Scalenus syndrome (also called scalenus syndrome) is a group of symptoms that include pain, numbness and weakness in the neck, shoulder or arm. The cause of symptoms is compression or damage to nerves or blood vessels in the costoclavicular space. The costoclavicular space is located between the collarbone and the upper rib, on both sides of the body. Most of the vessels (arteries and veins) and nerves supplying the arm pass through this space. Narrowing of this space can cause compression of nerves and blood vessels, which interferes with the normal functioning of the upper limb. The cause of the narrowing can be various conditions, such as injury, obesity, congenital anomalies, and poor posture. But sometimes it is not possible to find out the specific reason for the narrowing.
Description of the pathology. Pathogenesis
Scalenus syndrome is caused by the anatomy of this location. Having learned the details, you will immediately understand who is to blame and what to do?
The scalene muscles are located vertically along the spine. With their upper ends they are attached to the sides of the vertebrae, and with their lower ends they are attached to the two upper ribs, which are located in the uppermost part of the chest, deep behind the collarbone. It is here, above and behind the collarbone, at the border of the neck and chest, that the anterior scalene muscle syndrome develops. The scalene muscles owe their name to their peculiar arrangement - ledges. If a person were lying on his back, the muscles would look like steps. The bottom step is the posterior scalene muscle, the second is the middle step, and the topmost step is the anterior scalene muscle. This is exactly how ancient Roman anatomists saw these muscles and gave them the appropriate name.
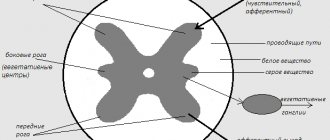
Between the anterior and middle scalene muscles are the subclavian artery and nerves that run from the spine to the arm. And although it is quite narrow here, like tunnels, if the muscles are healthy, then the nerves and arteries are not in danger. Firstly, because healthy muscles are elastic and soft, and secondly, both the muscles themselves and the nerves with the artery are covered with a dense slippery membrane - fascia. This ensures they slide smoothly relative to each other and protects them from any pinching when moving the head and neck. However, with pathology, everything changes - the anterior scalene muscle spasms and its tone increases sharply. This causes pain and, in addition, a muscle that is stretched like a string can squeeze the nerves and arteries in the narrow tunnel that we talked about above.
Thus, with anterior scalene muscle syndrome, the patient will experience one of two possible options for the development of this pathology. The first one is relatively easy. It causes muscular-tonic (myofascial) syndrome. Trigger points appear in the muscle, triggering referred pain in the neck, shoulder, chest, shoulder blade and arm. The second one is more difficult. Here the spasmed muscle pinches a nerve or vessel. In this case, in addition to pain, neurovascular pathology also occurs, or, as they say in medicine, neurovascular pathology. By the way, anterior scalene muscle syndrome is the most common neurovascular pathology of the neck. It is also called scalenus syndrome or Naffziger syndrome.
For reference: scalenus – staircase (latin). Howard Christian Naffziger is an American neurosurgeon who was one of the first to describe neurovascular pathology caused by the anterior scalene muscle.
Other meningeal signs
The following important symptoms of meningitis are common to adults and children:
- Kernig's syndrome . It consists in the fact that the subject cannot straighten the leg at the knee if it is already bent at the hip joint.
- Flatau reflex . With a sharp passive (by the doctor’s hand) flexion of the patient’s neck, the pupils dilate.
- Hermann's sign . While the doctor presses the patient's head to the chest, the patient's big toes extend.
- Mondonesi syndrome . When pressing on the eyeballs through closed eyelids, the examined patient feels pain, and this is a sign of meningitis.
- Matseven's symptom - a specific “sound of a cracked pot” is heard when examining the skull with a finger or a percussion hammer.
All these symptoms and specific reflexes are included in the meningeal symptom complex.
Symptoms of the syndrome
As mentioned above, the symptoms of anterior scalene muscle syndrome can be either purely painful, due to muscle spasm, or neurovascular disorders are also added to the pain, due to compression of the nerves and subclavian artery.
Pain is the first and most debilitating symptom
; it extends from the shoulder joint down the arm and can extend to the little and ring fingers. Sometimes the pain moves to the chest or back of the head. The pain often worsens at night. The pain also intensifies when turning the head, when moving the arm to the side and when taking a deep breath. The scalene muscles are accessory muscles of inspiration. When you inhale deeply, they contract and pull the upper ribs and chest upward. This causes the chest to rise and more air to enter the lungs. This is why anterior scalene muscle syndrome often develops, due to its prolonged overload, in people suffering from shortness of breath or some diseases of the respiratory system, for example, colds. By the way, not only shortness of breath or a cold can cause muscle strain. There is a so-called hyperventilation syndrome, when diaphragmatic breathing is impaired against the background of psychosomatic, anxiety or psychovegetative disorders. In these cases, the auxiliary respiratory muscles, primarily the scalene muscles, are forced to completely take over the performance of respiratory movements. This is an excessive burden for them, a cause of overexertion and the starting point for the development of anterior scalene syndrome.
Second group
symptoms of anterior scalene muscle syndrome are manifested by sensations of tension in the neck muscles, heaviness, numbness and weakness in the arm, up to severe paresis (incomplete paralysis) of the hand and muscle atrophy. However, it should be noted that paresis and atrophy of the hand are extremely rare - only in very advanced cases.
Third group
– vascular symptoms of anterior scalene muscle syndrome: swelling of the arm, its cyanosis, coldness, weakening of the pulse, up to its complete disappearance when raising the arm up or tilting and turning the head. In addition to the subclavian artery, lymphatic vessels are often affected. Their clamp disrupts lymph circulation. This leads to stagnation and edema, which manifests itself as swelling in the supraclavicular fossa (Kovtunovich's pseudotumor).
And the fourth group
– vegetative-trophic symptoms of the anterior scalene muscle syndrome are manifested by brittle nails and a decrease in hair on the arm. However, the manifestation of vegetative symptoms, too, is noted only against the background of long-term and advanced cases, which, fortunately, does not happen often. A modern person, especially one living in a large city, will rarely wait until such a stage to see a doctor.
Causes
SLM occurs as a result of compression of the nerves or vessels at the exit of the chest. Main reasons:
- Trauma – A traumatic episode may cause damage to the bone or soft tissue at the thoracic outlet. Most people with SLM have a history of one or another episode of an accident, injury at work or at home.
- Congenital anomalies, such as an extra rib or a tight ligament connecting the spinal column to a rib, can reduce the costoclavicular space.
- Poor posture - sagging shoulders or excessive forward tilt of the head can put compression on the area where nerves and blood vessels exit the chest.
- Frequent, repetitive movements can wear down the tissues and lead to SLM. An example would be movements associated with raising the arm (the collarbone lowers and the costoclavicular gap decreases), such as swimming, baseball, tennis, weightlifting.
- Other causes: Weight gain (pregnancy or obesity), overdeveloped neck muscles (from weightlifting or martial arts), or holding your arms in one position for a long time (working on a computer) can put additional pressure on nerves and blood vessels. Diseases that impair nerve function, such as hypothyroidism and diabetes, may be predisposing factors for neurogenic SLM.
What happens if you trigger scalene syndrome?
The most dangerous complication of anterior scalene muscle syndrome is thrombosis in the subclavian artery system. For a better understanding, it must be said that the vertebral arteries depart from the left and right subclavian arteries, from which, in turn, the arteries of the brain begin. Thrombosis in this system is a truly deadly complication of anterior scalene syndrome and requires immediate surgical intervention.
The second serious complication is paresis (incomplete paralysis) and atrophy of the hand muscles.
Another striking and unpleasant complication is a violation of the biomechanics of the neck and body as a whole. This point is a little difficult to understand for a non-specialist, but now we will understand it. So. With prolonged tension of the scalene muscles, they shorten. This increases cervical lordosis and moves the head forward. To compensate for balance and center of gravity, the muscles in the back of the neck are forced to tighten and, accordingly, overload. Soon, due to overload, secondary pain trigger points will form in the back muscles of the neck, and myofascial syndrome will develop. Further, if left untreated, increased cervical lordosis will lead to compensatory curvature of the spine in the thoracic and lumbar regions, because it is forced to seek balance. Curvature of the spine disrupts the distribution of axial loads on the intervertebral discs and, thus, opens the way to the formation of protrusions and disc herniations not only in the neck, but also in any other compensatory overloaded place in the spine.
Myofascial scalene syndrome
That is why timely consultation with a doctor, early detection and proper treatment can avoid all these serious complications of anterior scalene syndrome.
Diagnostics
Diagnosis of anterior scalene syndrome is based on a typical clinical picture and always begins with an examination. During such an examination, most patients will experience swelling in the supraclavicular region. This is the so-called pseudotumor (pseudotumor) of Kovtunovich. It occurs due to compression of the lymphatic vessels by the anterior scalene muscle. Also, during the examination, pay attention to the hand - it may be swollen and slightly bluish. In advanced cases, more pronounced changes will be noted, even trophic ones.
When palpating the anterior scalene muscle, it will be sharply tense and painful, and this will also cause increased pain in the neck with possible spread to the arm.
Neurological examination - checking sensitivity, reflexes, etc. - identifies sensory, motor and autonomic disorders.
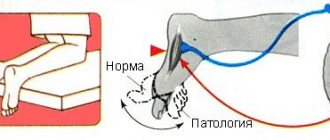
Spasm test. It is carried out to identify myofascial syndrome of the scalene muscles. You need to turn your head as far as possible in the painful direction and firmly press your chin to your collarbone. The scalene muscles will contract and trigger points in them will be activated. As a result, the patient will feel increased pain.
Adson's test: if you raise your arm on the side of the anterior scalene muscle syndrome and tilt your head here, then where you usually check the pulse at the wrist, there will be no pulse.
Doppler ultrasound (USD) of the neck vessels also has a certain diagnostic value, especially taking into account that the vertebral artery, which supplies the back of the brain, departs from the subclavian artery. And this entire vascular network may suffer from compression of the subclavian artery, which in turn threatens cerebrovascular accident or thrombosis.
Electroneuromyography (ENMG) is considered a generally accepted diagnostic method. Although, at the initial stages of pathology, its information content is not high enough, and sometimes even fraught with erroneous conclusions.
Therefore, the best test for all stages of anterior scalene syndrome is good old manual muscle testing.
Sign up for scalene muscle diagnostics
- Undergo a comprehensive diagnostics of the scalene muscles. We will conduct palpation, neurological examination, spasm test, Adson test and manual muscle testing: we will test the muscles for the presence of active and latent trigger points.
- Diagnostic duration is 30 minutes. This is a full-fledged examination, and not a 2-minute “feeling” for show.
- The diagnosis is carried out personally by Dr. Vlasenko A.A., a doctor with 30 years of experience, an expert in the treatment of myofascial and radicular syndromes.
Dr. Vlasenko Alexander Adolfovich, neurologist, manual therapy doctor
Sign up for diagnostics
Treatment of scalene syndrome
Effective treatment of scalene muscle syndrome requires a clear understanding of the cause and mechanism of the disease, as well as an integrated approach to treatment.
For the treatment of anterior scalene muscle syndrome, the following are used: drug treatment, physiotherapy, exercise therapy, massage, surgical methods and manual therapy. Of course, one should start with conservative methods, among which manual therapy occupies a key place. But first things first.
Manual therapy
Don't think that manual therapy for scalene muscle syndrome means realigning the vertebrae or anything like that. If you thought so, you were deeply mistaken. Modern gentle manual therapy is a set of methods aimed at eliminating pain, normalizing muscle tone and restoring the full range of movements of the affected region and the entire musculoskeletal system as a whole.
All methods of manual therapy for scalene muscle syndrome can be divided into direct and indirect; active and passive; soft and trusting. But, one way or another, the main part consists of the so-called neuromuscular methods, in which the impact occurs through soft tissues: muscles, fascia, etc.
In manual therapy of scalene muscle syndrome, neuromuscular methods are mainly used. They include: post-isometric relaxation, reciprocal inhibition, isotonic concentric and eccentric contractions, positional relaxation techniques, strain-counter-strain, myofascial release, etc. As well as direct manual methods: ischemic compression, pressure on trigger points, acupressure, transverse friction, soft tissue mobilization, deep tissue massage, etc.
Correct and adequate use of all these numerous soft methods gives an amazing therapeutic effect in manual therapy of scalene muscle syndrome.
Treatment
Drug treatment
- NSAIDs are non-steroidal anti-inflammatory drugs. These medications help reduce pain and inflammation (swelling and redness). For example: aspirin, ibuprofen (Advil), naproxen (Aleve), and celecoxib (Celebrex) movalis
- Muscle relaxants – Often used to treat muscle spasms, these medications can relieve pain by relaxing the muscles. Cyclobenzaprine (Flexeril), carisoprodol (Soma), diazepam (Valium), methocarbamol (Robaxin), and tizanidine (Zanaflex).
- Neuropathic drugs - The principle of their action is based on changes in the neurotransmitter transmission of pain impulses to the spinal cord and brain. Medicines that may help reduce pain by affecting neurotransmitters include fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), venlafaxine (Effexor), amitriptyline (Elavil), imipramine (Tofranil), desipramine (Norpramine) ), doxepin (Sinequan), and amoxapine (Ascendin).
- Opioids - Narcotic analgesics are used only for very severe pain after conventional analgesics have been exhausted. A combination of opiates with NSAIDs is possible (to enhance the analgesic effect).
Exercise therapy
Physical therapy is one of the most important components of SLM treatment. Selecting certain exercises helps improve posture and proper distribution of muscle loads. Exercises help increase range of motion in the limb. Stretching and strengthening the shoulder and pectoral muscles can help increase and relieve pressure on the nerves and blood vessels in the costoclavicular space. • There is a wide range of motion, both passive and active.
Physiotherapy
Various physiotherapeutic techniques can relieve swelling, inflammation, restore blood circulation and reduce compression of nerves.
Manual therapy
The use of certain manual therapy techniques allows you to mobilize the spine and ribs and increase the range of motion in the shoulder joint.
Blockades
Sometimes used for differential diagnosis and treatment. But, taking into account the anatomical features of this area, injections should be carried out by a doctor with experience in performing such manipulations.
Acupuncture (acupuncture)
Acupuncturists believe that a healthy body contains channels through which energy flows. When these channels close, the energy is blocked, which leads to various diseases. Needles are inserted into certain points (biologically active). In certain cases, acupuncture can reduce pain and restore conduction along nerve fibers.
Massage can help relieve stress and relax tense muscles. Massage helps increase blood flow to body tissues and helps muscles get rid of metabolic waste products.
Advantages of treatment at the Spina Zdorova clinic
- Guarantee of complete and qualified treatment. The word “full” is key in our work.
- High qualifications and extensive practical experience - 30 years.
- We consider each case individually and comprehensively - no formalism.
- Synergy effect.
- Guaranteed fair treatment and fair price.
- The location is a stone's throw from the metro in the very center of Moscow.
Other methods of treatment. Physiotherapy
Physical therapy for scalene syndrome is a supportive treatment. The most commonly chosen procedures are:
Sinusoidal modulated currents (SMC) or – second name – amplipulse therapy. This procedure perfectly copes with pain and muscle spasms, while simultaneously restoring their blood supply and nutrition.
Electrophoresis is a classic of physiotherapy. A less powerful, but gentler method of treatment. Suitable where there are contraindications for SMT therapy.
Ultrasound (UT) is, in fact, a micromassage. Propagating deep into the tissue, ultrasound transmits its vibrations to these tissues, thereby improving their drainage and trophic functions. Deep swelling, stagnation and inflammation disappear, blood circulation and tissue nutrition are normalized. Due to this, the pain syndrome is reduced.
Magnetotherapy – increases microcirculation, thereby eliminating congestion, swelling, inflammation and reducing pain.
Surgical treatment
Surgical treatment of scalene muscle syndrome is used only in advanced cases of the neurovascular stage of the syndrome, when compression of the nerves and subclavian artery could not be eliminated by other means. As we said above, conservative treatment is not always able to solve the problem, and then surgery becomes the only option.
During surgical treatment of scalene muscle syndrome, the muscle itself and adjacent tissues compressing the nerve and artery are dissected. To prevent relapses, muscle resection is carried out over as large an area as possible.
Once again, we draw your attention to the fact that it is advisable to consider the issue of surgical treatment of scalene muscle syndrome only when all conservative treatment methods have been completely exhausted.
Don't let your illness get worse! Timely consultation with a doctor allows you to avoid surgery!
Prevention
Prevention of scalene muscle syndrome is aimed at preventing the circumstances that lead to the occurrence of the syndrome. What are these circumstances?
Firstly, scalene muscle syndrome very often occurs as one of the links in the pathology of the intervertebral discs of the cervical spine. Therefore, timely consultation with a doctor and elimination of any pathology of the spine and discs in the early stages is the most important preventive action.
Secondly, since the main provoking factor in the development of the syndrome is prolonged forced positioning of the head and arms, which usually happens during sedentary work, it means that it is necessary to take regular breaks. Keep in mind that the optimal time for continuous work is 45 minutes, like a school lesson (plus or minus 15 minutes). In other words, try to change your body position - it doesn’t matter how exactly - get up, stretch, walk - the main thing is to make a short-term change in position. In general, approach this issue creatively and act according to the circumstances.
Thirdly, very often scalene muscle syndrome occurs against the background of sports overtraining, so people who are actively involved in sports need to be aware of this and be attentive to the signals of their body.
In general, this wish is not only for lovers of an active life, but for everyone - do not ignore “body language”, because many problems arise from neglecting these signals. As practice shows, almost all patients who consult a doctor with scalene muscle syndrome describe the onset of the disease in the same way: “It all started a long time ago and at first it didn’t bother me much.” This is a classic onset - gradual and not very painful. This is how the body sends us signals, giving us the opportunity to quickly correct everything. And we jam the signals with analgins, thinking that “everything will resolve itself.” Alas, this is not true. From a certain point, the disease will rush like a rapid avalanche, and it will be very difficult to stop it and eliminate the consequences. Therefore, we draw your attention once again - do not ignore “body signals”, do not let yourself go and do not bring the situation to a crisis.
Diagnostics
Diagnosing SLM can be difficult. Symptoms vary in nature and severity, depending on the individual. In addition, the symptoms are similar to those that occur with other diseases (for example, damage to the rotator cuff, diseases of the cervical spine leading to compression of the roots, etc.). Medical history and physical examination help to clarify the onset of the disease, the nature of symptoms, and their dependence on body position. In addition, there are external signs of this disease (swelling of the arm, discoloration, loss of sensitivity, limited range of motion in the shoulder). During a physical examination, the doctor may carry out procedures (manipulations) to identify symptoms (pulse pressure in the arms in various positions of the arm, both sick and healthy).
Instrumental research methods
- Electromyography (EMG) – EMGs help test how nerves and muscles are functioning. Small needle electrodes are inserted into the muscle where the problem is. Electrodes measure the electrical activity of the muscle innervated by a particular nerve. The pathological response of a muscle provides information about the condition of the nerve going to that muscle. In addition, EMG allows you to determine the speed of impulse transmission along a nerve fiber. This is done using electrodes placed on the skin. The speed of impulse conduction along each nerve fiber has a certain average value, and a deviation indicates damage to the nerve fiber.
- X-ray allows you to diagnose bone changes in the chest and ribs (the presence of an additional cervical rib).
- Laboratory examinations - general blood tests, blood for hormones, blood for sugar help in diagnosing SLM.
- Magnetic resonance imaging (MRI) - allows you to visualize the soft tissues of the body MRI to find out the cause of compression of a nerve or vessel.
- Computed tomography (CT) allows you to more clearly visualize changes in bone tissue.
- Ultrasound examination – Using an ultrasonic wave, it is possible to visualize soft tissues and blood vessels, the presence of blood clots and stenoses.
- Angiography – X-ray examination using contrast is used to diagnose vascular lesions. Angiography of arteries and veins is used to diagnose blocks and other problems in the blood vessels.