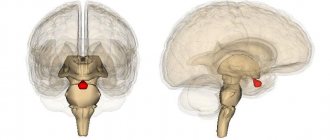
The pituitary gland is an endocrine gland located in the sella turcica (a formation in the human skull). Despite its miniature size, it controls many functions in the body. It is the pituitary gland that produces hormones that are responsible for the functioning of the entire endocrine system. Nature has reliably protected this gland from external influences, but internal factors can still cause pathological changes. One such problem is pituitary adenoma. It can be recognized by hair loss, infertility, changes in appearance, sexual dysfunction and many other signs.
Types of pituitary adenoma
There are various criteria for classifying benign pituitary tumors.
To size:
- microadenoma – tumor size up to 10 mm;
- mesoadenoma - a tumor measuring from 10 mm to 20 mm, located within the sella turcica;
- macroadenoma - a tumor measuring from 10 mm to 30 mm, or extending beyond the boundaries of the sella turcica;
- giant adenoma – a tumor larger than 30 mm.
In a simplified classification, meso- and giant adenomas are classified as medium and giant macroadenomas, respectively.
By nature of distribution:
- endosellar (intrasellar) – the tumor does not extend beyond the boundaries of the sella turcica;
- endosuprasellar - the adenoma grows upward beyond the sella turcica towards the optic chiasm;
- endolaterosellar - spread of the neoplasm into the cavernous sinuses by germination of the lateral wall of the sella turcica;
- endoinfrasellar – pituitary adenoma grows downwards from the sella turcica.
A tumor growing in different directions is called endo-supra-infra-laterosellar.
By origin:
- primary tumors;
- secondary, developed as a result of hypofunction of peripheral endocrine glands;
- adenomas caused by disruption of the hypothalamus, as well as the production of releasing hormones in ectopic formations located in non-endocrine organs.
Based on hormonal activity, pituitary adenomas are divided into active (about 60% of adenomas) and inactive (about 40%). Hormonally active tumors, based on the type of hormones they produce, are divided into:
- somatotropinomas;
- corticotropinomas;
- thyrotropinomas;
- prolactinomas.
Gonadotropinomas are also isolated, which most often do not affect hormonal levels, since they produce biologically inactive hormones. However, sometimes these tumors produce active forms of follicle-stimulating hormone and luteinizing hormone.
There are mixed tumors that produce more than one type of hormones.
Classification of pituitary adenomas of the brain
The pituitary focus is formed in the anterior lobe of the gland (adenohypophysis), which makes up the bulk of the organ (70%). The disease develops when one cell mutates; as a result, it escapes immune surveillance and falls out of the physiological rhythm. Subsequently, through repeated division of the progenitor cell, an abnormal proliferation is formed, consisting of a group of identical (monoclonal) cells. This is an adenoma; this is the most common development mechanism. However, in rare cases, the lesion may initially originate from one cell clone, and after relapse, from another.
Pathological formations are distinguished by activity, size, histology, nature of distribution, type of secreted hormones. We have already found out what type of activity adenomas have - hormonally active and hormonally inactive. The growth of defective tissue is characterized by an aggressiveness parameter: a tumor can be non-aggressive (small and not prone to growth) and aggressive when it reaches large sizes and invades neighboring structures (arteries, veins, nerve branches, etc.).
Large adenoma after removal.
Based on the size of pituitary adenomas, there are the following types:
- microadenomas (less than 1 cm in diameter);
- mesoadenomas (1-3 cm);
- large (3-6 cm);
- giant adenomas (more than 6 cm in size).
According to their distribution, AGGM are divided into:
- endosellar (within the pituitary fossa);
- endoextrasellar (extending beyond the sella landmarks), which extend:
► suprasellar – into the cranial cavity;
► laterosellar – into the cavernous sinus or under the dura mater;
► infrasellar – grow down towards the sphenoid sinus/nasopharynx;
► antesellar – affect the ethmoidal labyrinth and/or orbit;
► retrosellar – into the posterior cranial fossa and/or under Blumenbach’s clivus.
According to histological characteristics, adenomas are given names:
- chromophobe - neoplasia formed by pale, poorly contoured adenohypophyseal chromophobe cells (a common type, represented by NAG);
- acidophilic (eosinophilic) – tumors created by alpha cells with a well-developed synthetic apparatus;
- basophilic (mucoid) – neoplastic formations developing from basophilic (beta cells) adenocytes (the rarest tumor).
Among hormonally active adenomas there are:
- prolactinomas – actively secrete prolactin (the most common type);
- somatotropinomas – produce growth hormone in excess; corticotropinomas – stimulate the production of adrenocorticotropin;
- gonadotropinomas – enhance the synthesis of human chorionic gonadotropin;
- thyrotropinomas – produce a large release of TSH, or thyroid-stimulating hormone;
- combined (polyhormonal) – secrete 2 or more hormones.
Causes of pathology
The reasons for the development of pituitary adenoma are factors that directly affect the brain and the gland itself (trauma, neuroinfections), as well as those that have an indirect effect due to the pathology of other glands and organs. The latter include disorders of the regulatory function of the hypothalamus, thyroid gland, gonads, as well as the appearance in organs that are not endocrine glands of areas that produce hormones (for example, such accumulations of cells are found in small cell lung cancer).
In hereditary forms of the disease, mutations in suppressor genes that suppress the process of tumor cell changes play a role in the occurrence of tumors. The causes of the mutation are unknownSource: Pituitary adenomas within hereditary syndromes. Mamedova E.O., Przhiyalkovskaya E.G., Pigarova E.A., Mokrysheva N.G., Dzeranova L.K., Tyulpakov A.N. Problems of endocrinology, 2014. p. 51-59.
Epidemiology: causes, incidence rates
The factor that stimulates the development of a pituitary tumor has not yet been identified, and therefore remains the main subject of research. Experts only voice versions of the probable causes:
- traumatic brain injuries;
- neuroinfection of the brain;
- bad habits;
- pregnancy 3 or more times;
- heredity;
- taking hormonal medications (for example, contraceptives);
- chronic stress;
- arterial hypertension, etc.
The neoplasm is not so rare; in the general structure of brain tumors it accounts for 12.3%-20% of cases. In terms of frequency of occurrence, it ranks 3rd among neuroectodermal neoplasias, second only to glial tumors and meningiomas. The disease is usually benign in nature. However, medical statistics record data on isolated cases of malignant transformation of adenoma with the formation of secondary foci (metastases) in the brain.
The pathological process is more often diagnosed in women (about 2 times more) than in men. Below we present data on the age distribution based on 100% of patients with a clinically confirmed diagnosis. The epidemiological peak occurs at the age of 35-40 years (up to 40%), at 30-35 years the disease is detected in 25% of patients, at 40-50 years - in 25%, 18-35 and over 50 years - 5% each age category.
According to statistics, about 40% of patients have an inactive tumor, which does not secrete excess hormonal substances and does not affect endocrine balance. In approximately 60% of patients, an active formation is identified, characterized by hypersecretion of hormones. About 30% of people become disabled due to the consequences of an aggressive pituitary adenoma.
Symptoms of pituitary adenoma
Clinical manifestations of the disease can be divided into two groups. With microadenomas or small endosellar tumors, endocrine symptoms come to the fore, varying depending on the hormones secreted.
With large hormonally inactive adenomas spreading beyond the sella turcica, neuro-ophthalmological symptoms prevail, which are different for tumors growing in different directions.
Endocrine symptoms
Somatotropinoma
A tumor that produces somatotropin, or growth hormone. Its manifestations depend on the period of tumor onset. Before the growth of bone tissue is complete (in adolescence and young adulthood), it manifests itself as symptoms of gigantism; in adults, acromegaly.
Gigantism is a proportional increase in bone length and overall height. Women can reach a height of 190 cm, men - over 2 meters.
Acromegaly is characterized by pathological growth of bones, soft tissues, cartilage, and corresponding changes in appearance - the nose, lips, chin, brow ridges, hands, feet increase disproportionately to the rest of the body. Patients experience hyperhidrosis (excessive sweating), hirsutism (excessive hair growth), severe sebum production, and the appearance of papillomas, warts, and nevi on the skin.
In addition, the patient’s internal organs become enlarged, and metabolic and endocrine processes are disrupted. From the cardiovascular system, increased blood pressure, cardiomyopathy, and cerebrovascular accidents are observed. From the nervous system - polyneuropathy, manifested by pain, paresthesia, decreased sensitivity of the peripheral parts of the extremities. The development of obesity, secondary diabetes mellitus, and thyroid pathologies is possible. Source: Main types of complications with pituitary adenomas. K. E. Makhkamov, M. M. Azizov. Bulletin of Emergency Medicine, 2015. p. 90-92.
Corticotropinoma
A pituitary adenoma that produces ACTH is an adenocorticotropic hormone, an excess of which develops Cushing's disease. Its symptoms:
- Cushingoid obesity - an increase in the volume of adipose tissue on the face, back, hips and buttocks, and abdomen;
- swelling and congestion of the face;
- striae - stretch marks of purple-violet color on the skin of the abdomen and thighs;
- skin atrophy, especially on the back of the hands, pustular diseases, fungal infections;
- osteoporosis accompanied by multiple compression fractures;
- arterial hypertension, cardiovascular failure;
- secondary diabetes mellitus.
Thyrotropinoma
A neoplasm that produces thyroid-stimulating hormone. Thyrotropinoma can be primary or secondary.
Primary thyrotropinoma has characteristic signs of thyrotoxicosis (excess thyroid secretion). Its symptoms:
- cardiopalmus;
- tremor - trembling throughout the body, shaking fingers;
- hyperhidrosis;
- nervousness;
- bad dream.
Secondary thyrotropinoma develops as a result of a long course of uncompensated hypothyroidism. It is characterized by:
- weakness, lethargy;
- body swelling and weight gain;
- lethargy, absent-mindedness, memory impairment;
- slow metabolism.
Prolactinoma
One of the most common gland tumors. It arises from cells that synthesize the hormone prolactin. The symptoms of this pituitary adenoma are different in women and men. Source: Aggressive pituitary adenomas (literature review and clinical observation). Kalinin P.L., Trunin Yu.Yu., Fomichev D.V., Chernov I.V., Ryzhova M.V. Tumors of the head and neck, 2021. p. 74-80.
Among women:
- decreased sexual desire up to frigidity;
- menstrual irregularities;
- discharge from the nipples outside the period of breastfeeding;
- infertility.
For men:
- gynecomastia – enlargement of the mammary glands;
- hypoplasia of secondary sexual characteristics;
- decreased libido, erectile dysfunction;
- infertility.
Contrast enhancement
In a native (conventional, without contrast) study, microadenoma is most often isointense in T1 and T2 tissues of unchanged areas of the adenohypophysis. Thus, in the absence of structural signs, the presence of a tumor cannot be excluded. The use of contrast enhancement using the standard method of intravenous administration, with further scanning, in most cases, gives false negative results, i.e. The pituitary gland uniformly accumulates the contrast agent and homogeneously increases the MR signal on T1. Rarely, microadenoma is distinguished by the absence of contrast accumulation with standard administration.
Fig. 1585-1587
Microadenoma in the left half of the pituitary gland (arrowhead in Fig. 1585), having a weak T1 MR signal on a conventional (non-contrast) study. After standard intravenous contrast, a reduced accumulation of the contrast agent in the adenoma is determined (arrowheads in Fig. 1586, 1587), compared to the unchanged pituitary tissue that intensively accumulates contrast.
To verify the presence of a microadenoma, dynamic contrast is used, during which it is possible to evaluate the phase-by-phase accumulation of contrast in the adenohypophysis.
Dynamic sequences demonstrate a rounded area of delayed (or, less commonly, advanced) enhancement at the microadenoma site compared to the rest of the gland [131]. In the late phases of dynamic contrast enhancement, the accumulation of contrast by the adenoma and pituitary gland is aligned with T1. Dynamic contrast-enhanced MRI has a sensitivity of 90% [140].
Fig.1588-1590
On native scans and scans with conventional contrast, there is no convincing evidence for the presence of a microadenoma (Fig. 1588), however, using a bolus injection of a contrast agent, in the first 20 seconds, there is a lack of contrast in the pituitary gland zone (Fig. 1598), where the microadenoma is located, followed by equalization of the intensity of contrast adsorption in the pituitary gland and adenoma (Fig. 1590) and the absence of tumor differentiation.
Macroadenomas always accumulate contrast agent intensely and homogeneously, depending on their structure (ie, with the exception of cysts and areas of hemorrhage).
Fig. 1591-1593
Macroadenomas accumulate the contrast agent intensively and relatively homogeneously (Fig. 1591-1593).
Fig. 1594-1596
Macroadenomas on CT (arrow in Fig. 1594) have a density slightly higher than the density of brain matter (Fig. 1595). After intravenous contrast, an increase in the density of the adenoma is determined (Fig. 1596, 1598), and a clearer differentiation of the tumor (arrow in Fig. 1597) with the ability to visualize it when constructing volumetric reconstructions (Fig. 1599).
Fig. 1597-1599
Gonadotropinomas
Most often hormonally inactive, they can rarely produce active forms of follicle-stimulating or luteinizing hormones, causing ovarian hyperstimulation syndrome in women.
Neuro-ophthalmological signs
With endosuprasellar adenoma, partial loss of visual fields is observed while maintaining visual acuity. An increase in tumor size leads to gradual atrophy of the optic nerves and blindness.
A tumor growing to the sides causes impaired oculomotor function (ophthalmoplegia) and double vision (diplopia), and decreased visual acuity.
When an adenoma grows into the bottom of the sella turcica, patients note nasal congestion, simulating the clinical picture of sinusitis or nasal tumors.
If the tumor grows towards the hypothalamus, patients complain of sleep disturbances, uncontrolled appetite, unstable thermoregulation (fever, chills), emotional disturbances: unstable mood, tearfulness, irritability.
With a large adenoma and its multidirectional growth, the symptoms will overlap each other and be masked. The following neurological manifestations are possible:
- headache, dizziness;
- nausea, vomiting;
- speech and facial expression disorders;
- dysphagia is a swallowing disorder.
Diagnosis of the disease
Patients with suspected pituitary adenoma complain to various doctors: a neurologist, ophthalmologist or endocrinologist.
At the initial appointment, the doctor will conduct a general examination, collect an anamnesis of life and illness, prescribe laboratory and instrumental tests: general blood and urine tests, blood biochemistry, ECG. A doctor of appropriate specialization will conduct an ophthalmoscopy, test visual acuity, neurological examination, and evaluate the existing symptoms.
In addition, the following studies are indicated for patients with pituitary adenoma:
- radiography of the skull;
- CT, MRI of the brain;
- Ultrasound of the thyroid gland, heart, liver, spleen;
- analysis of hormone levels in blood and saliva.
If surgical intervention is indicated, the patient must consult a neurosurgeon.
Treatment of the disease
According to clinical guidelines, there are three main approaches to the treatment of pituitary adenoma:
- conservative (medicines);
- radiation therapy;
- neurosurgical.
The drug method is indicated for small prolactin-producing adenomas. Treatment is carried out with prolactin antagonist drugs.
Radiation therapy is carried out in various ways: gamma, proton, external beam radiation therapy, stereotactic radiosurgery.
For somatotropinomas and corticotropinomas, neurosurgical removal is used. Before surgery, hormonal therapy is often prescribed to reduce the effect of hormone hypersecretion, which sometimes leads to a reduction in the size of the tumor. Drug and radiation therapy are also prescribed after surgery according to indications.
Neurosurgical intervention is recommended for macroadenomas that have severe symptoms and a risk of complications - visual impairment, up to complete blindness, hemorrhage, brain cysts. Source: Pituitary adenomas: history, prevalence, clinical picture, diagnosis, treatment. V. P. Syty, A. A. Gonchar, Yu. V. Syty. Problems of health and ecology, 2010. p. 41-50.
Prognosis and rehabilitation
With timely diagnosis and proper treatment, pituitary adenoma has a generally favorable prognosis without undesirable consequences. Remission after removal of an adenoma occurs in 70-80% of cases, this figure is higher for microcorticotropins and lower for somatotropins and prolactin. The relapse rate is about 12%. Postoperative mortality is low - approximately 4%, decreasing to almost 0 for endosellar and endosuprasellar tumors. The risk of mortality is higher with a large adenoma, its penetration into the ventricular system, or tumor growth of blood vessels.
Rehabilitation, as a rule, does not take much time, since most pituitary adenomas are removed transnasally (through the nose) using endoscopic instruments. In the early postoperative period, the patient is prescribed painkillers, hemostatic agents, and antibiotic therapy. If there are no complications, after a few days the patient is discharged home and is under the supervision of a doctor (ENT, ophthalmologist, endocrinologist) in the clinic. No special rehabilitation measures are required.
Prevention
There is no specific prevention of pituitary adenoma, since the exact causes of tumor development are unknown. If suspicious symptoms appear, you should immediately consult a doctor. Timely diagnosis and treatment will help achieve the most favorable results and maintain the patient’s quality of life.
Sources:
- The main types of complications from pituitary adenomas. K. E. Makhkamov, M. M. Azizov. Bulletin of Emergency Medicine, 2015. p. 90-92
- Pituitary adenomas within hereditary syndromes. Mamedova E.O., Przhiyalkovskaya E.G., Pigarova E.A., Mokrysheva N.G., Dzeranova L.K., Tyulpakov A.N. Problems of endocrinology, 2014. p. 51-59
- Aggressive pituitary adenomas (literature review and clinical observation). Kalinin P.L.,
- Trunin Yu.Yu., Fomichev D.V., Chernov I.V., Ryzhova M.V. Tumors of the head and neck, 2021. p. 74-80
- Pituitary adenomas: history, prevalence, clinical picture, diagnosis, treatment. V. P. Syty, A. A. Gonchar, Yu. V. Syty. Problems of health and ecology, 2010. p. 41-50
Contraindications to surgical treatment
Surgical treatment for pituitary adenoma is in most cases the most effective method. Based on the diagnosis, a tumor removal scheme is developed (open or endoscopic surgery with the choice of optimal access).
Contraindications to radical treatment are:
- advanced age;
- heart and kidney failure in the stage of decompensation;
- diseases of the hematopoietic organs;
- untreated infections of any location;
- post-infarction and post-stroke conditions;
- systemic diseases that occur in severe form.
If surgery is not possible, other methods are prescribed to stop the progression of the pathological process and mitigate the symptoms of the disease.