of patients suffering from this disease later develop other signs of multiple sclerosis.
Autoimmune diseases of the nervous system have not been studied enough. It is believed that damage to the myelin sheaths of nerves occurs due to the influence of internal and external factors, including hereditary predisposition and chronic diseases. Certain gene mutations that increase the risk of developing multiple sclerosis are passed on to children from their parents. The first neurological disorders appear at the age of 18-35 years. Subsequently, the disease progresses and causes severe complications that negatively affect the quality and length of life.
Other reasons
Doctors often diagnose isolated damage to the optic nerve that is not associated with autoimmune processes. Neuritis can be a complication of existing chronic diseases.
Causes not related to multiple sclerosis:
- inflammation of the bones and soft tissues of the orbit, such as periostitis, phlegmon and other pathologies caused by the proliferation of pathogenic bacteria (infectious agents can enter the eyeball area and cause optic disc neuritis);
- chronic and acute infectious processes in the area of the eyeball, we are talking about inflammation of the iris, retina, cornea and other structures of the eye;
- inflammatory diseases of the brain and its membranes (damage to the optic nerve can be a complication of meningitis or encephalitis);
- bacterial and viral infections of the upper respiratory tract, such as tonsillitis and sinusitis (in the acute course of the disease, the first signs of neuritis appear within 7-14 days after the onset of infection);
- infection of the gums and roots of the teeth, including periodontitis; inflammatory processes in the upper jaw are especially dangerous;
- systemic infectious diseases: borreliosis, syphilis and herpes;
- poisoning with toxic substances, for example, low-quality alcohol containing methanol, quickly destroys the nerve fibers of the eyeball (toxic neuritis requires immediate treatment);
- malignant or benign tumor, compressing different parts of the optic nerve;
- vascular diseases of the brain: hemorrhagic stroke, ischemic stroke, aneurysm and hematoma.
Doctors are not always able to determine the cause of nerve fiber damage. Idiopathic neuritis is diagnosed in 3% of patients.
Risk factors
Ophthalmologists are aware of numerous diseases and lifestyle features that increase the likelihood of damage to the nerve fibers of the eyeball. The presence of certain forms of predisposition to such pathology should be the basis for prevention.
Main risk factors:
- Diabetes. Increasing blood glucose concentrations cause damage to small vessels that carry nutrients and oxygen to the nerves.
- Chronic autoimmune diseases: neurosarcoidosis, neuromyelitis and others.
- Congenital or acquired dysfunction of the immune system. Immunodeficiency contributes to the frequent occurrence of infections.
- Traumatic brain injury with damage to the structures of the eyeball and brain contusion.
- Bad habits. Alcohol and substances contained in tobacco negatively affect the central nervous system.
- Uncontrolled use of medications. Antibiotics can provoke the development of neuritis.
- Age and gender. The disease is more often diagnosed in women aged 20 to 40 years. In children, the disease can occur after chickenpox or other infections.
- Unfavorable family history. If close relatives of the patient suffered from autoimmune pathologies, the individual risk of neuritis increases.
Preventive measures must be carried out as early as possible, since a predisposition to the disease develops at a young age.
Causes
Etiology • Idiopathic NND - etiology unknown • Multiple sclerosis • Viral infections (measles, chickenpox, mumps, mononucleosis, herpes zoster, encephalitis) • Infectious diseases of the central nervous system, paranasal sinuses, orbits • Granulomatous inflammation (syphilis, tuberculosis, cryptococcosis, sarcoidosis) • Uveitis • Fungal infections. Clinical picture • Sharp decrease in visual acuity (over hours or days) of one or both eyes • Pain in the orbital and brow ridge, especially with eye movements • Central, paracentral or arcuate visual field defect • Decreased color vision • Decreased perception of light intensity • Increased symptoms with increased body temperature (Uthoff's sign) • Relative afferent pupillary defect (Marcus Gann pupil: weakening of the direct reaction of the eye to light as a result of a violation of the afferent innervation of the eye: the pupil of the eye being examined, having narrowed significantly when illuminating the other eye, dilates slightly when illuminated).
Optic neuritis - treatment
The presented disease often undergoes independent remission, but therapy is necessary
It is important to establish what triggered the optic neuritis - treatment methods depend on the causative agent of inflammation. The main conservative methods of treatment are the use of antibacterial and hormonal drugs
If these drugs are ineffective, immunoglobulins and plasmapheresis are prescribed.
Antibiotics for optic neuritis
If the inflammatory process begins against the background of a microbial infection, the use of drugs that suppress it is required. Optic neuritis involves taking broad-spectrum antibiotics:
- Ampicillin;
- Ertapenem;
- Ticarcycline;
- Levofloxacin;
- Amoxicillin;
- Ciprofloxacin;
- Meropenem;
- Levomycetin;
- Moxifloxacin and analogs.
It is prohibited to use antimicrobial agents with ototoxic effects:
- Neomycin;
- Kanamycin;
- Streptomycin;
- Gentamicin.
Antibiotics are not prescribed when the virus has provoked inflammation of the optic nerve - treatment in such a situation requires the use of appropriate medications:
- Famciclovir;
- Cycloferon;
- Valacyclovir;
- Panavir;
- Acyclovir;
- Famvir;
- Valvir and others.
Optic neuritis: treatment with Prednisolone - optimal dose
The basic method of suppressing the inflammatory process is the use of corticosteroid hormones. This is the fastest and most effective way to treat optic neuritis of any form. The modern treatment regimen includes simultaneous injections of 1 ml of Dexamethasone (a solution with a concentration of 0.4%) and internal administration of Prednisolone.
The dosage of the last indicated drug is selected individually, starting from 0.005 g 4-6 times a day. The course of treatment with Prednisolone is 5 days, but its amount should be gradually reduced to 0.001 g per 24 hours. The duration of Dexamethasone injections is 10-15 procedures. At the same time, it is necessary to drip-introduce detoxification medications (Reopoliglyukin, Hemodez) and agents that improve microcirculation processes (Nitsergolin, Trental).
Additionally, the ophthalmologist may recommend vitamin injections:
- thiamine;
- nicotinic acid;
- pyridoxine or combined solutions.
Optic neuritis – pulse therapy
The considered method of influence is rarely used, only when basic approaches are ineffective or the pathology is of autoimmune origin. Pulse therapy in the treatment of optic neuritis consists of intravenous administration of high doses of corticosteroid hormones, for example, Methylprednisolone. The patient receives from 0.5 to 1 g of the drug every 6 hours for 3-5 days. After complete suppression of the inflammatory process, therapy is gradually transferred to the standard regimen.
Optic neuritis - treatment with folk remedies
Due to the variety of causes of the described disease, its rapid progression and dangerous consequences, it is strictly prohibited to engage in self-therapy. Any traditional methods are allowed to be used only after the approval of an ophthalmologist and under his regular supervision
It is important not to stop conservative treatment. Alternative methods can only serve as adjuvant therapy
Compresses for eyes
Ingredients:
- freshly squeezed juice from aloe leaves – 1 teaspoon;
- cool boiled water – 5 teaspoons.
Preparation, use
- Mix the ingredients.
- Soak cotton pads with the resulting solution.
- Place them on your eyes for 15 minutes.
- Repeat the manipulation 6-8 times a day.
Shilajit for the treatment of optic neuritis
Ingredients:
- clean water – 90 ml;
- freshly squeezed aloe juice – 10 ml;
- mumiyo – 5 g.
Preparation, use
- Shake water with vegetable juice.
- Dissolve the mummy in this liquid.
- Apply 1 drop of the resulting product to both eyes.
- Keep your eyelids closed for half a minute.
- Repeat 2 times a day.
Medicinal syrup for neuritis
Ingredients:
- green pine cones – 100 g;
- flowers and leaves of fragrant rue – 50-70 g;
- lemon – 1 pc.;
- sugar – 1 glass;
- water – 2 l.
Preparation, use
- Mix pine cones, flowers and leaves.
- Pour boiling water over them.
- Add lemon, washed and cut into 4 parts (along with peel and seeds).
- Add sugar.
- Boil the resulting mixture.
- Reduce heat intensity and simmer syrup for 30 minutes.
- Cover the product with a lid and leave for a third of an hour.
- Strain the medicine.
- Drink 1 tbsp. spoon before meals, 3 times a day.
Diagnostics
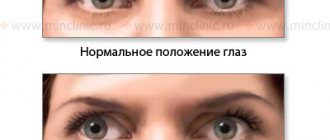
You need to start the examination by visiting an ophthalmologist. During the appointment, the doctor asks the patient about complaints and examines anamnestic data to identify risk factors. Visual acuity is assessed. Additional signs can only be detected with the help of special examinations.
Ophthalmological examinations:
- Assessment of color perception using special tables. A decrease in brightness and intensity of color perception is detected. This is a very important diagnostic criterion in the absence of objective changes in the fundus of the eyeball.
- Assessment of visual fields using a special apparatus. Patients exhibit loss of visual fields.
- Direct ophthalmoscopy is an examination of the fundus structures using a hand-held optical instrument (ophthalmoscope). Exudative edema, hemorrhage and tissue atrophy are detected. In some forms of the disease, no changes are detected.
After ophthalmological examinations, the patient may need to consult doctors of another profile.
Neurological examination
A consultation with a neurologist also begins with questioning. The physician then evaluates the patient's neurological status to look for reflex, cognitive, and mental changes that indicate the presence of serious cerebral pathology. Additional examinations help clarify all the features of the disease.
Ongoing research:
- Assessment of visual evoked potentials is an objective diagnostic method that allows one to determine the localization of the pathological process. Electrodes are attached to the patient's head in the area of the occipital cortex of the cerebral hemispheres to assess electrical activity in all areas of the nerve fibers. While collecting information, the patient looks at the monitor screen to stimulate activity in the studied areas of the central nervous system.
- Ultrasound examination of the eyeball and its nervous structures. This safe and accurate visual diagnostic method allows the doctor to detect swelling and tissue atrophy.
- Magnetic resonance imaging of the brain, which produces three-dimensional images of different parts of the brain. MRI helps to detect even minor changes in the organ, indicating the presence of demyelinating, infectious or vascular pathology.
- Laboratory examination of cerebrospinal fluid. A puncture using a needle is performed in the lumbar region. Using PCR and serological tests, the material is checked for infection that can affect various structures of the nervous system.
An important role in the examination is played by differential diagnosis, which is necessary to exclude diseases with symptoms similar to neuritis. For this purpose, patients are prescribed a study of the retinal vessels.
Hereditary and idiopathic polyneuropathy (code G60)
Hereditary polyneuropathy is an autosomal dominant disease with systemic damage to the nervous system and varied symptoms. At the onset of the disease, patients experience fasciculations (visible contractions of one or more muscles) and spasms in the muscles of the legs. Next, atrophy and weakness develop in the muscles of the feet and legs, a “hollow” foot and peroneal muscular atrophy are formed, the legs resemble the limbs of a stork.”
Later, movement disorders in the upper extremities develop and increase, and difficulties arise in performing small and routine movements. Achilles reflexes are lost. The preservation of other groups of reflexes varies. Vibration, tactile, pain and muscle-joint sensitivity decreases. In some patients, neurologists determine thickening of individual peripheral nerves.
The following types of hereditary neuropathies are distinguished:
- sensory radiculopathy with disorders of the functions of peripheral nerves and spinal ganglia;
- atactic chronic polyneuropathy - Refsum's disease.
- Bassen-Kornzweig disease is a hereditary acanthocytotic polyneuropathy caused by a genetic defect in lipoprotein metabolism;
- Guillain–Barré syndrome – unites a group of acute autoimmune polyradiculoneuropathies;
- Lhermitte syndrome, or serum polyneuropathy, develops as a complication of serum administration.
Neuropathologists also diagnose other inflammatory polyneuropathies that develop from insect bites, after administration of anti-rabies serum, rheumatism, systemic lupus erythematosus, periarteritis nodosa, as well as neuroallergic and collagenoses.