Choking and lack of air is an extremely unpleasant and frightening sensation, especially when it wakes you up in the middle of the night. In addition, night suffocation is always a sign of some serious disease that must be treated.
In this article we:
Let's name the possible reasons why a person suffocates in his sleep;
We'll tell you what to do when you suddenly wake up at night from lack of air;
We will recommend which doctor to see.
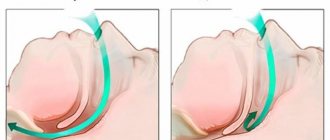
Obstructive sleep apnea syndrome
Obstructive sleep apnea syndrome (OSA) is the most common cause of shortness of breath at night.
This is how typical patients describe their condition. Compare the sensations with your own; perhaps you will recognize yourself immediately.
Valery:
“I didn’t know that I was suffocating in my sleep,” my wife said. For many years I just snored, but lately my breathing has also been interrupted. She often wakes me up, because sometimes I don’t breathe for a minute... In general, I sleep restlessly, I sweat a lot at night, and I often get up to go to the toilet. In general, I’m not happy with my sleep at all, or with my overall well-being. Drowsiness during the day, headache in the morning, high blood pressure...”
Kirill:
“A neighbor in a compartment on a train once told me that I suffocate in my sleep. Previously, I didn’t attach any importance to sleep at all, but after this incident I began to pay attention - and it’s true, there are problems. Sometimes I doze off in the evening and suddenly wake up abruptly, breathing quickly - as if there is not enough air. Or I wake up at night because I start snoring. Or I sleep restlessly, wake up and cough, and I also need to breathe before I fall asleep again. The Internet says it’s sleep apnea.”
So, the signs of obstructive sleep apnea:
- The sleeping person snores.
- In his sleep he suffocates. Stopping breathing occurs more than 5 times per hour and lasts 10 seconds or longer. The longest cessation of breathing recorded by the staff of our Sleep Medicine Center in a patient with apnea syndrome was 3.5 minutes.
- Often such pauses in breathing are observed by relatives and others. The patient himself, even with severe breathing problems, may not remember anything about the attacks of suffocation!
- In addition to snoring and respiratory arrest, there may be other symptoms: restless sleep, night sweats, heartburn (especially at night), frequent urination at night, daytime sleepiness, involuntary falling asleep during the day, morning headache, etc.
Look at the characteristic signs of breathing at night in a person with obstructive apnea in the video presented.
Typically, people who suffocate in their sleep due to obstructive sleep apnea are overweight men 40-60 years of age and older. Many have hypertension and heart disease. Apnea also occurs in other people (young people, women, children), but less frequently.
Sleep apnea is a serious condition. If left untreated, it can cause myocardial infarction, stroke, and sudden death in sleep.
If you suspect you have sleep apnea, consult a sleep specialist. You will undergo a polysomnography (overnight sleep study), an accurate diagnosis will be made, and the cause (or causes) and severity of the disease will be determined. After this, effective treatment will be recommended. The CPAP therapy method allows you to quickly stop suffocation during sleep, eliminate symptoms and reduce risks.
Causes of sleep apnea in adults
The term sleep disordered breathing covers a range of conditions characterized by abnormal breathing during the night. In many cases, this is due to narrowing or complete obstruction of the upper respiratory tract. Clinical manifestations can vary from partial airway obstruction without sleep disturbance to frequent episodes of apnea associated with repeated hypoxemia and microarousals.
Obesity is one of the common causes of obstructive apnea. Fat deposits in the neck area narrow the respiratory lumen of the pharynx and create an obstacle to the passage of air through the respiratory tract. However, contrary to popular belief, not all people with OSA are obese.
Sleep apnea in adults may be due to the following reasons:
- anatomical features: enlarged palatine tonsils; small lower jaw (micrognathia), lower jaw displaced back (recnognathia);
- problems with nasal breathing: deviated nasal septum; chronic sinusitis;
- obesity: increased risk of obstruction due to fatty deposits in the neck;
- drinking alcohol, smoking, taking sedatives;
- old age: with age, the incidence rate increases, because muscles lose tone;
- hormonal disorders (for example, during menopause in women);
- neurological diseases: stroke, amyotrophic lateral sclerosis, Alzheimer's disease, Parkinson's disease.
Heart failure
Specific description of the complaint.
Valentina:
“I have had heart problems for a long time, hypertension, 10 years ago I had a heart attack. I take pills... A couple of weeks ago it got worse. I can’t walk as much as before – I’m out of breath. When I go to bed at night, I’m also out of breath! I noticed that if you sleep on a high pillow or even half-sitting, it’s easier to breathe.”
Signs:
- A person suffocates not only in his sleep, but also simply in a lying position with a low headboard;
- Shortness of breath appears or worsens on exertion;
- A patient is a person with heart disease.
Patients with heart failure (chronic circulatory failure) may experience breathing problems at night. This is a sign of deterioration (decompensation). If you have heart failure, shortness of breath appears or worsens, and you begin to choke while lying down, be sure (urgently!) to consult a cardiologist.
Causes of lack of air
Difficulty in inhaling in healthy people is caused by a discrepancy between the amount of air inhaled and the need for oxygen. Such shortness of breath is disturbing when doing hard work, during intense training, climbing mountains, and in stressful situations. The appearance of a feeling of lack of oxygen is facilitated by wearing tight clothes, belts and corsets that interfere with normal breathing. In older people, as a result of age-related changes in blood vessels and heart, shortness of breath may appear with minimal exertion. The feeling of lack of air also manifests itself in a number of conditions and diseases.
Pregnancy
Shortness of breath with a feeling of insufficient inspiration occurs mainly in the 2nd half of the gestational age. As the uterus enlarges, the diaphragm is pushed upward, which limits the depth of breathing. The longer the pregnancy, the more often a lack of oxygen is felt, even with calm walking and minor exertion. In this case, the frequency of respiratory movements at rest increases to 22-25 breaths per minute. When shortness of breath occurs, a pregnant woman is usually bothered by slight dizziness, sometimes flashing “spots” and darkening in the eyes.
The symptom often appears and is more pronounced in patients who are carrying a large fetus, multiple pregnancies, or suffer from polyhydramnios. An aggravating factor is inferior vena cava syndrome during pregnancy. With aortocaval compression, in addition to shortness of breath, due to limited mobility of the diaphragm, women experience difficulty breathing and lack of air when lying on their back. Respiratory distress is combined with sudden weakness, severe dizziness and even fainting.
Pleurisy
Increasing shortness of breath with difficulty breathing is a characteristic sign of inflammation of the pleura. Respiratory disorders are caused by intense pain during dry pleurisy, accumulation of fluid in the pleural cavity - during an exudative, purulent, hemorrhagic process. Lack of air becomes the result of shallow, gentle breathing: in order to reduce acute stabbing or dull drawing pain over the affected area, the patient limits the volume of respiratory movements. Often shortness of breath is accompanied by a painful dry cough, fever, and chills.
Lung diseases
With inflammatory and diffuse damage to the lung tissue, the feeling of lack of inhaled air is associated with the exclusion of part of the lung from the respiratory process, limiting its mobility and elasticity. Patients complain of incomplete inspiration, weakness, fatigue, and dizziness. Signs of pulmonary dyspnea usually include:
- Lobar pneumonia
. Shortness of breath begins suddenly, simultaneously with a sharp rise in temperature to 39 ° C and above, severe headache, pain in the affected part of the chest, weakness, dry and later wet cough. Daily temperature fluctuations of 0.5-2 °C and profuse sweating are typical. - Interstitial pneumonia
. The feeling of “incomplete inspiration” appears gradually, first during exercise, later at rest. Lack of oxygen often worries you at night. Shortness of breath is accompanied by a dry cough, disrupts sleep, and provokes fatigue during the daytime. In an acute process, changes in breathing resemble the symptoms of lobar pneumonia. - Primary bronchopulmonary amyloidosis
. Difficulty in inhalation is pathognomonic for the deposition of amyloid in the wall of the trachea and large bronchi, while the patient’s heavy wheezing can be heard at a distance. If the alveoli are damaged, lack of air with a dry cough bothers you at the slightest movement, talking, or at rest. At the same time, due to damage to the heart and blood vessels, pressing pain occurs in the left chest, and the legs swell noticeably. - Pulmonary tuberculosis
. Lack of oxygen, causing shortness of breath, is characteristic of the primary tuberculosis complex and miliary process. The feeling of incomplete inspiration manifests itself against the background of an unproductive cough, pain in the chest, low-grade or high fever, severe weakness and sweating. In addition, with disseminated tuberculosis, skin cyanosis is pronounced. - Pulmonary zygomycosis
. Shortness of breath is preceded by a short period of severe intoxication with a temperature of 38°C, a dry or unproductive cough, in which blood may be detected. Shortness of breath worries almost constantly, even with complete rest. Difficulty in inhalation is combined with impaired exhalation. Later, severe chest pain occurs, further limiting breathing. - Sclerotic processes
. With diffuse pneumosclerosis, which developed as a result of post-radiation pneumonitis, pneumoconiosis, and other diffuse lung lesions, shortness of breath appears and increases gradually. In the terminal stages, the patient does not have enough air even at rest, due to oxygen deficiency, the skin becomes bluish, and the fingers are shaped like drumsticks (Hippocratic fingers).
Laryngeal stenosis
Most often, inhalation difficulties are caused by diseases in which, as a result of damage to the mucous membrane and vocal cords, obstacles are formed in the path of the movement of air masses. Dyspnea of laryngeal origin is often characterized by a feeling of limited air flow into the airways, wheezing, noisy breathing (stridor). The symptom is observed in the following pathological conditions:
- Acute laryngeal stenosis
. Difficulty in inhaling, noisy breathing, hoarseness, and hoarseness arise and increase extremely quickly. During inhalation, the intercostal spaces and epigastric region are retracted, the jugular fossae are sunken, and the wings of the nose are inflated. The patient shows anxiety, sometimes agitation, panic, feels the fear of death and, in order to facilitate the flow of air, leans on his hands. Breathing gradually becomes more frequent, becomes shallow, and cyanosis of the face and nail phalanges is possible. Acute stenosis complicates the course of croup, false croup, damage during tracheal intubation, and other pathologies accompanied by laryngeal edema. - Chronic stenosis.
A gradual increase in shortness of breath is typical for benign tumors and cancer of the larynx, laryngomalacia, other anomalies of organ development, laryngocele, neuropathic paresis, and damage to the thyroid gland. Symptoms increase slowly. Shortness of breath against the background of a barking cough and hoarse voice intensifies as the lumen of the larynx narrows, but the patient may not notice it for a long time due to gradual adaptation to hypoxia. In the later stages, the lack of air bothers you at rest; the intercostal muscles and abdominal muscles are actively involved in breathing. Lack of oxygen provokes memory impairment, sleep disturbances, and absent-mindedness.
Foreign bodies in the respiratory tract
When foreign objects enter the respiratory tract, breathing becomes difficult, up to the point of complete inability to inhale. The lack of air feels like suffocation. The patient shows anxiety, takes a forced position, breathes quickly and shallowly (“sobs”). A distinctive feature is the suddenness of the development of symptoms after accidental inhalation of food or small objects. Almost immediately, a paroxysmal cough begins with lacrimation, profuse salivation, and increased formation of nasal mucus. The face becomes purple and bluish.
If a foreign body remains in the respiratory tract, not completely blocking its lumen, extraneous sounds may occur when breathing. Balloting of objects in the lumen of the trachea is accompanied by hissing, buzzing, and whistling. Partial bronchial obstruction is characterized by a remotely audible whistle. At the same time, the intensity of the cough decreases, and mucous sputum with foreign body particles may be discharged. Shortness of breath becomes less frequent, but pain in the neck and chest increases. Subsequently, inflammatory processes occur.
Pulmonary and pleural tumors
Features of inspiratory dyspnea in malignant neoplasia depend on the location of the oncological process. However, in any case, respiratory disorders precede or complement specific symptoms of the disease and general manifestations in the form of fatigue, loss of appetite, and progressive weight loss. The feeling of inadequate breathing may bother patients who develop:
- Pleural cancer
. Shortness of breath caused by limited excursion of the lungs is possible both with a primary tumor and with metastatic damage to the pleural layers. Symptoms increase very quickly. In addition to incomplete gentle inhalation, which provokes a lack of air, there is pain in the affected half of the chest, weakness, and general exhaustion. - Bronchioloalveolar cancer
. Difficulty in inhaling during physical activity, and later at rest, is a late sign of a tumor. Often, shortness of breath develops against the background of a painful dry or profuse watery cough, indicates the presence of respiratory failure and precedes the onset of chest pain.
Heart diseases
Complaints about a lack of oxygen are one of the characteristic signs of cardiac dyspnea, which is detected in cardiac diseases that occur with rhythm disturbances (tachycardia, extrasystole, WPW syndrome) or insufficient blood supply to the myocardium (angina pectoris, unstable angina, other forms of coronary heart disease). The severity of the symptom usually directly depends on the degree and form of heart failure. In mild cases, shortness of breath is felt after moderate physical activity or with strong emotional experiences.
Pathological changes in the respiratory process in chronic heart failure are manifested by a feeling of lack of air and increased respiratory movements when performing simple physical exercises, everyday work, fast and then normal walking, at rest. Patients describe their sensation as a desire to inhale more air “full of the chest,” oh. Typical symptoms include cyanosis (cyanosis) of the nasolabial triangle, nails, swelling of the lower extremities, severe fatigue, complaints of discomfort, heaviness, and chest pain.
Emergency conditions
Shortness of breath with a feeling of acute lack of air is a harbinger or symptom of a number of disorders that require emergency medical care. Together with dizziness, fog and “floaters” before the eyes, “lightheadedness”, it indicates an approaching fainting (syncope). Severe respiratory distress and severe difficulty in inhaling are observed in such acute conditions as:
- Cardiac asthma
. Before or during an attack, there is a retrosternal stabbing, squeezing pain, interruptions in the functioning of the heart, and strong palpitations. An acute feeling of lack of oxygen is accompanied by cold sweat, cough (dry or with hemoptysis), fear of death, and severe weakness. Acrocyanosis is noticeable - blueness of the fingers and toes, lips, tip of the nose, and ears. The skin looks pale with a grayish tint. The patient tries to take a vertical position (orthopnea). Cardiac asthma can manifest itself as myocardial infarction, heart defects, and other cardiac pathologies. - Pulmonary embolism.
In acute cases, shortness of breath occurs suddenly and usually has the character of a painful lack of air with attempts to inhale it. The patient strives to maintain a horizontal position (“lying low”). Breathing quickens to 30-50 or more per minute, in the terminal stage it becomes rare, irregular, noisy (Biot, Cheyne-Stokes type). The skin noticeably turns pale, and as symptoms increase, it becomes bluish, gray-ashy, and in the lightning-fast form, a “cast iron” color. - Pulmonary hemorrhage
. Shortness of breath with a perceived incompleteness of inspiration develops and increases after an attack of persistent cough, at the end of which mucous sputum with scarlet blood or its clots is coughed up. In severe cases, dyspnea is accompanied by profuse bleeding from the respiratory tract, which is preceded by a burning sensation and tickling in the affected part of the chest. Against the background of frequent gurgling breathing, general disorders quickly increase: dizziness, noise in the head and ears. The skin turns pale and becomes covered with cold, sticky sweat, and signs of acrocyanosis are noticeable.
Chest and lung injuries
Respiratory disturbances in thoracic injuries can be either short-term or progressive. Thus, with bruised ribs, transient difficulty in inhaling is secondary and is associated with limitation of respiratory movements due to chest pain when deeply inhaling air. With closed traumatic or spontaneous pneumothorax, complaints of insufficient oxygen supply, rapid breathing, blue lips along with sharp stabbing pain in the chest, radiating to the arm and neck, cold sweat, drop in pressure, subcutaneous emphysema become leading in the clinical picture.
Neurotic disorders
Up to 75% of patients of neurologists and psychiatrists complain of frequent or constant lack of air, a feeling of a “damper” or other obstruction in the chest, making it difficult to breathe fully. Often, patients exhibit concomitant emotional disorders - anxiety, hypochondria, phobias, in particular, fear of death from suffocation. The key features of neurotic shortness of breath are the appearance or intensification after traumatic situations, vivid, figurative descriptions of experiences, and characteristic noise design (groans, groans, sighs). Shortness of breath is especially acute during a panic attack.
With cardioneurosis, somatoform dysfunction of the autonomic nervous system, vegetative-vascular dystonia, a typical combination of difficulty breathing with constant or paroxysmal palpitations, headaches, tingling in the precordial area, chilliness, sweating, and a tendency to turn pale or redden the face. A subjectively felt lack of incoming air (“empty breath”), forcing the patient to breathe frequently, deeply and noisily in the absence of somatic preconditions, is one of the variants of respiratory dysfunction in hyperventilation syndrome.
Bronchial asthma
Alyona:
“A week ago, I woke up suddenly in the middle of the night with tightness in my chest. I realized that I was suffocating. It was hard to breathe, harder when exhaling than when inhaling. I had to stand up and put my hands on the windowsill to feel at least a little easier. About 15 minutes passed. I was examined and was diagnosed with asthma.”
Choking in classic bronchial asthma is difficult to confuse with something else.
- The attack develops quite quickly;
- During suffocation, it is more difficult for a person to exhale than to inhale;
- The body position with a forward bend and support of the hands (on the knees, window sill) helps to breathe;
- The attack lasts up to 20 minutes;
- Choking quickly resolves with the use of specific drugs (for example, salbutamol);
- Not only nighttime, but also similar daytime attacks are possible.
If you find yourself short of breath in your sleep and have symptoms similar to asthma, contact your physician or pulmonologist.
What to do?..
Very often, patients report that when they suspected symptoms of apnea, they were at a loss: “What to do if you stop breathing during sleep? What to do? Who to contact?". Fortunately, we have answers to these questions.
First of all, it is important to understand: sleep apnea syndrome cannot be cured on your own at home. That is why the first step towards recovery should definitely be a visit to a doctor who deals with sleep problems - a somnologist. He will be able to diagnose apnea, assess the severity of the condition and select treatment appropriate to the situation.
A person suffocates in his sleep - other reasons
Perhaps the reasons why you suffocate in your sleep are still unclear to you. You may not have the combination of symptoms that we listed above when describing different diseases.
The feeling of suffocation can manifest not only physical, but also psychological problems - for example, nocturnal panic attacks. If you do not understand why you are suffocating in your sleep, contact a somnologist. A specialist will identify your problem and help you.
To make an appointment with a somnologist, call 85 or leave your contact details and we will call you back.
If you want to make an appointment with a doctor yourself, all contacts are listed here.
Stopping intermittent breathing
Doctors at the Yusupov Hospital treat breathing disorders due to VSD with sedatives, physical exercise, and psychotraining. During training sessions, psychologists try to teach the patient how to properly cope with a stressful situation. If the patient is simply very worried, take sedative medications - valerian, novo-passit, motherwort. If the patient has ever suffered a panic attack or has previously been diagnosed with neurosis, neurologists use tranquilizers, antipsychotics, and nootropic drugs. In severe cases, cyclic antidepressants are prescribed.
To relieve an attack of suffocation during VSD, the patient should be seated and calmed down. The patient needs rest. It is necessary to unfasten the compressive elements of clothing and ventilate the room. If this does not help, the patient needs a motherwort or valerian tablet. If there is information about a panic attack or neurosis, you must immediately give the medicine previously prescribed by a psychiatrist.
Diagnostic stages
The first step is to contact a specialist. The doctor will examine the patient and clarify his complaints about his general health. If necessary, he will redirect the patient to specialists from a medical institution specializing in a different profile.
To diagnose lack of air during inspiration at rest, the following are used:
- general blood and urine analysis,
- spirography,
- ECG,
- echocardiography,
- radiography,
- Ultrasound,
- CT.
Secondary studies can be prescribed in accordance with the individual characteristics of the body and the course of the disease.
Need for sleep and night awakenings
If a person sleeps less than he needs, then sleep deprivation occurs. If this happens constantly, then “debt” develops in a dream. Lack of sleep and poor sleep quality have been observed to cause severe changes in blood sugar levels. These changes may be due to decreased glucose tolerance or decreased insulin sensitivity. Lack of sleep affects the production of hormones that regulate appetite. As a result, the feeling of hunger increases, which, in turn, leads to overeating and weight gain. Weight gain can lead to obesity, which is often associated with sleep apnea. This is where the vicious circle begins.
Sleep problems have become more common in recent years, with studies showing that people's average sleep duration has become shorter. At the same time, the incidence of cardiovascular diseases, type 2 diabetes, depression and anxiety has increased. Chronic lack of sleep has adverse effects on health.
Other breathing disorders during sleep
Breathing disorders during sleep can also be a side effect of taking certain medications (for example, sleeping pills). In addition, there is hypoventilation syndrome, which is typical for patients with obesity, neurological and muscular diseases with reduced ventilation. Problems with breathing during sleep also occur in chronic lung diseases, such as chronic obstructive pulmonary disease (COPD), bronchial asthma, diseases associated with pulmonary fibrosis, bone deformities of the chest and spine. Single snoring can happen to anyone from time to time.