By etiology:
- Infectious;
- Infectious-allergic (for childhood exanthema infections: measles, rubella, etc.);
- Toxic;
- Allergic (vaccinal, serum, etc.);
- Dysmetabolic: with vitamin deficiency, with endocrine diseases (diabetes mellitus), etc.;
- Discirculatory: for rheumatic and other vasculitis;
- Idiopathic and hereditary (neural amyotrophy of Charcot-Marie, etc.);
- Compression-ischemic lesions of individual peripheral nerves;
- Vertebrogenic lesions (bone, disc, joint, muscle and tendon-ligament formations).
Diseases of the peripheral nervous system of various etiologies can be primary (Guillain-Barré polyneuritis, leprosy, syphilis, leptospirosis, etc.) and secondary (vertebrogenic, after childhood exanthemal infections, infectious mononucleosis, periarteritis nodosa, rheumatism, etc.).
Neuralgia is painful sensations in the area of innervation of certain nerves and the formation of trigger zones of the skin and mucous membranes, irritation of which, for example, touch causes another attack of pain. In the intervals between attacks, neither subjective nor objective symptoms of irritation or loss of function of the affected nerve are observed.
The most common symptoms of damage to the peripheral nervous system:
- viral (Guillain-Barré polyneuritis, viral diseases, influenza, sore throat, infectious mononucleosis, etc.);
- microbial (for scarlet fever, brucellosis, syphilis, leptospirosis, etc.);
- for chronic intoxication (alcoholism, manganese, lead, etc.);
- for toxic infections (botulism, diphtheria);
- blastomatous (for lung cancer, stomach cancer, etc.);
- sensory disturbances (pain, numbness, feeling of fullness, “crawling”, increased or decreased sensitivity of certain areas);
- movement disorders (weakness, impaired motor function of the limbs, facial muscles and eyes);
- vegetative disorders (dry or wet hands and soles, cold extremities).
Symptoms
With neuropathies, symptoms can be different and depend on the affected areas. They cause a lot of discomfort to the patient:
- flaccid muscle paralysis
- pain in limbs
- change in skin sensitivity (there may be a contrast in sensations in one area of the skin compared to another)
- no sensation of pain and more
- amyotrophy
- speech disorder
- feeling of numbness in the face and limbs
- muscle weakness of the limbs
- impaired motor coordination
- dry skin
- focal blanching
- redness and bluish discoloration of the injured area
- Facial asymmetry may occur (if the facial nerves are damaged)
If you find yourself with at least one of the described symptoms, you should immediately seek help from a qualified neurologist.
Diagnosis of diseases of the peripheral nervous system:
Methods for diagnosing diseases of the peripheral nervous system are aimed at identifying and correcting the underlying disease (for example, damage to peripheral nerves in diabetes mellitus requires correction of the underlying disease). An X-ray examination is carried out to identify the severity of degenerative-dystrophic changes in the spine, which are most often the causes of pain and discomfort in the back and limbs, to exclude pathological changes in bone tissue (including fractures).
For some pathologies, an MRI study may be indicated, which is aimed at identifying a pathological process that interferes with the normal functioning of the nerve fiber: for example, radiculopathy due to compression of the nerve root by an intervertebral hernia, neuromas, identifying congenital anomalies, etc.).
Recommendations and prevention
The main prevention of most diseases of the nervous system is maintaining a healthy and active lifestyle, giving up bad habits, timely and adequate treatment of infectious and non-infectious diseases.
If any neurological symptoms occur, do not delay contacting a doctor. Early diagnosis and timely treatment will help prevent the development of complications, prolongation of treatment and the consequences of uncontrolled use of medications. The most complete program of preventive measures is drawn up by a neurologist for each individual patient.
Treatment of diseases of the peripheral nervous system:
Treatment of these diseases includes medication, non-drug and surgical treatment. Drug therapy is aimed at correcting the underlying disease:
- Non-steroidal anti-inflammatory drugs (NSAIDs) are used to relieve pain.
- To normalize vascular tone and improve blood circulation, suitable vascular therapy is selected
- A course of vitamin therapy is prescribed to improve nerve conduction
- Recommended medications to normalize muscle tone
- and other medications, the selection of which is based on a specific pathology
Non-drug therapy includes the use of physiotherapeutic treatment methods, the selection of which depends on the specific pathology, the severity of the process and concomitant pathology:
- reflexology
- massage
- hirudotherapy
- ozone therapy
- osteopathy and manual therapy
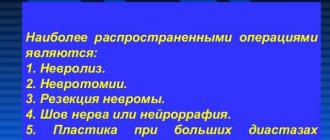
As for surgical treatment methods, they are used in case of long-term persistent neurological defect and ineffectiveness of conservative therapy, or in acute conditions and there are absolute indications for surgical treatment.
For the best result from treatment, it is necessary to contact a neurologist for a face-to-face consultation as early as possible from the onset of the disease; the doctor will develop an individual treatment and examination regimen.
Treatment of neuralgia
Treatment options for neuralgia vary depending on the type and severity of the condition.
Ointments, local nerve blocks, and steroid injections may provide temporary pain relief for mild neuralgia.
Treatment for severe neuralgia pain may require prescription drugs, surgical procedures, or both.
Medications
Painkillers are generally not very effective in controlling neuralgia pain. Medications that can treat the underlying causes of neuralgia include :
- anticonvulsants such as carbamazepine, topiramate, and lamotrigine
- antidepressants such as amitriptyline
- muscle relaxants such as baclofen
- membrane stabilizing drugs such as gabapentin
Diagnostics
With the right approach to establishing a diagnosis, it is not difficult to determine the presence of polyneuropathy in a person. As a rule, specialists have difficulty establishing the etiology of the disease. To get an accurate picture, the patient is prescribed a clinical analysis of blood and urine, determination of the levels of glucose, urea, and liver enzymes in the blood. Chest radiography and plasma protein electrophoresis are also performed. In some cases, patients are prescribed an ultrasound of the abdominal cavity. If there are indications, it is possible to conduct instrumental studies of the genitourinary system, gastrointestinal tract, lumbar puncture , and tests for the presence of rheumatic diseases .
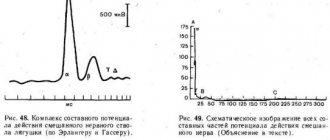
Needle ENMG
To study muscles, and this is necessary if there is a suspected pathology of the motor neuron of the spinal cord, for muscle diseases, or to determine the degree of muscle damage in neurological pathology, needle electromyography . A thin needle-electrode is inserted into the muscle being studied (reminiscent of an intramuscular injection). The electrical activity of the muscle is recorded at rest and under moderate tension. Needle ENMG is a more complex method from the point of view of interpretation and often takes more time and requires more qualifications from the doctor.
So what is stimulation ENMG?
The standard method for studying motor and sensory fibers of peripheral nerves looks simple on the surface. Electrodes are applied over the surface of the muscle or on the area of skin innervated by the nerve being studied (most often they look like a small patch or sticker), and the electrodes are connected to equipment (electroneuromyograph). In areas where the nerve is not very deep, using a special stimulator (vaguely reminiscent of the plug of any electrical appliance), the nerve is irritated by electric current discharges. The current is weak and absolutely safe, although the sensations may be unpleasant. As a result of electrical stimulation, a muscle contracts or a response occurs in the skin (in the case of studying sensory fibers). This response, or muscle contraction, is recorded by electrode stickers. The data obtained is analyzed by a doctor.
Causes of polyneuropathy
Acute polyneuropathy is provoked by a number of different factors. Most often, the acute form of the disease occurs under the influence of bacterial infections, which are accompanied by toxicosis . Also, the causes of acute polyneuropathy are identified as an autoimmune reaction, poisoning, the use of a number of medications, in particular antibiotics , as well as those drugs that are used during chemotherapy. The disease can develop in people suffering from cancer, which is accompanied by nerve damage.
Chronic polyneuropathy develops under the influence of diabetes mellitus, systematic alcohol consumption, decreased thyroid function, liver dysfunction, and a lack of vitamin B12 or excess vitamin B6 .
Most often today, the chronic form of the disease develops as a consequence of constant high blood sugar levels in a patient who does not take measures to reduce it. In this case, a separate form of the disease is determined - diabetic polyneuropathy . When establishing a diagnosis and prescribing treatment for polyneuropathy to a patient, the doctor must take into account those factors that influenced its development.
Causes and types of peripheral polyneuropathies
Peripheral polyneuropathy can develop due to many reasons:
- poisoning;
- nerve injuries;
- tumors;
- immunity disorders;
- lack of vitamins;
- alcoholic illness;
- problems with blood vessels;
- vasculitis;
- blood diseases;
- metabolic disorders.
Peripheral nerves are affected by the pathological process due to endocrine pathology, viral and bacterial infections, and the consumption of certain medications. Polyneuropathy can develop due to family history and in cancer patients. Often doctors cannot determine the cause of the disease.
Polyneuropathy can be toxic, vascular, infectious, somatogenic (appearing due to malfunctions of internal organs), autoimmune and hereditary. The following types of polyneuropathies are also distinguished:
- acute inflammatory demyelinating polyneuropathy (Guillain-Barré syndrome) - develops as a result of damage to nerve fibers by autoimmune antibodies;
- Serum polyneuropathy – occurs when antitetanus or antirabies serum is administered;
- diphtheria polyneuropathy – provoked by the diphtheria bacillus and its toxins;
- autonomic polyneuropathy – occurs mainly due to intoxication with carbon monoxide, hydrogen sulfide, manganese;
- uremic polyneuropathy – develops in chronic renal failure;
- paraneoplastic polyneuropathy – formed in patients with malignant neoplasms;
- diabetic polyneuropathy - occurs in 70% of patients who suffer from type 1 diabetes.
When the nature of the disease is unclear, doctors talk about idiopathic polyneuropathy. Based on morphological characteristics, two forms of peripheral nerve damage are distinguished: myelinopathy and axonopathy. Clinical manifestations of axonopathies and myelinopathies differ in the speed of muscle involvement in the pathological process, the course of the process, and the characteristics of the involvement of sensory, motor and autonomic fibers in the process. Certain forms of peripheral polyneuropathy have specific clinical symptoms that neurologists take into account when making an etiological diagnosis.
List of sources
- Levin O.S. Polyneuropathy: Clinical Guide / O.S. Levin. - M.: Medical Information Agency LLC, 2006;
- Angelcheva O.I., Zinovyeva O.E., Yakhno N.N. Neuromuscular disorders in chronic alcoholism. M.: MED-press, 2009;
- Zhulev, N.M. Neuropathies: a guide for doctors / N.M. Zhulev [and others]. -St. Petersburg, 2005;
- Skoromets A.A. Nervous diseases: Textbook. allowance / A.A. Skoromets, A.P. Skoromets, T.A. Skoromets. — Ed. 2nd, revised and additional - M.: MEDpress-inform, 2007;
- Gekht B.M., Merkulova D.M. Practical aspects of the clinic and treatment of polyneuropathies // Nevrol. journal - 1997. - No. 2. - P. 4-9.