Double vision
Double vision is a very unpleasant symptom. Normally, a person has binocular vision. We look with two eyes, each eye sends its own signal to the brain, they overlap each other, and we see a stereoscopic single picture. A single picture is necessary for us to feel confident in space. If we see two images at once, it is extremely tiring. The brain gets tired trying to coordinate signals and is unable to do so. With severe double vision, headaches, dizziness, and possible attacks of nausea are typical. A person has difficulty estimating distances to objects, and it may be difficult for him to navigate in space.
Vision system
We rarely think about how exactly vision works until problems arise with it. In a normal state, the visual process occurs like this:
- the object is projected onto the retinas of both eyes, right and left,
- the brain combines information from both eyes, producing a complete picture.
Otherwise, this connection is broken, and the image doubles.
Let's take a closer look at the causes and treatment of double vision.
Symptomatic signs
Signs of amblyopia cannot always be detected in a timely manner, since with a mild degree of the disease there is no clinical picture, and only a qualified specialist can suspect the presence of disorders.
Symptoms of amblyopia appear as follows:
- decreased vision in one or both eyes that cannot be corrected with glasses;
- visual perception of objects and their spatial characteristics (size, location of objects relative to each other) is disrupted;
- the symptoms of strabismus (if present) intensify, that is, the asymmetrical arrangement of the corneas relative to the inner corners and outer edges of the eyelid becomes more noticeable;
- The child does not absorb visual information well.
What is diplopia
Diplopia (double vision) is the inability to see a single image of objects located in the vision zone.
The brain provides a binary image of a single object. The image can be deformed in different ways: vertically and horizontally or diagonally. In this regard, a person is not able to see a clear, unified picture of an object. The pathology causes very unpleasant sensations for patients, causing eye fatigue, dizziness and disorientation in space.
It is important to understand that this is not an independent illness, but a concomitant signal of a systemic disease. In medical practice, almost all causes of double vision have been studied, and proper treatment in most cases leads to a positive result.
Nature of appearance and types of diplopia
In order to diagnose diplopia, it is enough to consult an ophthalmologist. After all, sometimes this illness is a consequence of other, more serious neurological or oncological diseases.
This defect occurs when a visible object is projected onto asymmetrical areas of the retina. Therefore, the brain, when processing the signal, does not reduce it into a single picture. The image can bifurcate in different directions and, as a rule, is a consequence of dysfunction of the oculomotor system. The muscles bring the eyeballs into non-identical positions, causing different focus.
If you notice symptoms of diplopia, you should definitely consult a specialist. Especially if the disease has been with you for a long time.
Persistent double vision comes in two forms:
- Binocular . The most common violation. A defect caused by the lack of parallelism of the visual axes in the eyes. Often accompanied by or resulting from strabismus. Often occurs after injury, but is not always permanent.
- Monocular . A rarer form that can begin against the background of organ injury, corneal degeneration (astigmatism), damage to the visual cortex of one of the cerebral hemispheres, or clouding of the lens. The main difference from the binocular form is that double vision can occur even when the affected eye is closed.
There are also forms of diplopia that are temporary:
- Strong-willed . Conscious “defocus” of the gaze. Thanks to which, the ability to look, as it were, “through” an object appears.
- Temporary . Typically caused by alcohol intoxication, traumatic brain injury, or a side effect of certain medications. However, if the symptoms become permanent, it is necessary to check the organs of vision and systematically treat the disease.
Determination of the angle of strabismus
When amblyopia develops against the background of strabismus, the doctor determines the angle of strabismus according to Hirschberg. To do this, the child is asked to look at the ophthalmoscope, after which the doctor records the light reflections. Normally, the glare is projected in the middle of the pupil, but with strabismus - at the edge of the pupil, within or beyond it, which determines the angle of deviation.
Determining the nature of visual fixation is the most important diagnostic procedure for any form of amblyopia, since the treatment regimen depends on visual fixation.
Get a complete vision examination at the Lege Artis Eye Clinic
It's time to correct your vision!
Make an appointment by phone:
8(804) 333-02-14 Free call
Photos of treatment stages
Patient : 30 years old
Diagnosis : Double vision + strabismus after an accident
1. Several operations to compensate for double vision (the last two at the Hemholtz Research Institute of GB)
2-3. The results of the operations are not visible after a year; double vision progresses.
4-5. Double vision remained plus the lack of eye mobility towards the temple was added
6. Prismatic glasses were prescribed to compensate for double vision and restore eye mobility when worn continuously for a year, treatment continues.
Need specialist advice?
Operating procedure
Clinical picture of double vision
Many modern clinics offer intervention services for vision problems. But few can guarantee that the patient will not gradually begin to lose visual acuity after a year. That is why it is so important to understand everything and make the correct diagnosis.
Pathology has an extremely long list of causes for its occurrence. Starting from traumatic brain injuries, alcohol intoxication, migraines and abscesses, ending with stroke and oncological diseases such as cancer and brain tumors.
In most cases, double vision indicates a neurological condition and requires treatment of the underlying cause at the level of the peripheral nervous system or brain.
Causes of double vision
Speaking about the monocular form of the disease, it is worth considering the following reasons for its occurrence:
- Astigmatism, since with it only one eye has a split.
- Corneal dysfunction. Such as dryness, scarring and various infections.
- Also, against the background of clouding of the lens, a possible cause may be cataracts.
As for the binocular shape, the main reasons may be:
- Strabismus. It can be both a cause and a consequence of a disease.
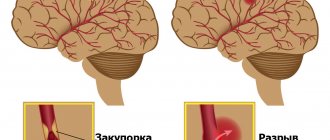
- Various diseases characterized by impaired vascular function - cerebral aneurysm, stroke, hypertension.
- Diabetes. Due to damage to nerve endings.
- Autoimmune diseases such as myasthenia gravis and multiple sclerosis, which affect the central nervous system.
- Injuries. Traumatic brain injury is an extremely common cause of diplopia.
Considering a wider range of causes, diplopia can be caused by the following diseases:
- Neuropathy caused by B vitamin deficiency.
- Cervical osteochondrosis.
- Migraine, epilepsy, hypertensive crisis, stroke.
However, double vision has other causes. A correct clinical picture is possible only with timely diagnosis and detection of the localization site. For example, there is also a paralytic form of diplopia, it is characterized by paralysis of one or more eye muscles:
- When the rectus ocular muscles are damaged, the patient sees a parallel bifurcated image.
- With pathology in the oblique muscles, the image is located one above the other.
Often, the provocateurs of this visual disorder are also:
- Complications of various infectious diseases.
- Aneurysm of the carotid artery, leading to compression of the optic nerve.
- Thyroid dysfunction.
- Tumors inside the skull.
- Endocrine ophthalmopathy.
- Inflammation in the brain: meningitis, encephalitis.
Examination of a child with amblyopia
Congenital ophthalmic pathology, such as a cataract, cataract or ptosis, is detected immediately after birth if it is pronounced and obvious. However, examination and consultation with a pediatric ophthalmologist, taking into account the above data, is mandatory in any case.
Parents (usually the mother) should be prepared to provide the consultant with the most complete anamnestic information possible: ophthalmic heredity on both lines, the nature of pregnancy and childbirth, infections suffered by the child, injuries, stressful situations; Peculiarities of the child’s behavior observed at home that may be related to vision (squinting, blinking too often, rubbing his eyes, sometimes squinting slightly, etc.); neurological status; previous treatment received and its success, and many others.
Accurate visometry, the measurement of visual acuity, is impossible in early childhood, but these data are necessary to diagnose amblyopia. Pediatric ophthalmologists use indirect assessment techniques and take into account known cause-and-effect relationships (for example, the development of amblyopia is always accompanied by congenital unilateral cataracts).
During the initial ophthalmological examination, attention must be paid to the shape, size and symmetry of the palpebral fissures, the condition and tone of the eyelids, and the consistency of movements of the eyeballs. Pupillary and psychomotor reactions to light are assessed. Using an ophthalmoscope, the condition and light transmittance of transparent ocular structures and media (cornea, lens, vitreous body), as well as the status of the fundus, are examined.
Speaking about indirect, but quite effective methods for assessing refraction, one cannot fail to mention skiascopy - one of the most well-known and widely practiced methods for the early diagnosis of myopia, farsightedness and astigmatism.
Conventional ophthalmic equipment is used: a powerful light source and a head mirror. A directed beam illuminates the pupil; Normally, there is a reflection from the fundus of the eye - the so-called. red reflex. By turning the mirror, the doctor notes the displacement of the shadow (by the way, “skia” means “shadow” in Greek), using special lenses and a ruler, evaluates its direction and deviation. The presence of a refractive error, its nature and severity, including in young children, can be diagnosed using the skiascopic method. The disadvantages are lower measurement accuracy compared to visometry with interchangeable lenses, as well as the need to dilate the pupil. As a mydriatic drug, for children under 1 year of age, a 0.5% solution of tropicamide is usually used 20 minutes before the test; patients from 1 to 3 years of age are instilled with a 0.5% solution of atropine; from 3 years of age, 1% atropine is instilled several days later. before inspection.
Visometric measurement of visual acuity, necessary for the final establishment (or exclusion) of the diagnosis of amblyopia, becomes possible from the moment the child learns to understand and follow simple instructions, answer questions like “What is shown in the picture,” etc. The main diagnostically significant sign of amblyopia is the impossibility or ineffectiveness of correcting impaired vision with glasses.
In addition, the ability of central fixation is examined. The diagnostic method is simple and, like skiascopy, is based on the analysis of the behavior of the shadow under narrowly focused illumination of the fundus through a pre-dilated pupil. An opaque point with a diameter of 3 mm is placed in the center of the ophthalmoscopic lens. The child looks with only one eye (the other is covered) and must focus his gaze on this point. Normally, a reflex is observed from the macular (central and most light-sensitive) zone of the retina, and the shadow is located clearly in the center. Any other position of the shadow indicates impaired fixation. In this case, eccentric fixation can be either stable (the shadow is motionless) or unstable (the shadow is constantly moving).
One of the standard methods for assessing binocular vision is the color test. A special device is used, the main element of which is a disk with four circles illuminated from the inside: two green, red and white. The patient is put on glasses with light filters - red glass on the right eye and green on the left - and placed in front of the disk so that the right eye sees only the red circle, and the left only the other three. With normal binocular vision, a person sees a red circle, both green circles, and a white circle (white may alternately appear red and green). In case of binocularity disturbances, various other options are possible - for example, two red, three green, etc. - each of which is known and informative for the ophthalmologist, who, based on the nature of the picture observed by the patient, establishes the type of dysbinocularity (monocular vision, simultaneous, etc.).
Double vision: treatment and diagnosis
Consultation cost 3000 rubles
The risk of developing an underlying disease and irreversible visual changes is a sufficient reason to immediately consult a doctor. Identifying the causes will create the prerequisites for the correct diagnosis and appropriate treatment regimen.
Diagnostics
- History taking
When compiling a medical history, first of all, attention is paid to the patient’s most recent injuries and illnesses.
- Detecting the form of diplopia
At the next diagnostic stage, the form of diplopia (binocular/monocular) is determined by tests.
- In-Depth Study
It is necessary to identify the degree of discrepancy between the patient’s images (vertically, horizontally) through a test.
- Quantitative Research
At this stage, the prism compensator allows you to correct diplopia by combining double images to set the number of prism diopters.
- Diagnostic analysis
The degree of functionality of the extraocular muscles is assessed using the Haabu method. Namely, by the method of infrared videooculography and electrodynamic scanning, as a result of which hyperfunction of the oculomotor muscles is detected.
Risk factors
Some pathological conditions and unfavorable factors can lead to the development of functional disorders of the visual analyzer:
- ametropia - deviation of the refractive power of the eye from age-related values;
- strabismus;
- cerebral palsy;
- mental development disorder;
- III and IV degree of prematurity of the child;
- underweight newborn;
- the presence of ophthalmological diseases in close relatives (amblyopia, strabismus, lens opacity).
The presence of bad habits in pregnant women (smoking and drinking alcohol) increases the risk of developing visual system dysfunction several times.
Basic principles of treatment
Binocular disorders
- Depending on the underlying cause of the disorder, treatment will be prescribed by a specialist in a specific field. However, a neurologist and a neurosurgeon are the doctors you should consult first.
- In case of injury to the organ of vision, a comprehensive examination by an ophthalmologist is necessary.
- Corrective therapy involves wearing sphero-prismatic glasses, which neutralize the double vision syndrome. Regular eye exercises will be an effective addition.
Stages of severity of pathological processes
Amblyopia manifests itself from a slight decrease in visual function to a sharp deterioration in the visibility of objects. In the first stage of the disease, it is almost impossible to timely detect visual impairment in a child. A weak degree of amblyopia (visual acuity 0.4-0.8) is diagnosed during preventive examinations by an ophthalmologist.
The average degree (visual acuity 0.2-0.3) of impairment may also have no clinical signs and is detected during an ophthalmological examination.
With a high degree of amblyopia, the child’s vision deteriorates (visual acuity 0.1-00.5), visual perception of information decreases.
The highest degree of impairment (from 0.04 and below) is manifested by a sharp decrease in vision; the child cannot see objects.