Causes of the disease
Classification of cochlear neuritis
- Because of its occurrence, cochlear neuritis in otolaryngology is classified into congenital and acquired. The latter is also divided into post-traumatic, ischemic, post-infectious, toxic, radiation, allergic, and professional. Based on the time of appearance, cochlear neuritis is divided into prelingual - occurring in children before speech development and postlingual - occurring in patients with developed speech.
- According to the level of damage to the auditory analyzer, cochlear neuritis is classified into peripheral, associated mainly with disturbances in sound perception in the inner ear, and central, caused by pathological processes in the auditory structures of the brain.
- Depending on the duration of the disease, there are 3 forms of acquired cochlear neuritis: acute (no more than 1 month), subacute (from 1 to 3 months) and chronic (more than 3 months). According to the nature of the course, reversible, stable and progressive cochlear neuritis is distinguished.
- According to threshold audiometry, there are 4 degrees of hearing loss in cochlear neuritis: mild (I degree) with a threshold of perceived sounds of 26-40 dB, moderate (II degree) with a threshold of 41-55 dB, moderately severe (III degree) - 56-70 dB and severe (IV degree) - 71-90 dB, as well as complete deafness.
Causes of congenital cochlear neuritis
Congenital cochlear neuritis can be caused by pathology at the genetic level or disorders that occurred during childbirth. Hereditary cochlear neuritis is more often observed in combination with other genetic disorders. Hereditary diseases with an autosomal dominant transmission path, the clinical picture of which includes cochlear neuritis, include: Waardenburg syndrome, Stickler syndrome, branchiootorenal syndrome. Autosomal recessive diseases characterized by cochlear neuritis are: Usher syndrome, Pendred syndrome, Refsum disease, biotinidase deficiency. Cochlear neuritis can also be inherited as an X-linked pathology. For example, with Alport syndrome, manifested by hearing loss, progressive glomerulonephritis and various visual impairments. The occurrence of cochlear neuritis during childbirth is associated with birth trauma or fetal hypoxia, which can develop during discoordinated labor, premature birth, prolonged labor due to weak labor, a narrow pelvis of the woman in labor, or a breech presentation of the fetus.
Causes of acquired cochlear neuritis
Acquired cochlear neuritis in 30% of cases is caused by infectious diseases. First of all, these are rubella, mumps, influenza, measles, ARVI, herpetic infection, then scarlet fever, epidemic meningitis, syphilis, typhus and typhoid fever.
About 10−15% of cochlear neuritis is caused by toxic damage to the auditory nerve.
Ototoxic substances used in medicine include: antibiotics (neomycin, kanamycin, gentamicin, streptomycin, etc.), cytostatics (ciplatin, cyclophosphamide), salicylates, quinine preparations, diuretics, drugs for the treatment of arrhythmia. The cause of cochlear neuritis can be intoxication caused by arsenic, salts of heavy metals, gasoline, phosphorus, etc. Toxic cochlear neuritis can be associated with professional activities. Cochlear neuritis, which develops with chronic exposure to noise and vibration, is also of a professional nature.
The occurrence of cochlear neuritis can be caused by a violation of its blood supply as a result of atherosclerosis, thrombosis, hypertension, vascular disorders in the vertebrobasilar region with chronic cerebral ischemia, the consequences of a hemorrhagic or ischemic stroke.
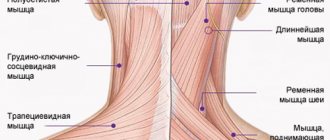
Post-traumatic cochlear neuritis is associated with traumatic brain injury, damage to the auditory nerve during surgical interventions, disruption of the sound-receiving apparatus as a result of barotrauma and aerootitis that developed after it. In some cases, the appearance of cochlear neuritis was observed after acoustic trauma received when exposed to a strong sound (whistle, gunshot, etc.).
Other factors that provoke the occurrence of cochlear neuritis include allergic reactions, acoustic neuroma, hypoparathyroidism, diabetes mellitus, sickle cell anemia, exposure to radiation, Paget's disease, and brain tumors. The development of cochlear neuritis may be a consequence of the aging processes occurring in the auditory nerve in people over 60 years of age.
Symptoms and course of the disease
With neuritis of different origins, the clinical symptoms are the same, the only difference is their intensity.
The main symptom is progressive sensorineural hearing loss (hearing loss), up to complete deafness. In addition, the patient may notice noise and ringing in the ears.
Violation of sound lateralization is also characteristic. With a unilateral lesion, there is a shift in the perceived sound closer to the healthy ear, with a bilateral lesion - to the ear that hears better. Sudden onset cochlear neuritis is characterized by hearing impairment that develops over several hours, usually of a unilateral nature. In most cases, the patient discovers hearing problems after waking up from a night's sleep. In other cases, the acute form of cochlear neuritis can develop within 2-3 days. Acute cochlear neuritis can develop into subacute and chronic forms. During chronic cochlear neuritis, there are 2 stages: stable and progressive. The latter manifests itself as hearing impairment worsens over time and can lead to deafness.
Also, symptoms of auditory neuritis consist of phenomena of irritation and depression of the cochlear and vestibular nerves and sometimes resemble the Meniere symptom complex, while the vestibular apparatus is disrupted. Vestibular symptoms:
- paroxysmal dizziness, which can occur with nausea and vomiting;
- imbalance;
- instability, increasing with a sharp turn of the head;
- uncertainty when walking.
Bilateral cochlear neuritis often leads to a decrease in the emotionality and expressiveness of patients’ speech, causing them to be withdrawn and socially maladjusted.
Classification of cochlear neuritis of the auditory nerve
Cochlear neuritis is the most common reason why a person's ability to perceive sound is reduced. Auditory nerve disease can affect one side, but sometimes hearing loss affects both sides. According to this, they divide:
- unilateral neuritis;
- bilateral neuritis.
Another classification of the disease concerns the degree of clinical development of cochlear neuritis. It shows how long the nerve dysfunction has been occurring and how severely it is affected. Thus, the following three forms of cochlear neuritis are distinguished:
- Acute cochlear neuritis. The period of the disease at this stage is up to four weeks. If you consult a doctor at this stage of the disease, the probability of complete hearing restoration is 70-90%.
- Subacute sensorineural hearing loss. This stage is diagnosed if the nerve damage lasts from one to three months. Treatment is also used here, the probability of recovery is about 30-70%.
- Chronic sensorineural hearing loss, which lasts for 3 months, is difficult to treat.
There are different types of cochlear neuritis according to the nature and level of damage diagnosed by the doctor. Since the disease is neurosensory in nature, nerve dysfunction can have different origins:
- peripheral cochlear neuritis - causes of impaired sound perception in the inner ear;
- central sensorineural hearing loss - the causes of hearing loss are caused by dysfunction of the corresponding structures in the brain.
According to the degree of development of the disease, four stages of cochlear neuritis are distinguished:
- Mild (I) degree, when the threshold for sound perception is 26-40 dB;
- Moderate (II) degree, the auditory limit here reaches 41-55 dB;
- Moderately severe (III) degree, sound perception threshold 56-70 dB;
- Severe (IV) degree, when the auditory limit is 71-90 dB.
If sound perception is almost completely impaired and the patient is unable to hear any sounds, the doctor diagnoses complete deafness.
According to the likely results of treatment, the nature of the course and symptoms, cochlear neuritis is classified into:
- reversible;
- progressive;
- stable.
In addition, cochlear neuritis is distinguished by the cause of the disease.
- Congenital sensorineural hearing loss, which manifests itself in childhood.
- Acquired cochlear neuritis, the cause of which can be many things. According to this, acquired sensorineural hearing loss is also considered as:
- ischemic;
- radial;
- professional;
- post-traumatic;
- allergic.
If cochlear neuritis occurs before a person learns to speak, then this type of disease is called prelingual. If it appears after, then such neuritis is classified as postlingual.
There can be many reasons for the occurrence of cochlear neuritis, and they differ for congenital and acquired hearing loss.
Degrees of hearing loss
Based on the results of audiography and determination of the average hearing threshold (decibels), the doctor can differentiate the stage of the disease, which will determine the further tactics of patient management. Post-traumatic secondary hearing loss (damage to the hearing organ after acoustic, vibration and barotrauma) also requires determining the degree of damage to objectify the diagnosis.
1
At grade 1 (26-40 dB), a person cannot distinguish between quiet sounds and cannot hear speech in a noisy environment. He understands words of standard volume from a distance of less than 6 meters, and whispers from 1-3 m. With mild hearing loss, the patient does not always consult a doctor, so the disease begins to progress. First degree hearing loss in young children is quite difficult to identify.
2
At level 2 (40-55 dB), spoken speech is perceived at a distance of 4 m, whispers are only discernible at the ear itself. Parents may notice that the child does not respond to his name and does not turn his head towards the sound source.
3
With hearing impairment to degree 3 (55-70 dB), spoken speech is perceived only at a distance of less than 1 m from the speaker, and whispers are indistinguishable. Only at this stage do most patients turn to a specialist.
4
Grade 4 (70-90 dB) is the most severe form of hearing loss and borders on complete deafness. The patient hears only loud sounds uttered near the auricle.
Causes of congenital cochlear neuritis
Congenital cochlear neuritis, symptoms of which appear from birth, may occur due to genetic abnormalities, illnesses suffered by the mother during pregnancy, or problems during the birth process.
- Hereditary hearing loss can occur due to Waardenburg syndrome, branchiootorenal syndrome, Refsum disease, Alport syndrome, Stickler syndrome.
- Diseases suffered by the mother during pregnancy that can cause cochlear neuritis. Among them are: rubella, meningitis, syphilis, influenza, otitis media, mumps, herpes, ARVI.
- Problems during childbirth can cause damage to the auditory nerve. For example, such a disease can be caused by fetal hypoxia, premature birth, weakness of labor or its incoordination, birth trauma, or a narrow pelvis of the laboring mother.
Causes of acquired cochlear neuritis
Acquired cochlear neuritis in a third of cases is caused by inflammatory and infectious diseases. In addition, damage to the auditory nerve is caused by drugs, impaired blood supply, injury, and allergies.
- Infections and inflammatory processes that can cause cochlear neuritis include: ARVI, influenza, rubella, scarlet fever, mumps, syphilis, typhus and syphilis.
- Toxic effects of drugs, for example, antibiotics, anti-arrhythmia drugs; medications containing heavy metals or phosphorus.
- Trauma to the skull, tumors that can damage the auditory nerve.
- Arterial thrombosis, atherosclerotic plaques that disrupt cerebral circulation and blood supply to the auditory nerve.
- Long-term professional activity associated with constant exposure to noisy environments, loud sounds or vibrations.
- Age-related cochlear neuritis associated exclusively with gradual changes in the auditory nerve.
Prevention
Audiological screening is used to prevent sensorineural hearing loss in children. In the first years of life, the child is examined at least twice by a pediatrician to assess his reaction to sounds. If parents notice the child’s lack of activity in response to sounds and noises that interest him, this should also be reported to the pediatrician. If hearing loss is suspected, the child is referred for consultation with a specialist - a pediatric otolaryngologist.
For adults, prevention consists of a protective hearing regimen: avoiding loud and prolonged sounds and timely treatment of inflammatory ear diseases. It is necessary to avoid trauma to the hearing organs, sudden changes in high and low atmospheric pressure, and exposure to intense vibration.
Symptoms of cochlear neuritis
Both unilateral and bilateral cochlear neuritis are characterized by two main symptoms that are constantly present:
- hearing loss (decreased);
- feeling of constant noise.
These manifestations of the disease may be complemented by other problems with the perception of sound, for example, a shift in the sense of the sound source. There are disorders of the vestibular apparatus, dizziness, vomiting, nausea. These symptoms are more characteristic of chronic cochlear neuritis.
Due to the fact that the disease affects the auditory nerve and the perception of sounds is difficult, children with cochlear neuritis suffer from psycho-emotional problems, moral disorders, and difficulties with speech. There is a decrease in the emotional background, isolation, and isolation from society.
Diagnosis of cochlear neuritis
In order to begin treatment of the disease, it is necessary to conduct a broad diagnosis of this problem. As already mentioned, cochlear neuritis exists in a wide variety of types and types and can be classified and defined into groups. Therefore, the doctor needs to conduct many tests, analyzes and procedures in order to fully describe the disease, identifying all aspects of cochlear neuritis and determining its genesis, causes, symptoms, period of occurrence, etc. This is a meticulous process, difficult at an early stage both if there is unilateral and bilateral cochlear neuritis.
The degree of damage to the auditory nerve is determined using audiometry or acoustic impedance testing. Additionally, the ability of the vestibular apparatus to respond to stimuli and load is studied. To determine the nature of the disease, various tests and analyzes are carried out; separately, using computed tomography, x-rays or magnetic resonance imaging, the vascular system, cranial bones, and human brain are studied.
To clarify the diagnosis and check its truth, manipulations are carried out aimed at detecting other diseases. Thus, the patient can be checked for otitis media, cerumen impaction, and otosclerosis using endoscopy or otoscopy.
After other possible options have been excluded from the diagnostic field, the doctor narrows the search and not only records the disease, but also characterizes it, describing the type, variety, and possible cause that caused it.
Prices
| Disease | Approximate price, $ |
| Prices for diagnosis and treatment of sinus pathologies | 10 370 — 17 560 |
| Prices for the treatment of thyrotoxic goiter | 22 590 — 22 670 |
| Prices for treatment of laryngeal cancer | 6 170 — 77 000 |
| Disease | Approximate price, $ |
| Prices for diagnosing migraine | 7 060 — 8 260 |
| Prices for diagnosing childhood epilepsy | 3 100 — 4 900 |
| Prices for brain shunting for hydrocephalus | 33 180 |
| Prices for treatment of Parkinson's disease | 58 600 |
| Prices for migraine treatment | 9 680 |
| Prices for the diagnosis of amyotrophic lateral sclerosis | 6 550 |
| Prices for diagnosing epilepsy | 3 520 |
| Prices for rehabilitation after a stroke | 78 300 — 82 170 |
| Prices for treatment of childhood epilepsy | 3 750 — 5 450 |
| Prices for treatment of multiple sclerosis | 4 990 — 17 300 |
Otolaryngology in Israel receives extremely positive reviews, and the reason for this is not only the high effectiveness of the treatment, but also its affordable cost for most medical tourists. Prices for diagnostic and treatment procedures in Israeli hospitals are at least a third lower than in similar medical institutions in Western Europe, the USA, Canada and other countries with developed medicine.
The cost of treatment for an ENT disease in Israel depends on its nature, location, stage of development, medications used, the number and type of diagnostic procedures required, therapeutic methods, as well as the individual characteristics of the patient. You can find out the approximate cost of solving a particular ENT problem from a medical representative of the clinic during a free consultation. The final cost will be clear on the spot, after all examinations have been completed and the treatment plan has been approved by the doctor.
Treatment of cochlear neuritis
The goal of treatment for this disease is complete or partial restoration of hearing. If the patient is sick with a chronic form of cochlear neuritis, treatment is prescribed aimed at stabilizing the existing condition and preventing its deterioration. In other cases, cochlear neuritis may respond to various forms of treatment, both in a hospital and in a regular setting.
Drug treatment is used, usually prescribed intravenously. Vasodilator drugs, venotonics, neuroprotectors and disaggregants are indicated for administration over a period of two weeks. Then they move on to another stage of treatment, when the medicine can be taken orally or administered intramuscularly.
If hearing loss was caused by intoxication, first a course of procedures is carried out to remove harmful substances from the body, such as heavy metals, arsenic, phosphorus. After the toxic element is eliminated, treatment is prescribed.
The symptoms of the disease are also relieved, eliminating pain, dizziness, nausea, and vestibular disorders, if any.
In addition to treatment with medications, manipulations are also prescribed. With the wide possibilities of modern ENT medicine, procedures such as electrical stimulation, oxygen barotherapy, electro-, laser-, acupuncture, as well as phonophoresis are successfully used.
This range of treatment options is indicated for those types of disease where there is a possibility of complete or partial restoration of hearing. If the task is such that it is necessary to maintain the patient’s existing health condition, or as an additional therapy, hearing prosthetics may be prescribed.
Hearing aids are indicated not only to make it easier for patients to perceive sounds, but also to restore speech function. Linear, analog, and digital hearing aids are used. In order for the prescribed prosthesis to function correctly, its adjustment and selection must be carried out by a specialized ENT professional.
Surgical intervention, the possibility of which we mentioned earlier, is indicated if cochlear or brainstem implantation is required, or hearing impairment is caused by injury, tumor or neoplasm, the removal of which is necessary. In addition, the operation will be performed on those patients for whom the symptom of dizziness or noise becomes painful.
If the patient has a severe form of cochlear neuritis, then surgery may be aimed at manipulating the cochlea.
Prognosis for cochlear neuritis
The prognosis for the effectiveness of treatment for cochlear neuritis largely depends on the duration and symptoms of the disease. Modern and proven ENT techniques show themselves very well, having proven to be truly effective and efficient solutions to this problem, however, if cochlear neuritis was diagnosed at a late stage, then no medicine can help here. However, in the case when the patient consults a doctor on time, for example, at the stage of acute cochlear neuritis, the probability of recovery and complete restoration of hearing is 50%. Partial hearing restoration is guaranteed for another third of patients.
Chronic cochlear neuritis is practically untreatable; drug and procedural intervention will help little, but the efforts of doctors will be aimed at stabilizing and maintaining the current state of human health. It is important to prevent regression and further damage to the auditory nerve. This is why such patients are prescribed hearing prosthetics: it minimizes the likelihood of further deterioration of the condition, since it significantly facilitates the functioning of the auditory system, preventing it from overstraining.
Doctors repeatedly emphasize the importance of promptly going to the hospital in case of damage to the auditory nerve. Both if cochlear neuritis occurs suddenly, and if it bothers the patient for a certain period of time, it is necessary to go to a specialist. Early diagnosis can save your hearing or prevent it from deteriorating further. Remember that your health is the most important thing, and hearing problems are far from local in nature: damage to the auditory nerve entails disturbances in speech, and therefore in socialization, behavioral sphere, emotional background, mental and moral state.
Morozova S.V..Department of Ear, Nose and Throat Diseases (Head - Prof. A.S. Lopatin) Moscow Medical Academy named after. I.M.Sechenova Directory of polyclinic doctor / No. 10 / 2008
Peripheral cochleovestibular syndrome
Dizziness is one of the most common patient complaints faced by doctors of various specialties - therapists, otolaryngologists, neurologists, emergency doctors.
Often, acute and severe dizziness is combined with hearing impairment and tinnitus, which is caused by damage to the labyrinth and is classified as peripheral cochleovestibular syndrome (PCVCS).
Symptoms of systemic dizziness
The leading symptoms inherent in peripheral (systemic) dizziness:
- an illusory sensation of rotation of objects surrounding the patient or an apparent vector movement of the patient himself along with the surrounding environment;
- nausea or repeated vomiting that does not bring relief;
- impaired balance and gait;
- hearing loss, most often in one ear;
- noise in the ear;
- autonomic disorders (palpitations, sweating, pallor or redness of the face).
Causes of OPCVS
Currently, there are about one hundred etiological factors of OPCVS, among which the leading position is occupied by:
- cardiovascular diseases: primarily hypertensive crisis, vegetative-vascular dystonia, vertebrobasilar insufficiency caused by atherosclerotic disorders and degenerative processes in the cervical spine;
- acute infectious diseases: influenza, ARVI, mumps, encephalitis;
- acoustic and barotrauma;
- intoxication, including the use of ototoxic drugs (aminoglycosides, loop diuretics, platinum drugs).
Differential diagnosis
Dizziness can be due to various reasons, including:
- diseases of the middle and inner ear (labyrinthitis, benign paroxysmal vertigo);
- neurological and mental diseases (Parkinson's disease, migraine, Alzheimer's disease);
- volumetric intracranial formations (tumor, cerebellar abscess);
- cardiovascular diseases (heart rhythm disturbances, arterial hypo- and hypertension, cerebral atherosclerosis, postural hypotension);
- autonomic disorders during menopause and post-castration syndrome;
- household intoxication (alcoholism, smoking).
Dizziness is quite common in old age: by the age of 65, up to 30% of people, and by the age of 80, up to 75% of women and up to 35% of men experience dizziness. It should be noted that about 500 medications have the unwanted side effect of dizziness. Dizziness can be triggered by staying in a stuffy room, visual stress (including working with a computer), driving a car, following moving objects, drinking alcohol, and emotional stress.
A patient with OCVS is subject to urgent hospitalization in a specialized hospital. The basis of effective treatment is timely correct diagnosis of the disease, an etiopathogenetically based individual approach to the development of therapeutic tactics, and initiation of treatment as early as possible.
Dizziness due to vestibular disorders
Dizziness is a typical symptom of vestibular disorders of various locations. If any part of the vestibular analyzer is damaged, two types of sensations may occur:
- sensation of movement of one’s own body relative to any axis or plane (sensation of internal movement - autokinesia interna);
- sensation of movement of surrounding objects relative to one’s own body (sensation of external movement - autokinesia externa).
Internal movement is also called proprioceptive vertigo and is a major component of systemic vertigo. If the patient has nystagmus, the proprioceptive component is joined by a visual component (the sensation of rotation of surrounding objects) - visual dizziness. When the connections between the vestibular nuclei and the cerebellum are damaged, tactile dizziness occurs - a feeling of instability of support relative to one’s own body. Patients complain that the soil is floating away from under their feet, comparing their sensations to walking on the deck of a ship during a storm.
Peripheral vestibular vertigo (vertigo) occurs when the sensory elements of the ampullary apparatus and vestibule of the labyrinth, vestibular ganglion and nerve conductors of the brain stem are damaged. Central vestibular vertigo occurs when there is damage to the connection with the vestibular nuclei in the brain stem, disruption of connections with the cerebellum, medial longitudinal fasciculus, oculomotor nuclei and their own connections, disruption of the vestibulospinal and vestibuloreticular connections (tract), as well as connections with the cerebral cortex.
At the peripheral (labyrinthine) level of the lesion, the dizziness is systemic (“vector”), paroxysmal, has a sudden onset and lasts up to several days, intense, forcing the patient to take a forced position, aggravated by turning the head, usually accompanied by decreased hearing and tinnitus. Central vertigo is often non-systemic, begins gradually, lasts several weeks, months or years, and is accompanied by moderate imbalance. In this form, the severity of dizziness is practically independent of head rotation; focal neurological symptoms are present (for example, impaired tactile and pain sensitivity, oculomotor disorders).
Central vestibular disorders are characterized by a longer course, often non-systemic dizziness (a feeling of swaying, sinking, blurred vision, flickering of spots before the eyes), are not combined with auditory disorders, and individual components of the vestibular reaction can occur in different ways: in the absence of dizziness, severe nausea, vomiting, increased sweating or pronounced nystagmus in the absence of dizziness and vegetative manifestations. With central vestibular vertigo, a lack of harmony in the components of spontaneous vestibular symptoms is revealed, and dissociations in the results of experimental vestibular tests are possible.
Assessment of auditory function
In the diagnosis of ACVO, timely and competent assessment of auditory function is extremely important (acumetry, tone threshold audiometry in the normal and extended frequency range up to 20 kHz, suprathreshold tests, otoacoustic emissions). In case of unilateral cochleo-vestibular syndrome, to exclude acoustic neuroma, impedance measurements are also performed and CVEP is examined. Electrocochleography is used to establish labyrinthine hydrops.
Otoneurological examination
In case of cochleovestibular disorders, an otoneurological examination should be carried out, which involves the comprehensive use of research methods of the vestibular analyzer and the functional state of the cranial nerves, analysis of audiometric data, radiography and other additional laboratory and instrumental research methods.
Plan for otoneurological examination of the patient:
- Study of the patient's complaints, medical history and general medical history.
- Examination of ENT organs according to generally accepted methods, if necessary, otomicroscopy.
- Hearing examination using speech and tuning forks, familiarization with audiological research data.
- Assessment of nasal breathing, olfactometry.
- Determination of sensitivity in the zone of innervation of the trigeminal, glossopharyngeal and vagus nerves.
- Study of the state of motor cranial nerves: oculomotor, trochlear, abducens, facial, glossopharyngeal.
- Study of taste sensations on the tongue, electrogustometry.
- Registration of spontaneous and positional nystagmus, Dix-Hallpike test, electrooculography (EOG).
- Saccadic test, EOG.
- Visual tracking test, EOG.
- Conducting pointing tests to study the coordination of hand movements.
- Detection of adiadochokinesis.
- Stability test in the Romberg pose.
- Stabilometry (posturography).
- Gait study.
- Carrying out caloric, rotational, otolith tests.
- Carrying out a pneumatic test (pressor or fistula test, Lutse test).
An individual approach to a patient with OCVS requires taking into account the nature of his emotional profile, studying unfavorable professional and everyday factors (noise, vibration, intense visual stress, intoxication), identifying and treating concomitant diseases etiopathogenetically associated with the pathology of the labyrinth (cardiovascular pathology: arterial hyper - and hypotension, anemia, metabolic, allergic and vegetative disorders, diseases of the endocrine and excretory system).
Magnetic resonance imaging (MPT)
The results of using the MRI method of the cervical spine, which makes it possible to identify and specify degenerative-dystrophic changes (hernias, protrusions, uncoverebral arthrosis, spondylosis), are of important diagnostic significance. If an acoustic neuroma is suspected, MRI of the brain with intravenous contrast enhancement makes it possible to diagnose a tumor as small as 2 mm. The study of hemostatic parameters and hemodynamic parameters of the bracheocephalic vessels (duplex, triplex scanning, MR angiography) should be considered mandatory.
Urgent Care
Symptomatic drug therapy for OPCVS:
- drugs that reduce vestibular excitability,
- antiemetics,
- sedatives,
- detoxification,
- dehydration (neototoxic diuretics).
Infusion administration:
- drugs that improve microcirculation and intracellular metabolism, have a positive effect on the blood supply to the labyrinth and cerebral hemodynamics (vinpocetine, pentoxifylline, piracetam, low molecular weight dextran, glucocorticoids).
- antioxidants (mexidol),
- neuropeptides (actovegin),
- antiplatelet agents (acetylsalicylic acid),
- cerebroprotectors (Ginkgo biloba preparations).
The use of vertigolytic drugs, primarily betahistine dihydrochloride 24 mg 2 times a day, should be considered a mandatory stage of emergency treatment for OPCVS.
Treatment of OPCVS
The clinical result of therapy directly depends on how timely it is started: when providing medical care in the first hours, it is possible to achieve positive results in 80-90% of cases; when starting treatment a week after the onset of the disease, the prognosis worsens several times. A patient with OPCVS needs bed rest, rest, a gentle diet and adherence to a fairly strict regime: bright lights, loud sounds are excluded, visual stress, telephone use, and smoking are undesirable. OPCVS has an extremely unpleasant emotional connotation and is characterized by increased anxiety and fear, so an important component of therapy is eliminating emotional stress, normalizing the state of the central nervous system, and ensuring adequate sleep.
When providing urgent care, there is a need for symptomatic drug therapy: prescribing drugs that reduce vestibular excitability, antiemetics, sedatives, providing detoxification, dehydration, normalizing vital signs.
Complex etiopathogenetically based pharmacotherapy involves infusion of drugs that improve microcirculation and intracellular metabolism, positively affecting the blood supply to the labyrinth and cerebral hemodynamics (vinpocetine, pentoxifylline, piracetam, low molecular weight dextran, glucocorticoids). The use of antioxidants (Mexidol), neuropeptides (Actovegin), antiplatelet agents (acetylsalicylic acid), cerebroprotectors (Ginkgo biloba preparations), and neototoxic diuretics is indicated.
The use of vertigolytic drugs, primarily betahistine dihydrochloride, 24 mg 2 times a day for 1-3 months, should be considered an obligatory stage of complex therapy for OPCVS. By order of the Ministry of Health and Social Development of the Russian Federation dated April 24, 2006, betahistine was included in the “Standards of Medical Care” as a treatment for patients with impaired vestibular function and sensorineural hearing loss. Domestic and foreign researchers have reliably proven that betahistine (Betaserc) quickly relieves acute attacks of peripheral dizziness, reduces the intensity and duration of dizziness of various origins, improves coordination of movements and balance, reduces the severity of autonomic disorders, helps reduce tinnitus and improve hearing. An important property of the drug is the absence of sedation and influence on blood pressure. Betahistine, effective when taken orally, due to its active effect on the H1- and H3-receptors of the vessels of the inner ear and vestibular nuclei of the central nervous system, selectively improves microcirculation of the inner ear and capillary permeability, normalizes endolymph pressure in the labyrinth, increases blood flow in the basilar arteries, and has a positive effect on the transmission of nerve impulses in the labyrinth. medial and lateral vestibular nuclei and peripheral vestibular receptor formations.
Other treatments
Considering the close connection between the function of the inner ear and the condition of the auditory tubes, it is necessary, along with treatment of the underlying disease, to conduct research and, if necessary, treatment of diseases of the nose and paranasal sinuses, to ensure the normal function of the auditory tubes.
The effectiveness of drug therapy is increased by the use of reflexology (in the absence of contraindications), as well as a mixed form of vestibular training, including gymnastic exercises and passive techniques to increase nonspecific statokinetic stability and resistance to certain professional conditions.
Modern vestibular rehabilitation involves the use of computer stabilographic (posturographic) complexes. The training cycle includes 4 types of functional exercises with a specified level of difficulty:
- static and dynamic exercises in a sitting position on a stationary and on a moving platform;
- static and dynamic exercises for transferring body weight on a stationary and moving platform;
- exercises for walking in a straight line and on steps, including inclined ones, fast and slow running exercises;
- exercises for rehabilitation of the motor system.
Dosage regimen of the drug
Betaserc ® (betahistine dihydrochloride)
The drug is prescribed orally during meals.
Betaserc 24 mg – 1 tablet 2 times a day
An improvement in the condition is noted already at the beginning of therapy. A stable therapeutic effect is achieved within 2 weeks of taking Betaserc and can increase when taking the drug for several months. The treatment is long-term.
The duration of therapy is determined individually. A summary of the manufacturer's information on drug dosing in adults is provided. Before prescribing the drug, read the instructions carefully.