Blood circulation occurs through elastic vessels, but if the latter become thin, a rupture occurs, leading to hemorrhage. This concept is defined in medicine as hemorrhagic stroke. After hemorrhage, blood enters the nerve tissue, which leads to destructive processes in the tissue. The consequences of this disease are irreversible - disability at best, and death at worst. Therefore, in order to prevent tragedy, it is necessary to have an understanding of why hemorrhage occurs and how to prevent it.
Main reasons
In the first place among the causes is long-term arterial hypertension (almost 50% of all cases). The risk group includes people who ignore the preconditions for the disease and do not take medications to lower blood pressure. Additionally, other root causes are identified:
- Vascular aneurysm. In some areas, the artery widens significantly. The nature of the disease can be either congenital or due to a disease. Unfortunately, it occurs in a latent form, so it cannot be diagnosed in a timely manner.
- Injury to a vessel of a mechanical nature. This is the main reason that leads to stroke before the age of fifty.
- Insufficient blood clotting is also among the causes leading to hemorrhage.
- Consequences of uncontrolled use of antidepressants and anticoagulants.
- Encephalitis, which causes an inflammatory process of an infectious nature.
The inelasticity of the bone structure leads to very high pressure in the nerve centers due to hemorrhage. Therefore, if a large hematoma forms, a person dies within 24 hours.
Among the associated factors are the following:
- Obesity.
- The presence of bad habits over a long period of time.
- Elderly age.
- Heredity factor.
- Some diseases, for example, diabetes.
How does hemorrhage occur?
Arterial hypertension is a devastating disease, which in most cases can lead to hemorrhage. When high blood pressure is diagnosed in a person for a long time, the vessels become thinner accordingly, and necrosis of the vascular walls may occur. Therefore, in the event of a sharp drop in blood pressure, microaneurysms burst. This process occurs very suddenly, therefore, it is completely impossible to predict hemorrhage. Through a burst vessel, blood begins to flow into areas of nerve tissue, causing swelling and hematoma. If a pathological lesion occurs in the stem sections, then the likelihood of respiratory dysfunction increases.
Clinical syndromes of cerebral hemorrhage in hypertension
Hypertensive intracerebral hemorrhages can occur in any patient with hypertension. But more often hemorrhages occur with constant essential arterial hypertension. Hypertensive intracerebral hemorrhages almost always occur while the patient is awake, but are not always necessarily provoked by overexertion. Unlike sudden embolisms of cerebral vessels, hemorrhagic stroke develops within a few minutes, and its symptoms are determined by the location and size of the hemorrhage.
Characteristic symptoms
The manifestation of obvious symptoms will directly depend on the location and extent of the lesion. Clinical signs may appear suddenly and immediately intensify, or appear and disappear. Basically, with hemorrhage, complex symptoms are observed:
- Suddenly a severe headache occurs.
- Attention sharply decreases.
- Nausea appears, which often ends in vomiting.
- Coordination problems begin.
- There are problems with the basic senses of perception - hearing, vision, etc.
- The limbs, both lower and upper, go numb.
- Hyperemia is visible on the face.
- Pronounced wheezing can be heard in breathing.
- Hand tremors.
Subsequent signs include the following:
- The skin of the face takes on a purplish-red hue.
- Trembling of the cheeks is observed on the side of the hemorrhage.
- When examining the tongue, you can see its curvature to the side.
- The patient loses the ability to perceive information and speak.
- Seizures may occur.
- Involuntary urination cannot be ruled out.
Depending on the location of the lesion, distinctive symptoms are distinguished.
| Location of hemorrhage | Main features |
| Distant parts of the brain | 1. Nausea with vomiting. 2. The patient may suddenly lose consciousness. 3. Coma often occurs after hemorrhage. 4. The eyes do not react to light at all. 5. Bradycardia is observed. 6. Dysfunction of the respiratory system. 7. The main reflexes are absent. 8. Hyperthermia |
| Cerebellum | 1. A sharp pain occurs in the back of the head. 2. Deep coma may occur. 3. Dizziness, which causes severe nausea. 4. It is painful for the patient to tilt his head to the sides |
| Gray and white matter | 1. Obvious changes in the psyche. 2. A person becomes uncontrollably overexcited. 3. There are no tactile sensations. 4. Distortion of perception and orientation. 5. Seizures may occur. A complication of this lesion is that the patient denies his mental disorder |
You can learn a few facts about cerebral hemorrhage from the video.
Video - Brain hemorrhage
Symptoms of hemorrhage in children
Oddly enough, hemorrhagic stroke can occur even in a newborn. What is distinctive is that a child can experience damage to several areas of the brain at the same time. The main reason why hemorrhage occurs in a newborn is prematurity. However, in medicine there have been cases where vascular rupture was observed even in full-term babies. This occurs due to late toxicosis or when a mistake was made during childbirth.
In general, the symptoms are practically no different from those that occur in adults. But, there are a number of distinctive signs that warn of rupture of blood vessels. These include:
- The child practically cannot make a sucking movement.
- The sclera of the eyes become red.
- There is a violation of the tendon reflex.
Note! If the baby does not have obvious symptoms of hemorrhage, then the possibility of this pathological process manifesting itself after some time cannot be ruled out. A distinctive feature is the increased growth of the skull. If this phenomenon occurs, it is necessary to urgently seek medical help.
Hemorrhage into the putamen of the brain
Most often, in patients with arterial hypertension (hypertension), one has to observe the clinical picture of hemorrhage in an area of the brain such as the putamen. When hemorrhaging at this location, the hematoma also affects the nearby internal capsule of the brain.
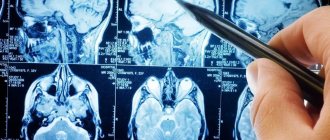
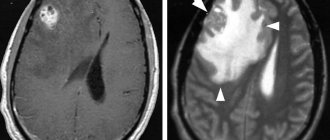
MRI of the brain of a patient with intracerebral hemorrhage due to hypertension. An acute hematoma is visible in the right external capsule and insular cortex (indicated by an arrow).
An axial CT scan of the brain shows a hematoma located in the left external capsule and putamen (indicated by an arrow).
With extensive hemorrhages, the patient immediately loses consciousness, falls into a coma, and develops paralysis of the muscles of half the body (hemiplegia). However, more often he manages to complain about unpleasant sensations in his head. Within a few minutes, a distortion of the face, confusion of speech or its complete absence (aphasia) appear. The patient gradually develops weakness in the limbs, and there is a tendency to turn the eyes in the direction opposite to the side of paralysis. Typically these phenomena develop within 5–30 minutes. Such dynamics of symptoms most likely indicate intracerebral hemorrhage.
Weakness in the limbs increases to complete muscle paralysis (plegia). The patient does not respond to painful stimuli, a pathological Babinski symptom appears, speech disappears (aphasia) when the dominant hemisphere is affected by a hematoma. The patient's consciousness changes from drowsy to stupor. In particularly severe cases, symptoms of compression of the upper part of the brain stem quickly arise. The patient's ensuing coma is accompanied by deep, irregular or intermittent breathing, with dilation of the pupil (on the side of the hemorrhage) and its lack of reaction to light, bilateral Babinski's sign and decerebrate muscle rigidity. The increase in neurological symptoms in the period from 12 to 72 hours after its onset is caused by the development of edema of the brain tissue around the hematoma (perifocal edema), and not by repeated rupture of the vessel.
How is pathology classified?
The classification varies and directly depends on the location and causes of the disease.
Types of hemorrhage by location
| View | a brief description of |
| Intracerebral | When a vessel is damaged, blood fills the brain tissue in the shortest possible time |
| Epidural | Hemorrhage occurs due to head trauma |
| Subarachnoid | The middle and inner membranes are the site of localization of hemorrhage |
| Intraventricular | The name of the type of hemorrhage speaks for itself. That is, blood from the vessel enters the cavity of the ventricle |
| Subdural | Damage occurs between the membranes of the brain |
The above types of hemorrhage can be provoked by the following factors:
- Brain tumor or injury.
- Systematic drug use.
- Thinning of the walls of blood vessels.
- Hypertensive hemorrhage.
Attention! Regardless of the type of hemorrhage, only three hours are left to save a life. Only timely provision of assistance can save the patient’s life and minimize risks.
Hemorrhage into the thalamus of the brain
Thalamic hemorrhage of moderate size also causes the patient to experience paralysis or partial weakness of the muscles of half the body (hemiplegia, hemiparesis) due to compression or stratification by the hematoma of adjacent structures of the internal capsule. The patient will have impaired pain, temperature, proprioceptive and tactile sensitivity of half the body. With lesions of the dominant hemisphere, speech disorder (dysphasia) may occur, often with preserved repetition aloud.
MRI of the brain of a patient with intracerebral hemorrhage in the thalamus (indicated by arrows).
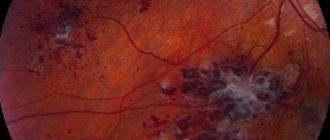
If a hemorrhage occurs in a patient with arterial hypertension in the non-dominant hemisphere of the brain, then there will be a violation of goal-directed actions and recognition (apractoagnosia). Developing homonymous visual field defects in the patient usually then disappear within a few days. Thalamic hemorrhage, spreading inward and downward into the subthalamus, causes oculomotor disorders. They appear including:
- in the form of vertical gaze paralysis
- forced downward rotation of the eyeballs
- different pupil diameters (anisocoria) with the absence of their reaction to light
- strabismus with deviation of the eyeball opposite to the side of the hemorrhage, downward and inward
- on the side of the hemorrhage there is a drooping of the upper eyelid (ptosis) and constriction of the pupil (miosis)
- lack of convergence
- disturbances in horizontal gaze movements (paresis or pseudoparesis of the VI nerve)
- retraction nystagmus
- swelling of the eyelids
Shortening of the neck may be noted. Thalamic hemorrhage in the non-dominant hemisphere of the brain sometimes causes the patient to be unable to speak (mutism).
What diagnostic techniques?
To determine hemorrhage and its type, you should interview the patient about his alarming complaints. If you are unable to speak, it is necessary to talk with loved ones about whether the patient has had frequent increases in blood pressure. It was this factor that could precede the hemorrhage.
Damage to brain tissue can be diagnosed even by visual signs. To do this, you need to ask the patient to move, raise his arms, and talk to him. If these functions are impaired, we can assume a possible hemorrhage.
After a neurological examination, you can begin hardware diagnostics. First of all, a computed tomograph is used to exclude hemorrhage. Thanks to this method, an accurate diagnosis is determined, the location of the lesion and its size. The second effective device for diagnosing pathology is MRI, but, unfortunately, this is a very expensive way to determine hemorrhage. However, MRI can detect even minor damage to brain tissue.
Before the arrival of specialists, it is recommended to provide the following assistance:
- The person should be in such a position that he has free access of air and blood flow.
- In case of vomiting, turn the patient on his side so that the person does not choke on the vomit.
- Apply a cold compress to your head.
- Measure blood pressure.
- Do not disturb the patient and wait for the ambulance to arrive.
First aid nuances
It is worth paying attention that it is strictly forbidden to try to bring the patient to his senses, to move or disturb him. Special treatment for hemorrhage can only be provided by medical professionals.
Reference! The emergency doctor is obliged to carry out the following life-saving measures:
- Introduce a special drug that quickly eliminates cerebral edema.
- Stop bleeding.
- Bring blood pressure back to normal.
- Deliver to intensive care promptly.
Depending on the lesion, the patient may even be prescribed surgical treatment. In this case, the operation must be performed in the first three days after the hemorrhage. These surgical measures consist of several procedures that help get rid of accumulated blood in the aneurysm. Thus, intracranial pressure quickly decreases and the patient’s chance of recovery increases.
The subsequent stage of treatment involves the use of medications that are aimed at normalizing blood pressure and maintaining the patient’s condition in the postoperative period.
Hemorrhage into the pons (brain stem)
After hemorrhage into the pons, the patient usually falls into a deep coma within a few minutes. The clinical picture includes paralysis of the muscles of all extremities (tetraplegia), severe decerebrate rigidity, pupillary constriction (miosis) with up to 1 mm and lack of response to light. In a patient with hemorrhage into the pons, reflex horizontal eye movements caused by turning the head (doll's eye symptom) and irritation of the ears with cold water (caloric test) will be impaired. These patients often experience hyperventilation, high blood pressure, and excessive sweating (hyperhidrosis). As a rule, the death of a patient with hemorrhage into the bridge occurs within a few hours. In rare cases, consciousness remains intact and clinical manifestations indicate a small lesion in the pons. These are symptoms such as disorders of the movements of the eyeballs in the horizontal plane, gross speech disorder (dysarthria), cross motor and sensory disorders, constriction of the pupils (miosis), cranial nerve palsies, bilateral symptoms of involvement of the pyramidal tracts.
Conservative treatment
Therapy is based on specific and basic neuroprotective, as well as surgical treatment, which includes drugs from several pharmacological groups:
- Stimulation of the respiratory system using artificial ventilation.
- Stabilization of blood pressure with the help of special medications ( Enalapril, Labetalol
, if hypertension;
Dopamine
, if hypotension). - Taking antipyretic medications ( Magnesium sulfate
or
Paracetamol
). - Stabilization of water-salt balance ( Lasix
). - Prophylactic medications that prevent infectious inflammation (uroseptics and antibiotics - prescribed individually by a doctor).
- Symptomatic therapy (for convulsions - Thiopental
,
Diazepam
; in case of vomiting -
Cerucal
; if psychomotor overexcitation is observed -
Fentanyl
). - To prevent cerebral edema ( Albumin
solution,
Mannitol
, as well as sedative drugs).
For specific therapy, drugs with neuroprotective effects are used:
- To improve the trophism of nerve tissue, use Actovegin
or
Piracetam
. - It is also recommended to take drugs with antioxidant properties - Emoxipine
and
Mildronate
.
Attention! The above therapy for hemorrhage is approximate, since depending on the type of illness and consequences, the leading doctor determines an individual course of treatment.
Neurosurgical intervention
After the patient is hospitalized in the neurosurgery department, he undergoes an operation within three days, the indications for which are the following:
- large hematomas;
- flooding of the cerebral ventricles with blood;
- aneurysm damage.
Thus, removing blood helps reduce pressure in the skull, which significantly improves prognosis and saves the patient’s life.
Rehabilitation period
About 60% of patients die after suffering a hemorrhage due to untimely neurosurgery. In other cases, with adequate treatment, the patient remains alive, but loses his ability to work. Therefore, rehabilitation therapy is required, which is aimed at restoring functionality. If the patient suffered damage to the brain stem or was in a coma, then rehabilitation will take a long time.
The rehabilitation course includes the following procedures:
- Exercise therapy.
- Application of therapeutic massage techniques.
- Treatment of the patient using electrocoagulation and other physiotherapeutic manipulations.
- If there is a speech disorder, a visit to a speech therapist may be indicated.
The rehabilitation process must take place under the vigilant supervision of a specialist, since self-medication after a stroke is contraindicated.