Epilepsy in adolescence is most often a continuation of a disease that began in childhood. Epileptic seizures in adolescents can either increase or decrease. Puberty is associated with global changes in the body, preparation for growing up and puberty. Therefore, it is quite difficult to predict how epilepsy will manifest itself. To do this, the patient must be regularly monitored by a neurologist or epileptologist. The attending physician evaluates the results of the therapy, studies the dynamics of epileptic seizures, and changes in tests. Based on research data, the doctor makes recommendations to normalize the teenager’s condition. Epilepsy can also develop in adolescence as a result of a previous illness or brain injury. In this case, the child must undergo a comprehensive examination to make the correct diagnosis. Epilepsy brings significant discomfort to everyday life, which is especially difficult for adolescents due to emotional changes and social development. Therefore, the child must be shown to a qualified specialist as quickly as possible in order to prepare effective treatment.
The Yusupov Hospital provides diagnostics and high-quality treatment of various types of epilepsy. The highly qualified doctors, as well as the modern technical equipment of the hospital, make it possible to create the most optimal therapy that reduces the manifestations of epilepsy and allows you to completely eliminate the disease.
Epilepsy: general information
Epilepsy is a chronic neurological disease that occurs when there is excessive electrical activity in the brain. Patients with epilepsy suffer from recurrent seizures. These are short-term involuntary spasms. They may affect one part of the body or the entire body. Sometimes these attacks cause people to lose control of their bowel and bladder functions. Loss of consciousness is also possible.
If a patient has an attack: first aid
What NOT to do with a patient during an epileptic attack:
- Do not use any object to force the jaw open.
- Do not give the patient any medications or liquids.
- Do not try to restrain jerky movements.
- Do not hit the patient on the cheeks or pour water on them.
- Do not perform artificial respiration or cardiac massage.
What to do during an attack?
- When a diagnosis of epilepsy is made, emergency specialized medical care is required only in cases of a series of seizures.
- If the ambulance has not arrived yet, make sure that the patient does not injure his head.
- Turn the person on his side, hold him, make sure his head is turned to his side.
- Do not put anything in the mouth, otherwise you will damage the patient’s teeth, palate, or tongue. Due to the spasm of the chewing muscles, he may bite off your finger.
- Do not be alarmed; during an attack, foam may come from the mouth or even blood if the person bites his tongue.
- After the attack, the patient is usually disoriented for 5-10 minutes. You need to talk to him calmly. Tell us who you are, where he is and what happened to him.
- Diabetics using insulin may experience cramps due to low blood sugar. Then after an attack, give the person a spoonful of honey or candy, but only if you know for sure that he is using insulin.
- Typically, after an epileptic attack, people feel very tired and confused. They need rest and sleep to regain their strength.
Kovalchuk Maria Sergeevna
expert
UZ "GSSMP Minsk"
The exact mechanisms of development of epileptic seizures are still unknown. It is assumed that seizures are a consequence of an imbalance in the processes of excitation and inhibition in the cerebral cortex. Normally, they equalize each other, creating an optimal level of brain activity. However, with epilepsy, excitatory activity increases markedly. Nerve cells begin to synchronously produce electrical discharges, which can spread to other parts of the nervous system. This leads to an attack¹.
According to the World Health Organization (WHO), there are approximately 50 million people worldwide with epilepsy². Up to 80% of all patients live in low- or middle-income countries. WHO estimates that up to 70% of people with epilepsy can live full, seizure-free lives. This requires timely diagnosis and adequate therapy.
5 myths about epilepsy
1. This is a mental illness.
Many people confuse mental illness with neurological illness. Epilepsy is a “classical” neurological disorder. Therefore, this problem is dealt with by neurologists and neuropathologists, and not by psychiatrists. At the same time, a patient with epilepsy may also suffer from mental disorders, but this will only be a concomitant disease.
2. Epileptics suffer from dementia.
Some people with epilepsy actually have dementia. But this statement is also true for people with hypertension, atherosclerosis and any other diseases. This does not mean that dementia is a consequence of a specific pathology.
In the vast majority of cases, epilepsy does not have any effect on the intellectual abilities of patients. Such great minds as Socrates, Thomas Edison, Isaac Newton, Alexander the Great and many others suffered from this disease.
3. A person with epilepsy needs to completely change their lifestyle.
This is wrong. Thanks to modern treatment methods, a person with epilepsy is in most cases able to lead a normal life. Such people study in schools, universities, work and start families. It is noteworthy that mental activity, physical labor and sports reduce the number of attacks, easing the course of the disease.
But there are also restrictions for people with epilepsy. For example, they cannot drive vehicles or machinery, perform military service, or work in potentially hazardous enterprises.
4. Hyperactive children are more likely to become epileptic.
This myth is well established even among doctors. Excessive excitability, hysteria and sudden mood swings may be mistakenly perceived as the first signs of epilepsy.
Some children sometimes have affective-respiratory attacks. This is a short-term breath holding, which in some cases is accompanied by loss of consciousness. Doctors may prescribe anticonvulsants to such children, believing that this is the first manifestation of epilepsy. However, increased excitability and affective-respiratory attacks have nothing to do with epilepsy. Here you need a consultation with a competent neurologist and differential diagnosis.
5. You can only get epilepsy in childhood.
In most cases this is true. In approximately 70% of patients, their first epileptic seizures occurred in childhood. However, the second peak incidence of epilepsy occurs in old age. This is due to a number of neurological diseases (stroke, brain tumors and others), which often develop in old age.
Epilepsy: classification of seizures
Today, in modern world medicine, it is customary to distinguish two main groups of seizures caused by epilepsy. Typically, each of them is determined by the original source, which most often begins to be localized in areas of one or another part of the brain, thereby causing an epileptic discharge.
If an attack occurs in certain areas of the cerebral cortex, it is usually called either a partial or focal attack. After which, epileptic discharges spread not to individual areas of the cortex, but to almost the entire gray matter as a whole. Epileptic seizures can also be characterized by simultaneous discharge activity in both hemispheres of the cerebral cortex and are called a generalized seizure.
If the focus of the main activity is in the frontal and temporal lobes, or in rare cases in the occipital areas, it is usually called a focal epileptic seizure. Those types of seizures that doctors are unable to logically attribute to either of the two groups are called unclassifiable.
Symptoms of epilepsy
Symptoms and signs of epilepsy vary. First of all, this is due to the fact that an attack can be caused by various factors and stimuli. The same patient may have a seizure one or more times over a certain period of time. In this case, the nature of convulsive attacks may change.
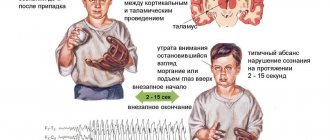
Figure 1. Common symptoms of epilepsy. Image: Natty_Blissful / Depositphotos
Despite this variability of clinical manifestations, doctors identify 4 characteristic features of epileptic seizures:
- They start suddenly. A person does not know when he will have another attack. This is a serious psychological factor, due to which the patient is in constant tension and expects that a seizure will happen to him. Some patients experience an aura before an epileptic seizure. These are specific sensations, such as emotional feelings or smells, that indicate an impending attack.
- The attacks do not last long. Lasts from a few seconds to several minutes. Some patients do not notice the attack at all. For example, they may freeze or experience some unusual sensation. Some fall, losing consciousness. Sometimes attacks follow one after another.
- The attack may go away on its own. As a rule, this is what happens. During a seizure, no medical intervention is needed to stop it. The exception is status epilepticus, when the patient experiences a series of incessant seizures.
- The attacks have a stereotypical character. If a patient has a certain type of attack, then, as a rule, future attacks will be the same. In some cases, the nature of the attacks changes over a long period. However, over a short period of time, the attacks are almost identical.
Safety precautions for people with epilepsy
Following these simple rules will help you avoid serious complications:
- Don't cook food alone. If you are alone at home, buy ready-made food. Also, refrain from using tools and household appliances if no one is around.
- Instead of a stove, use a microwave oven.
- Take a shower instead of a bath. Bathtub drowning is one of the most common causes of death in people with epilepsy.
- Lay a rubber mat in the bathroom.
- Cover hard corners of tables, chairs and other furniture. This is especially true for objects that are lower than you (that you could potentially fall on during an attack).
- Move the bed away from walls and furniture.
- Use seizure alarms. These are various gadgets for epileptics (bracelets, watches or devices that are attached to the head), which notify the victim’s loved ones or a doctor about an attack.
Epileptic seizures are different:
- long-term;
- random – occur without a provoking stimulus;
- cyclical – appear periodically;
- provoked - arise in response to the action of some factor;
- with or without convulsions.
According to clinical manifestations, seizures are generalized and partial. Generalized ones include:
- Tonic-clonic. This is the most common type of generalized seizure. The man suddenly loses consciousness and falls. His body arches due to tonic muscle tension. Tonic-clonic seizures are characterized by short-term holding of breath and muscle twitching (clonic convulsions). Some patients experience involuntary urination and bowel movements. Typically, tonic-clonic seizures last no more than 5 minutes.
- Clonic. They are rare. Manifested by repeated muscle twitching.
- Tonic. This is a sudden attack-like muscle tension. The patient's eyes roll back and it becomes difficult for him to breathe. If an attack occurs in a standing position, the person falls, which may be accompanied by injuries.
- Atonic. During such attacks the patient does not have convulsions. He loses consciousness, and his muscles lose tone. Atonic attacks are characterized by rapid recovery.
- Absence seizures. These seizures most often occur in children. The child freezes for a few seconds. Sometimes some movements may occur during a seizure.
- Atypical absence seizures. Seizures begin and fade gradually. They are characterized by head nodding, body bending and falling. Sometimes the muscles twitch slightly.
- Myoclonic. These are attacks with short, non-rhythmic muscle twitching.
Figure 2. First aid for an epileptic attack.
Image: leremy / Depositphotos Partial seizures can also occur in different ways. It all depends on in which area of the brain epileptic activity is observed. For this reason, such attacks are also called focal or local. They are often accompanied by impaired coordination of movement, loss of orientation, frequent mood swings, impaired cognitive functions and sensory organs.
Some patients experience seizures that do not meet the criteria described above. These are unclassified epileptic seizures. For example, a person suddenly begins to move his eyes rhythmically or make intense chewing movements with his jaws.
Seizures are not always a symptom of epilepsy. In some children they occur in response to hyperthermia (increased body temperature), in pregnant women diagnosed with eclampsia - in connection with increased blood pressure. Convulsions can appear after binge drinking during alcohol withdrawal syndrome and with various types of shock.
Keto diet for epilepsy
Even before the advent of antiepileptic drugs, the mainstay of treatment for epilepsy was the ketogenic diet.
It began to be used in the 20s of the last century, when it was noticed that when carbohydrates were limited, patients with epilepsy were less likely to experience seizures. The ketogenic diet is a diet with a predominance of fatty foods. On such a diet, you can eat eggs, fatty meats, fish, avocados, butter and vegetable oil. Protein and leafy vegetables are also allowed. But you need to give up sugar, flour products, potatoes and other carbohydrate foods.
When you sharply reduce your carbohydrate intake, ketosis starts within 2-3 days. The body switches to another fuel - fats, the oxidation of which produces ketones. The latter are then used as fuel, including by brain cells.
There are several types of ketones, including beta-hydroxybutyrate and acetoacetate. They are known to have anticonvulsant effects. The positive effect of the keto diet is associated with this property of ketones. However, the exact mechanism of the therapeutic effect of the keto diet for epilepsy is not yet completely clear.
There are over 50 million people in the world with epilepsy. Some people got the disease as a hereditary factor, some became its owner due to a head injury, and others developed the disease due to a tumor formed in the brain. Today there are communities of epileptics who communicate in reality and via the Internet. Among the sick people there are many bright and extraordinary personalities. Anyone can find help and support. Tips, recommendations, stories of successful treatment - all this ceases to be a sealed secret! Look for useful information on our website and be sure that the fight against epilepsy gives excellent results!
Description of epilepsy - signs of manifestation of the disease
Children and adolescents most often suffer from epilepsy. It is believed that the disease occurs in 1% of people under the age of 18 years from the total population of this age group. Epilepsy occurs in adults and older people. However, in this case, it more often acts as a complication after strokes, injuries and other vascular pathologies. In Russia, the development of epilepsy is progressing at a pace similar to the world level.
When most of us hear about the disease, we imagine a fallen person convulsing. Foam appears at the mouth, he makes inarticulate sounds, and, tired from the attack that has been ongoing for a long time, he falls silent and slowly falls asleep, exhausted. This is a classic manifestation of epilepsy, medically called a generalized tonic-clinical seizure. Often the disease is accompanied by other symptoms, including loss of consciousness, inappropriate reactions to others, and withdrawal.
The attack time can be minimal and take only a few seconds. Doctors say that this condition is often invisible from the outside; it can be mistaken for absent-mindedness or inattentiveness. However, if such symptoms tend to recur with a certain frequency, loved ones notice alarming phenomena and consult a doctor. In medicine, these cases are called absence seizures.
During an absence seizure, you will not notice the patient convulsing, but will only see a person falling out of reality for no more than 30 seconds. He will not react to the people around him, show attention to them, or be distracted by questions and extraneous irritants. At this time, he seems to be given to himself and is alone with his own thoughts. It is important to pay attention to the manifestation of this behavior in time, since in the future the frequency of these attacks increases. They can occur up to several dozen times a day, which frightens others.
Children also experience nocturnal attacks, which are not similar to a traditional epilepsy attack. During sleep, a child tends to take unusual positions, in which increased tension in certain parts of the body clearly appears. You can notice how the mouth twists, how the awakened baby tries to say something, but cannot do it due to the tension spasms that arise. It is important not to make the mistake that disturbances of consciousness are related to epileptic seizures. In the case of epilepsy, seizures always occur spontaneously, without a specific cause. It is difficult to predict their appearance, since in most cases they appear out of nowhere.
Causes of epilepsy - where does the attack come from?
WHO groups the causes of the disease into several main forms, including:
- Ideopathic form - the disease is genetic in nature and is inherited, sometimes after several dozen generations, which does not make it possible to immediately identify the root cause of the disease. In this form, there is no organic brain damage, but a specific reaction of neurons to external stimuli is observed. The course of the attacks is unstable, seizures occur for no reason.
- Symptomatic form - trauma, tumors, intoxication of the body, and developmental defects have a significant impact on the development of the disease. The attack has a sudden onset and can be caused by even the slightest irritant from the outside (injection, insult, severe frustration).
- The cryptogenic form - the cause of the manifestation of pulsed foci has not been precisely identified.
Why does the disease occur? What are the causes of epilepsy that cause terrible seizures? It is believed that there are a great many forms of the disease and the causes that cause it. The cause may be a difficult pregnancy, pathological childbirth, mechanical injuries to the pregnant woman and the baby. In these cases, epilepsy occurs early and manifests itself in the first or second years of a child’s life.
Despite the long period of study of the disease, there is no certainty that epilepsy in most cases occurs due to the presence of a genetic predisposition. According to statistics, 40% of epileptics have a history of relatives with a similar illness, but this does not give the right to say that unfavorable heredity is always passed on from generation to generation. Among the most common causes of the disease are:
- history of traumatic brain injury;
- diseases of parasitic or viral origin that give complications in the form of epileptic seizures;
- insufficient blood supply to the brain and resulting oxygen starvation;
- emerging tumors, abscesses and formations of unknown etiology in various parts of the brain.
Medicine is unable to determine the exact causes of epilepsy in 70% of cases. However, specially organized studies have shown that the sensitivity of brain tissue in people with epilepsy is several times higher than in healthy people to the same stimuli. If a healthy person does not notice the influence of a certain signal from the outside, then the patient’s response is an epileptic seizure.
By nature, an attack is the result of synchronous excitation of brain neurons. Nerve cells of a certain area of the cortex are excited - the so-called epileptogenic focus, which gives a reaction. The causes may be meningitis, stroke, alcoholism, drug addiction, multiple sclerosis. It has been proven that every 10th alcoholic is susceptible to epileptic seizures. Another interesting trend is that more than 60% of people suffering from epilepsy experienced their first attack of the disease before the age of 18 years.
It is easy for a person unfamiliar with the problem to confuse hysteria with epilepsy. The seizures are similar in many ways, but have clear differences. A hysterical attack is a consequence of a strong stress-generating effect on the psyche. It occurs as a response to frustration, severe resentment, grief, and can be a consequence of fear or other experiences. Typically, hysteria occurs in the presence of other people, it can last from 15 minutes to a couple of hours, and may be accompanied by convulsive body movements.
A person in this state screams, falls, and performs spectacular actions in public. But if you look closely, he does not seek to harm himself with careless movements, does not try to cause serious damage and is in a state of consciousness. Having woken up from hysteria, a person does not experience the stupor and drowsiness characteristic of epilepsy. He quickly comes to his senses and begins to control his own behavior.
In cases of mild epilepsy, a seizure may appear as a brief loss of connection with the outside world. The patient's eyelids twitch slightly, his face trembles convulsively, and there is a slight pulsation of the muscles. From the outside, this state looks like absorption in one’s own thoughts or deep thoughtfulness. People around you may not even notice the attack. Moreover, a seizure may go unnoticed by the patient.
A distinctive feature that signifies the approach of an attack is the presence of an aura - a special reaction of the body. Warning symptoms may include fever, dizziness, unreasonable anxiety and fussiness. During an attack, the patient does not understand anything, does not feel pain or discomfort. The attack lasts several minutes, so it often goes unnoticed by others.
Benign and malignant epilepsy
The disease epilepsy is divided into benign and catastrophic (pathological) forms. The first is characterized by rare attacks that do not have a detrimental effect on personality development. It is recognized that this form of the disease can go away on its own without specialized treatment or medical intervention. However, this type of disease is typical exclusively for children.
Catastrophic forms of epilepsy have another name - epileptic encephalopathies. The disease is also observed only in childhood, but unlike benign epilepsy, it is very severe and is accompanied by disturbances in speech and neuropsychic functions. The disease has a significant impact on personality development and can cause mental illness.
Living with epilepsy - the struggle for health
To neutralize the manifestations of epilepsy, doctors prescribe medications that differ in strength and intensity of action, depending on the general clinical picture of the disease. Their use is lengthy and requires great responsibility from the patient. It is strictly forbidden to skip taking medications recommended by your doctor. Even a benign form of epilepsy can be treated for several years before its symptoms subside.
In the case of a complex form of the disease, medications have been taken for decades. It is not always possible to cure a harmful condition, but you can achieve control over it, which greatly simplifies life and improves its quality. For the patient, the absence of seizures is an opportunity to live a full life. A person with epilepsy, in the absence of sudden attacks and fits, can play sports, have various hobbies, travel the world, learn the traditions of different countries and cultures. Physical and intellectual stress, as well as emotional stress, rarely become triggers for an attack. Therefore, you should not significantly limit yourself if the course of the disease is favorable.
Abroad, people with epilepsy who have not had seizures for a long time are given a driver's license and a permit to drive a vehicle just like everyone else. However, after getting rid of seizures for a long time, you should be careful about your health. It is required to maintain a balanced regime of sleep and wakefulness, rest and exercise. You should absolutely not drink alcohol. You should choose your activity with caution, trying to avoid extreme activities. Although the likelihood of an attack can be reduced with the help of medications, the risk of its reoccurrence in the future cannot be ruled out.
Pregnancy and epilepsy - a factor of caution
The period of gestation is a particularly important time in the life of every woman. Therefore, great attention must be paid to all possible risk factors that could pose a threat to the mother and the child developing in the womb. If a pregnant woman suffered from epilepsy as a child, which subsequently went away, there is no reason to worry about the safety of the child. The situation is different when the conversation turns to a future mother suffering from an illness during pregnancy. She must be monitored by an epileptologist. Pregnant women suffering from epilepsy are monitored in accordance with the standards of the International League Against the Disease.
It is believed that taking medications prescribed by a doctor and strictly following the recommendations of a specialist provide a 95% guarantee that a healthy child will be born, and the birth process will not cause a negative reaction from the body. Moreover, there is a well-known opinion of professional doctors who claim that pregnancy in some situations can soften the course of epilepsy and make seizures less common.
Perception of a patient with epilepsy in society
Russian society has not yet become accustomed to the normal perception of sick people on the streets, in schools, in state companies and commercial structures. Therefore, a sudden epileptic attack in full view of passers-by can become a serious psychological trauma for a sick person. Most people suffering from an illness try to hide their own illness, keep silent about it, and not make it known to colleagues at work, housemates, or business partners. Unfortunately, epilepsy is perceived as some kind of shameful stigma, inferiority, inferiority. What can we say about ordinary people, when even some doctors believe that the disease in any of its manifestations has a serious impact on the patient’s level of intelligence, disrupting and deforming it. In reality, everything is different.
The majority of patients with epilepsy do not have any mental disorders or personality disorders. These are ordinary people, among whom there are quite a few professionals in one industry or another. The more offensive is the cruelty of others who refuse to admit an epileptic to kindergarten, school, or work.
Since ancient times, little has changed in the everyday perception of epileptics, when they were spoken of as people endowed with demonic powers. It was believed that they were capable of infecting by simply touching or inhaling the same air in a room with healthy people. However, not everyone shared this point of view. There is another opinion, according to which epilepsy is a disease of the elite. Napoleon, Gaius Julius Caesar, and Alexander the Great suffered from it. These great personalities made history, conquered continents and cities, and shaped destinies.
Comparing the level of social support for sick patients abroad and in Russia, it should be noted that in our country there is no legislative framework defending the rights of epileptics. Abroad, the presence of public organizations that lobby for the interests of patients is considered normal. Active information work is carried out with them, within the framework of which specialists explain the rights, interests and characteristics of the lives of these people. In European countries, epileptics are not perceived by society as outcasts; they are not labeled as inferior.
Symptoms of epilepsy - learning to distinguish an attack
The disease may look different in different forms of the disease. This depends on the manifestation of a pathological discharge in a specific area of the brain. The consequence of its influence can be speech disorders, failure in coordination of movements, changes in muscle tone (increase and decrease in muscle tension), and mental deviations from the norm. Symptoms can manifest themselves either in individual reactions or in their complex. Let's look at several types of epilepsy in more detail to study the symptoms of the disease.
Jacksonian attacks - since a clearly localized area of the brain is irritated, the symptoms are specific in nature and affect a specific muscle group. A sudden psychomotor disorder is short-lived and usually lasts a few minutes. The patient experiences confusion and loss of contact with people around him. He does not realize that he has suffered an epileptic attack, so he refuses help offered from outside. Mild cramps or slight numbness begin to appear in the extremities - hands, legs, feet. If the spasms spread throughout the body or involve a large part of it, a generalized or grand mal seizure occurs, which is characterized by:
- Precursors in the form of a state of anxiety and restlessness that arise several hours before the onset of an attack. The patient's nervous excitement is increasing.
- Tonic convulsions, when the patient's head is thrown back, the muscles of the body tense, the body is stretched into a kind of arc, reminiscent of a bow in shape. Stopped breathing blocks the access of oxygen to the lungs, and the patient’s face takes on a bluish tint. The phase lasts no more than 30 seconds, in rare cases reaching a minute.
- Clonic convulsions, in which there is a rhythmic contraction of the muscles of the body. Salivation increases and foam comes out of the mouth. The phase lasts no more than 5 minutes, after which the cramps go away. Breathing is restored, swelling in the face and the swelling caused by lack of oxygen disappears, and the bluishness of the skin disappears.
- Stopper - a sharp relaxation of the muscle corset, possible involuntary discharge of urine and feces. The patient may lose consciousness and faint. The duration of the phase reaches half an hour. There are no reflexes at this time.
- Dream.
After a seizure, the patient may experience headaches and dizziness for several days. At this time, muscle weakness is typical.
Minor attacks have a milder manifestation. During their course, there is a twitching of the facial muscles, a sharp relaxation or, on the contrary, a toning of the muscular corset of the body. Consciousness is not lost, absence is possible. The patient may roll his eyes and freeze for a short time. These attacks most often occur in preschool age. After their completion, patients cannot remember what happened recently.
Status epilepticus is the most terrible condition in which immediate medical attention is required due to increasing brain hypoxia. The sequential manifestation of a whole series of attacks is accompanied by a lack of consciousness, decreased muscle tone, and the absence of reflex manifestations of the body.
It should be noted that any epileptic seizures begin spontaneously and also end suddenly.
What examinations need to be completed
Before diagnosing the disease, the doctor examines the patient, fills out his health card, and identifies risk factors associated with a history of relatives with epilepsy. Systemic and chronic diseases of the patient are identified, the symptoms of the attacks that appear are checked and carefully studied. The frequency of seizures, their strength, intensity and duration are studied. To do this, the patient himself and people close to him are interviewed. This helps to reconstruct the picture in detail, since in most cases the patient does not remember what happened to him. In addition to the specified set of measures, the epileptologist refers the patient to electroencephalography, which results in a pulse recording of brain activity and neuron activity. Computed tomography and magnetic resonance imaging may also be used.
Prognosis map of the disease
Provided that epilepsy was detected in a timely manner and received proper treatment, life without seizures is observed in 80% of cases. These people are active, social, fully developed. Many of them adhere to drug therapy for the disease throughout their lives according to the schedule recommended by the doctor. They take special medications, neutralizing the possibility of attacks. The list of drugs, as well as the dosage of the drugs, are determined by the attending physician depending on the form and nature of the disease. Patients with generalized tonic-clonic seizures need constant care and monitoring from close relatives, since if a seizure develops, there is a high probability of death under unfavorable circumstances.
Treatment of epilepsy - stages of therapy
Stable remission is achieved in 80% of cases of epilepsy treatment. About 35% manage to get rid of the disease for good with the support of doctors and close relatives. Upon initial diagnosis, a timely course of drug therapy helps to suppress seizures for several years to come or neutralize the disease completely in most cases.
The content of the therapeutic course depends on the form of the disease, the symptoms that appear, the age of the patient and his general state of health. Epilepsy is treated with conservative methods or surgical intervention. Doctors most often try to avoid the second method, since with proper prescription of medications and their timely administration, they can achieve successful results in 90% of cases. Drug treatment is based on compliance with the main stages of therapy:
- Diagnosis of epilepsy with determination of the type and form of the disease for the competent selection of an effective drug.
- Identifying the root causes of the disease. If a symptomatic form of the disease manifests itself, a detailed examination of the brain is carried out, aneurysms, malignant tumors, and benign neoplasms are identified.
- Development of a schedule of measures to eliminate risk factors to prevent the development of attacks. It is necessary to eliminate stress factors, minimize situations of mental and physical fatigue, drinking alcoholic beverages, hypothermia and overheating of the body.
- Relief of attacks by providing immediate assistance, taking anticonvulsants and other medications prescribed by a doctor.
The main task of the attending physician is to inform relatives caring for the patient about the correct behavior during periods of convulsions and epileptic attacks. Timely assistance will help protect the patient from injury and prevent death where it can be avoided.
Omega-3 treats epilepsy and reduces seizures
This is evidenced by data from a study conducted by the University of California, USA. The sample consisted of 24 people with epilepsy and prone to seizures. The result of the experiment showed that Omega-3 acids consumed daily in food help reduce the occurrence of epileptic seizures by up to 36%. The intake of useful substances into the body occurred thanks to fish oil capsules. The study lasted for 2.5 months. In addition to reducing the symptoms of epilepsy and reducing the excitability of brain cells, patients experienced normalization of blood pressure in the body.
You can take Omega-3 not only in capsule form. Eating fatty varieties of sea fish helps the body receive useful elements. These include Atlantic herring, mackerel, sardines, trout, tuna, and salmon. All kinds of dietary supplements based on the use of Omega-3 in their composition have proven themselves well.
The catogenic diet for epileptics works wonders
Doctors agree that the catogenic diet allows epileptics to improve their quality of life by softening the manifestation of seizures and making them more rare. The technique is prohibited for children under one year of age. Since food consumption follows strictly regulated standards, only a doctor can prescribe a diet after a complete examination of the patient’s clinical picture.
Long-term dietary restriction can reduce the frequency of seizures. There are cases where, after using the catogenic diet, the symptoms of eilepsy completely disappeared. However, the aggressive nature of the diet is not for everyone. The doctor must carefully monitor the patient’s condition and be sensitive to any changes in well-being. The essence of the diet is fasting. In the first three days, the patient is asked to take exclusively plain water without gases. During this period, physical activity is reduced and bed rest may be maintained.
Starting from the fourth day, the patient gradually introduces solid foods into his diet, which include chicken breast, eggs, sausages, and cottage cheese. Fasting is prohibited on these days. You need to eat in small portions, at least 5-6 times a day. Products are carefully calculated. As a result, on the “edible” days of the week you should get a menu with the following proportions: 4 shares of fats/1 share of proteins/1 share of carbohydrates. You should not eat potatoes, beets, cereals, bread, pasta, or carrots.
For children with epilepsy from one to 12 years of age, the catogenic diet is transformed. Nutritionists include milkshakes prepared according to a special recipe in the diet. The main goal of the diet is to teach patients to eat foods rich in fat. Fats have antiepileptic properties, so they help the body fight the disease more effectively.
During the catogenic diet, it is allowed to eat fermented milk and dairy products, lean turkey and chicken meat, sea fish, eggs, fatty cottage cheese, vegetables, tea and coffee with cream. It is recommended to drink a lot of water to remove toxins and decay products. On the Internet you can find many recipes for the catogenic diet, which will make it more interesting and original.
Traditional medicine recipes in the fight against epilepsy
Folk wisdom offers its own means of combating epileptic seizures. However, a passion for prescriptions can be destructive if you do not coordinate them with your doctor or neglect traditional medicinal medicine. Among the most popular folk remedies are:
Stone oil , rich in vitamins, minerals and trace elements. It has pronounced antispasmodic and immunomodulatory properties. The most widely used is the “Siberian” recipe for combating the disease. According to it, 3 grams of oil are diluted in 2 liters of water. The solution is taken before meals for a month three times a day, no more than once a year in full course.
Herbal powder , for the preparation of which equal parts of dried peony, licorice and duckweed are taken. You can grind the raw materials using a blender, mortar or coffee grinder. The drug is taken in half a teaspoon along with a diphenine tablet three times a day for up to 2 weeks, followed by a week break and a repetition of the two-week schedule. A total of three courses are recommended. Since the product contains a drug, it is worth getting a doctor's recommendation to take it.
Maryin root is used in the form of an alcoholic tincture of the petals. The tincture has a beneficial effect on neurasthenia, paralysis, and epilepsy. Infuse 3 tablespoons of the solution in a bottle of vodka for a month. Take a teaspoon with meals three times a day.
On the Internet you can find many recipes that treat epilepsy and neutralize seizures. According to naturopathic doctors, herbs such as Blue cyanosis, Hogweed, Shiksha, Chernobyl, Oregano, Drupe, St. John's wort and Meadowsweet help well. However, it is better to select herbs together with your doctor on an individual basis. Incorrectly prescribed therapy can delay the time needed to correct epilepsy and have a detrimental effect on the general condition of the body.
Herbalists say that medicinal plants can give good results, but they need to be used for a long time. The cumulative effect of the positive effects of herbal components promotes long-term use. Sometimes homeopathic treatment lasts several years.
In addition to herbs, manual techniques for treating epilepsy are also known, which came to us from recipes of folk wisdom. During an attack, it is recommended to press the epileptic’s left hand to the floor, while simultaneously stepping on the patient’s left little toe. This is easy to do when the patient is in a supine position during an attack. In addition to these recipes, there are techniques based on smell. It is recommended to constantly place myrrh resin in the epileptic’s room, which can be bought in the church. Priests used this miraculous substance to heal in ancient times. Resin calms the nervous system, has a beneficial effect on mood and harmonizes the emotional background.
Drug therapy for epilepsy - mandatory compliance with conditions
Taking medications in strict accordance with the dosage and schedule allows you to bring epilepsy attacks under control. Skipping pills and lack of consistency in treatment create significant risks for the occurrence of epileptic seizures. During conservative treatment, the following conditions must be observed:
- Follow the medication schedule and exact dosage recommended by your doctor;
- Avoid self-medication and the use of any medications without the consent of your doctor. If your friends recommended the drug or the pharmacist at the pharmacy praised the new drug, discuss the possibility of taking it with the specialist treating you;
- Therapy should not be stopped when lasting results have been achieved. An independent decision to discontinue the drug can provoke an attack. Only an epileptologist or neurologist can cancel the appointment.
The patient is obliged to notify the doctor supervising the treatment about the manifestation of non-standard reactions of the body to external or internal stimuli. If previously unusual symptoms appear, you should notify your doctor immediately.
The majority of people with epilepsy successfully cope with seizures by taking medications prescribed by a doctor. A correctly selected drug and its proper dosage can stop the development of the disease for many years, forcing the patient to forget about previously manifested attacks. According to standard practice, the doctor initially prescribes a minimal dose of an antiepileptic drug and then monitors the patient. If it is impossible to prevent attacks with small doses, the dosage is increased. As soon as stable remission occurs, the successfully selected dosage is fixed in the patient’s medication schedule.
Prescribed medications include carboxamides, valproates, phenytoins, and phenobarbital. Wherein
Treatment of epilepsy
Drug, non-drug and surgical methods are used to treat epilepsy. In most cases, the result is achieved with the help of antiepileptic drug therapy. The basis of such treatment is anticonvulsant drugs. These are anticonvulsant drugs of various pharmacological groups, in particular, drugs based on carbamazepine and benzonal.
Recently, drugs containing valproic acid (valproate) have been used to treat epilepsy. Such drugs, in addition to their anticonvulsant effect, also protect nerve cells from damage and improve their metabolism. This is especially important for patients with epilepsy with concomitant mental disorders.
Electrical stimulation of the vagus nerve
If drug treatment does not bring the desired results, doctors use other options. One of these is VNS therapy or electrical stimulation of the vagus nerve.
The essence of this treatment comes down to the subcutaneous implantation of a neurostimulator, which constantly sends impulses to the vagus nerve. The latter is an important link between the body and the brain. Such stimulation of the vagus nerve in most cases leads to a decrease in pathological electrical activity in epileptic foci. The patient's frequency of seizures decreases.
Surgical treatment of epilepsy
If it is determined that the cause of epilepsy is a tumor, cyst or vascular pathology of the brain, the problem is often solved surgically. After the operation, the patient's condition stabilizes. Sometimes the epileptogenic focus is also removed (if this is permissible).
Generalized epilepsy and sleep
Seizures during sleep are characteristic of idiopathic generalized epilepsy. This connection is explained by damage to thalamocortical structures.
In idiopathic generalized epilepsy, sleep deprivation stimulates epiactivity and increases the likelihood of an epileptic seizure.
Attacks more often occur when falling asleep or waking up, especially with early forced awakening.
Thus, in the first 15 minutes - 1 hour after getting up, patients with juvenile myoclonic epilepsy experience epileptic seizures: myoclonus (usually in the form of twitching in the hands) or, especially with ineffective therapy, generalized tonic-clonic seizures.
In epileptic encephalopathies with electrical status of slow-wave sleep (ESES), even from the name it is clear that the manifestations of the disease are associated with sleep. A feature of these forms of epilepsy is the presence of continued epileptiform activity with a high epiactivity index (more than 80%) during the slow-wave sleep phase. And during the rapid eye movement sleep phase, the epiactivity index decreases.
Nocturnal seizures in epileptic encephalopathies with electrical status of slow-wave sleep can be in the form of: focal motor seizures during sleep, generalized tonic-clonic seizures. Daytime attacks, both focal and generalized, are also possible.
Symptomatic secondary generalized epilepsy is less dependent on sleep-wake cycles. With this form of epilepsy, epileptiform activity and seizures can occur at any time of the day with equal probability.
Prognosis and prevention
Each patient's disease progresses differently. The prognosis for epilepsy depends on a number of factors, including:
- type of epilepsy;
- age at onset of disease;
- frequency of epileptic seizures;
- severity of concomitant mental disorders;
- the body's reaction to the therapy used;
- other factors.
Specific prevention for epilepsy has not been developed. The risk of developing the disease can be minimized by eliminating the factors of acquired epilepsy. This includes timely treatment and prevention of infections, avoiding brain injuries and a healthy lifestyle. Sports, proper nutrition, and the absence of bad habits (including avoiding alcohol) reduce the risk of developing neurological disorders in old age (this is also true for epilepsy).
Epilepsy and pregnancy
Epileptic seizures during pregnancy are fraught with serious consequences for both mother and fetus.
The risk of miscarriage, birth injuries, or intrauterine developmental disorders increases significantly. However, this does not mean that pregnancy is contraindicated for women with epilepsy. It is better to prepare for it under the supervision of an experienced doctor. Conception should be planned against the background of stable remission, when there are no symptoms of epilepsy for 1-2 years.
During the first trimester of pregnancy, your doctor will advise you to take folic acid. This is necessary to reduce the risk of abnormal fetal development.
Pregnant women with a history of epilepsy should regularly undergo tests prescribed by their doctor and monitor their condition.
If it is difficult for a woman with epilepsy to achieve stable remission, then conception is undesirable.
When to see a doctor
To prevent further development of the disease, it is necessary to consult a doctor immediately after the first attack or the appearance of indirect symptoms of epilepsy. The sooner the diagnosis is made and treatment is started, the more favorable the prognosis for recovery will be.
With such a disease, you need to contact a pediatric neurologist. At JSC “Medicine” (clinic of Academician Roitberg), located in the center of Moscow, experienced specialists conduct appointments. The clinic is equipped with all the necessary equipment for correct and accurate diagnosis of diseases. A detailed account of how the attacks progress will be a huge help in making a diagnosis. Even more helpful is a video that one of the parents can take during the seizure.
Causes of epilepsy
The causes of epilepsy still remain unclear. Researchers consider the hereditary component of the disease as fundamental. According to statistics, 40% of people with epilepsy have blood relatives with a history of the same disease. But at the same time, epilepsy cannot be classified as a hereditary disease. Even if both parents suffer from this disease, this does not mean that their child will also suffer from it. You can inherit from your parents the specific structure of the brain and nerve cells, as well as the degree of their sensitivity to external stimuli. These features make a person more or less prone to epilepsy.
It has been established that epilepsy in both parents increases the likelihood of the child becoming ill by 10-12%. If one of the parents is sick, the risk is halved. The likelihood of inheriting the disease also depends on the degree of its severity in the parents. The more severe the disease, the higher the risk of passing it on by inheritance.
If a child has inherited from his parents a special brain structure that is prone to abnormal electrical activity, then the disease may not manifest itself for a long time (or may not make itself felt at all). However, there are factors that contribute to the occurrence of epilepsy, even without a hereditary component. These include:
- Brain injuries. In approximately 10% of cases, brain contusions provoke the appearance of epileptic seizures in children and adults. Most often, such injuries occur in road accidents, falls or sports (for example, boxing). If the injury causes the victim to lose consciousness, then the likelihood of an epileptic complication is higher.
- Infections. The danger comes from toxins produced by microbes. They disrupt trophic processes in brain tissue, promoting changes in the electrical activity of neurons.
- Circulatory disorders. Most often these are age-related changes associated with loss of vascular elasticity. Thus, the supply of nutrients and oxygen to the brain is disrupted. This leads to metabolic changes, and sometimes to an imbalance between the inhibitory and excitatory systems.
- Metabolic disorders. As a rule, these are pathological changes that occur against the background of hormonal imbalance.
- Anomalies of brain development. Sometimes congenital abnormalities in the structure of the brain or blood vessels (for example, arteriovenous malformation) become a trigger for the occurrence of epileptic attacks.
- Brain tumors. Epilepsy in adults and children often occurs against the background of an intracerebral tumor. The larger the size of the tumor, the higher the risk of epileptic seizures. As a rule, after the tumor is removed, the symptoms of epilepsy disappear.
- Action of toxins. Alcohol, drugs, heavy metals and some medications have a toxic effect on nerve cells. Against the background of intoxication, entire groups of neurons may not function properly.
It is important to understand that the factors described above almost never cause epilepsy on their own. The common factor in this case is organic damage to the brain, in which a focus of epileptic activity is formed.
An epileptic focus is a group of neurons with unstable cell membranes. They are prone to spontaneous electrical excitation, which leads to a seizure.
Electroencephalogram of an epileptic seizure. Photo: Neuroscience Journal / Open-i
Prevention
The prevention of seizures plays a special role in getting rid of the disease. However, even if the attacks disappeared from a person’s life a year ago, the foci that caused them do not disappear. Therefore, a diagnosis made in childhood, overcome by painstaking treatment or due to age, can return. In adulthood, with much more serious symptoms.
To reduce the likelihood of this happening, you need to remember throughout your life that your body is prone to seizures. And carry out preventive measures:
- adhere to a clear daily routine;
- avoid discos and computer games;
- choose sports activities allowed for such a diagnosis;
- avoid overwork;
- do not drink alcohol;
- follow a diet;
- avoid taking drugs;
- warn doctors about a previously made diagnosis when choosing medications;
- approach the issue of driving with caution;
- choose a profession taking into account instability to severe stress and overwork; there are jobs that are contraindicated for epileptics;
- closely monitor your health, as some diseases can provoke repeated attacks in adulthood;
- regularly practice courses of selected physiotherapy.
Even if there were no attacks after reaching puberty, and the diagnosis was eventually removed, you cannot forget about the structural features of your brain. Whether it is possible to cure epilepsy in a child forever is an open question due to the specifics of the disease.
Types of epilepsy
Let's look at the main types of epilepsy based on the classification described above so that you understand what you are dealing with.
Generalized epilepsy
This is a type of epilepsy in which almost the entire brain is engulfed in increased electrical activity. The causes of generalized epilepsy are unclear, which is why it is called idiopathic. It is believed that this pathology has a genetic component. In this sense, genetic and idiopathic generalized epilepsy are synonymous.
Focal epilepsy
In focal epilepsy, pathological electrical discharges occur only in a certain area of the brain. If there is only one epileptic focus, then such epilepsy is called unifocal; if there are several foci - multifocal. In rare cases, pathological activity affects the cerebral hemisphere. This is hemispheric focal epilepsy.
Combined epilepsy
Some patients experience seizures characteristic of both generalized and focal types of epilepsy.
Unknown epilepsy
Unknown or unspecified refers to epilepsy for which it is impossible to determine the type of seizure (focal, generalized or combined).
Epileptic syndromes
The next level of classification of epilepsy is the definition of the syndrome by which the disease can be expressed. Currently, dozens of different epileptic syndromes have been described in children, adolescents and adults. Many of them bear the names of their discoverers, for example, Ohtahara, West, Dravet, Lennox-Gastaut syndromes and others.
Figure 3. Ketogenic diet recommended for epilepsy. Image: macrovector/freepik.com
Etiological criterion
Based on etiology, the following types of epilepsy are distinguished:
- Genetic. It occurs due to genetic, chromosomal abnormalities or other features of the human genome. However, genetic etiology does not mean that the disease is inherited.
- Structural. These are epilepsies caused by structural abnormalities of the brain. Such features may be congenital or acquired (for example, after injury, infection or poisoning).
- Metabolic. In this case, epilepsy develops due to disturbances in creatinine, cerebral folic acid, mitochondrial disorders, deficiency of certain enzymes and other metabolic disorders.
- Immune. Against the background of some immune (and autoimmune) disorders, parts of the central nervous system become inflamed. This increases the risk of developing epilepsy.
- Infectious. One of the most common etiologies of epilepsy, especially in developing countries. A variety of pathogenic pathogens infect the nervous system, causing both acute and epileptic seizures. Such infections include bacterial meningitis, viral encephalitis, cytomegalovirus, cerebral toxoplasmosis, HIV and others.
- Unknown. Unspecified etiology is said to exist when the underlying cause cannot be determined.
Psychological discomfort in epilepsy
Another complication of epilepsy can be considered psychological discomfort. The person realizes that he could have a seizure at any second. Sometimes such attacks are accompanied by foaming at the mouth, urination and defecation. At such moments, it is extremely important that the people around you treat this with understanding.
Epilepsy: first aid
In the event that you become an involuntary witness to an epileptic attack of your relative, good friend or just a stranger from the outside, you need to do the following:
Throw panic aside and come to your senses, because you must not forget that now the life of another person completely belongs to you and only you can help him. Call emergency services immediately.
While the attack lasts, be sure to stay close to the patient and under no circumstances leave him.
Take a look at everything that is around. Is there any threat around you? Once you are sure that everything is fine, do not touch the person, much less move him. It is best to eliminate nearby objects in the form of furniture, sharp or piercing objects that may accidentally cause harm or pain.
As a matter of urgency, turn on the timer or read the time out loud from the second the epileptic attack occurred.
If the person is standing, you should carefully lower his body to the ground and place any soft object (jacket, hat, empty backpack, etc.) under his head.
Under no circumstances should you try to forcibly restrain a person in a constrained state in order to supposedly prevent a convulsive state. This will not help relax the muscles, but it can cause serious injuries.
Do not open or put anything in the sick person's mouth. It would also be unnecessary to try to unclench his jaw during an attack.
The last thing is to check again whether the timer is set.
After everything is over, provide moral support and, if possible, calm the person down. Your speech should not be rude or sound like a quick set of phrases.
Diagnosis of epilepsy
Existing diagnostic methods make it possible to establish an accurate diagnosis, as well as distinguish epilepsy from other disorders with similar symptoms. First of all, these are the following instrumental studies:
- Electroencephalography (EEG) is the main diagnostic method for epilepsy. Patients with epilepsy are known to have abnormalities in their brain wave patterns. These changes can be recorded even in the absence of seizures. As a rule, EEG video monitoring is initially performed at night. This allows us to determine the cause of epileptic seizures. Then regular EEGs are done once every six months4.
- High-resolution computed tomography and magnetic resonance imaging (CT and MRI) of the brain allow one to evaluate the structural features of the brain, the presence of cysts, tumors, vascular and other disorders.
To assess the effectiveness of treatment, the patient needs to donate blood every 3 months. The test will also help assess the risk of certain side effects of antiepileptic drugs.
How to make an appointment with a neurologist
To make an appointment with a neurologist at a time convenient for you, use the online form or call the clinic’s contact number. Children experiencing epilepsy for the first time may require hospitalization to undergo a full examination. We are located in the Central Administrative District, close to the Novoslobodskaya, Tverskaya, Chekhovskaya, Belorusskaya and Mayakovskaya metro stations.
Also, in case of attacks that do not go away for more than 5 minutes or recur after a short period of time, you can call an ambulance.
Complications of epilepsy
Epilepsy is fraught with the development of a number of serious complications, including:
- Status epilepticus is a series of generalized seizures requiring medical intervention.
- Injuries. If a patient falls, they can suffer serious injuries, sometimes fatal (for example, if they hit their head on a hard object).
- Increased intracranial pressure. Patients with epilepsy may complain of severe headaches and dizziness. Due to high intracranial pressure, patients may experience nausea and vomiting.
- Brain swelling. When fluid accumulates in the brain tissue, the patient experiences a noticeable increase in neurological symptoms. The condition may worsen to the point of coma.
- Strokes. These may be ischemic or hemorrhagic strokes. This complication arises due to the fact that in epilepsy the central regulation of vascular tone is disrupted. Against this background, in some cases, blood pressure rises sharply or the walls of blood vessels are damaged, which leads to ischemic stroke or hemorrhage.
- Thrombosis of intracranial veins. Dysregulation of vascular tone can also lead to venous stagnation, which can lead to thrombosis. In rare cases, the disease is complicated by pulmonary embolism, which can be fatal.
- Aspiration pneumonia. This is one of the most severe complications of epilepsy. During an attack, the patient may vomit. Sometimes a person swallows vomit, which can enter the lungs. This causes a severe inflammatory process in the lungs, which leads to empyema - an accumulation of pus in the pleura.
Sleep epilepsy or sleep disorder
How to distinguish between nocturnal seizures, are seizures a manifestation of epilepsy during sleep or is it a sleep disorder?
Differential diagnosis of paroxysmal events during sleep
To clarify the nature of nocturnal attacks, an objective research method is video EEG polysomnography. An option for diagnosing epilepsy in sleep is video EEG monitoring; studies are more informative after sleep deprivation.
If during a paroxysm epiactivity is simultaneously recorded on the EEG of sleep, then these paroxysms are of epileptic origin, that is, they are epileptic seizures in sleep.
Night attacks can be short and not accompanied by epileptiform EEG discharges; then these disorders of non-epileptic origin are more often classified as parasomnias.
Sleep disorders are often associated with certain stages of sleep and have a characteristic clinical picture.
At an appointment with an epileptologist, there are also options when the patient has nocturnal seizures and epilepsy, but this is not epilepsy.
Let us give a clinical example of seizures during sleep, accompanied by epileptiform activity on the EEG, but not related to epilepsy.
A 3-year-old boy came to see him with nocturnal paroxysms in the form of sleepwalking and sleep-talking. According to my mother: “2 hours after falling asleep, he gets out of bed, says, and walks around the apartment. It's like he's looking for something. More often than not, something is unclear. Some of the words can be understood; they are associated with sleep, with the events of the day. Sometimes the son laughs, cries, moans, is afraid, and is in a hurry. The eyes are open, but the gaze is unconscious or “wild”. After about 10 minutes I manage to calm him down and put him to bed. He falls asleep calmly. After treatment with sedatives, there was a break in his sleepwalking for 4 months, and then gradually became more frequent up to 2-4 times a month.” On the EEG, the patient has epiactivity of the type of benign epileptiform discharges of childhood in a small amount in the background and during sleep. When conducting an EEG with sleep deprivation: during sleep recording, neurophysiologists described a paroxysm (sat down on the bed, did not react, said a few words), but at this moment no epiactivity was noted in the EEG. A diagnosis was made: Parasomnias (sleeping, sleeping). Concomitant diagnosis: Benign epileptiform disorders of childhood. There are currently no data for active epilepsy. Antiepileptic drugs were never prescribed to this patient. Emphasis was placed on the need to maintain a rational daily routine. In therapy, he received sedatives or nootropics in age-related doses in the form of monotherapy (pantothenic acid, adaptol, atarax, phenibut, decoction of sedative herbs, novopassit) in courses of 1-2 months, 1-3 courses per year. The response to such therapy is always good: the parasomnias described above completely stopped for 4-8 months or decreased significantly; could be of an erased nature (sits on the bed in a dream, sits for 3-5 seconds, lies down and sleeps further; no more than 1-2 times a month). The child has been observed by an epileptologist for several years. Over time, complaints about sleep disturbances gradually become less and less. According to the EEG, epiactivity of the DERD type persists: in different recordings it may be in a small index or absent.
Sources
- Kissin M.Ya. Clinical epileptology. – M.: GEOTAR-Media, 2009. – 256 p. : ill.
- WHO official website - https://www.who.int/ru/news-room/fact-sheets/detail/epilepsy
- Avakyan G. N. Blinov D. V. Lebedeva A. V. Burd S. G. Avakyan G. G. Classification of epilepsy of the International League Against Epilepsy: revision and update 2021. Epilepsy and paroxysmal conditions. 2017; 9 (1): 6–25. DOI: 10.17749/2077–8333.2017.9. 1.006–025.
- Zenkov L.R. Clinical electroencephalography (with elements of epileptology). – M.: MEDpress-inform, – 2001. – 368 p.