The prevalence of the genetic disease Huntington's chorea is about 10 cases per 100 thousand people in the world. Pronounced signs of diagnosis include disturbances in the functioning of the musculoskeletal system, convulsions, sudden unconscious jerks of the limbs and deterioration of consciousness. Treatment for Huntington's chorea (a disease involving a disorder of the protein structure of genes) has not yet been created; it is only possible to reduce the patient's symptoms with medication, as well as help reduce movement disorders.
From the history of the disease
Since the classic symptoms of chorea are erratic arm movements and an unsteady gait accompanied by dancing movements, it is not surprising that the Greek word chorea, which means “dance,” eventually became the name for this disease.
One of the first doctors to describe this serious illness was Paracelsus (1493-1541). Describing the phenomena of religious ecstasy in the form of the dance of St. Vitus, popular in the Middle Ages and the Renaissance, he discovered people demonstrating severe pathological symptoms. Much later, already in the 17th century, the doctor T. Sydenham described chorea, which appears in childhood and was named in his honor. And only in 1872, D. Huntington (Huntington) described a hereditary form of chorea that debuts in adults. Now this disease is called chorea or Huntington's disease (abbreviated as HD).
In 1993, an international team of genetic researchers discovered a mutation that causes HD.
Classification
All over the world, doctors identify several forms of the disease. For example, primary forms include the following types:
- Huntington's chorea.
- Neuroacancytosis, or choreoacanthocytosis.
- Benign - non-progressive hereditary form.
- Lesch-Nyhan disease.
Secondary forms can be caused by autoimmune diseases, infections, metabolic disorders, brain damage, and intoxication. That is, here the disease begins to manifest itself against the background of some other pathology, which became the trigger. You can see exactly what the disease looks like in a photo on the Internet.
But there is another classification of chorea disease. In this case, the following types are distinguished:
- Hereditary, which includes Huntington's chorea, hereditary non-progressive with early onset and chronic with late onset.
- Occurring in extrapyramidal diseases.
- Secondary forms.
However, no matter what classification it belongs to, almost all types of this disease have the same symptoms.
Causes of chorea
We are talking about serious genetic changes: this is the HNT gene, which is responsible for the development of pathology. Its location is the fourth chromosome. It has the ability to encode a special protein called huntingtin. How it works normally is unknown to science, but if it changes due to genetic abnormalities, HD occurs.
As the protein changes its structure, it causes nerve cells in the human brain to begin to function incorrectly and eventually die. Huntingtin is a complex substance, so the course of the disease is complex and multivariate. Modern researchers continue to actively study Huntington's chorea, trying to better understand the specifics of the basic mechanisms of its development.
The mutation that causes chorea is contained in all cells of the patient’s body, so we are talking about a classic hereditary disease.
Description
Chorea is a type of involuntary movements (hyperkinesis), which are characterized by a sweeping or shaking character.
Movements in this pathology are sudden, unrelated and cannot be controlled by the person.
Chorea in children and adolescents is much more common than in adults. However, despite this, the disease can also occur at the age of 30–40 years, which is much less common. Chorea is not a very common disease. According to statistics, it is diagnosed in 1 person out of 10,000 people. Moreover, it is important to note that chorea is diagnosed in men an order of magnitude more often than in women.
The reasons for the development of chorea are numerous:
- hereditary diseases, for example, Huntington's chorea, which manifests itself as a gradual increase in the manifestations of chorea with accompanying intellectual impairments. Wilson-Konovalov disease is also hereditary. The essence of the disease is a violation of copper metabolism, as a result of which copper accumulates in the liver, cornea and basal ganglia of the brain, which are responsible for regulating tone and coordinating movements;
- cerebral palsy (CP). Not always, but in some cases, in addition to the main symptoms of the disease, involuntary movements of a sweeping nature may be observed;
- Sydenham's chorea (“minor chorea”) develops as a result of a streptococcal infection;
- chronic insufficiency of blood supply to the brain;
- vasculitis (inflammation of the walls of blood vessels) of the brain;
- taking certain medications, for example, long-term use of antipsychotics, abuse of centrally acting drugs.
As a rule, the prognosis for chorea is not very favorable. Death in these patients occurs not due to the disease itself, but to severe complications. Typically, death in patients occurs 12–15 years after the diagnosis of the pathology. Patients with chorea rarely live beyond 35 to 45 years of age. People who have relatives suffering from this disease are not recommended to have children. Adoption may be a way out of this situation.
Symptoms of chorea
The time of appearance of the first symptoms of chorea is middle age (period from 35 to 55 years). About 10% of clinical cases of HD occur in childhood and adolescence. In such situations, experts talk about juvenile chorea.
The development of the disease often occurs latently and is unnoticeable at first, so it can be diagnosed late.
The symptoms of chorea are varied. For example, it can manifest itself with a combination of symptoms (the patient’s mood constantly changes and difficulties in thinking arise). The development of symptoms depends on age and severity of the pathology. Some patients demonstrate predominantly motor disorders with mild mental disorders, while others, on the contrary, show anxiety, signs of depression or other mental disorders. The exact time when the first symptoms appear is difficult to determine.
Movement disorders
Movement disorders associated with chorea are usually called:
- actually, trochee;
- bradykinesia;
- dystonia.
These symptoms prevent the patient from being in a natural physiological position, disrupting the processes of walking and balance. “Dance” is expressed in involuntary movements that a person cannot control. Bradykinesia manifests itself in the slowness and complexity of voluntary movements, and dystonia manifests itself in the formation of unnatural and awkward poses, accompanied by “twisting” or twitching of the limbs. Also, movement disorders that occur with Huntington's chorea include dysfunction of the eye muscles, problems with swallowing and unclear speech.
Motor disturbances in the manifestations of chorea in adults are characterized by speed, pretentiousness and spontaneity. In this case, any muscle groups can be involved, and control of movements is absolutely impossible.
Usually, the onset of a pathological process is indicated by deviations observed during movements of the facial muscles. Patients grimace, stick out their tongues, raise their cheeks, curl their lips into a “tube,” frown and wink ridiculously. The progression of the pathology is accompanied by the appearance of involuntary movements in other muscles. Patients begin to quickly bend and straighten their fingers, then similar symptoms affect the lower extremities. Sometimes movements occur in the legs and arms at the same time.
Children suffering from chorea, on the contrary, demonstrate sluggish movements. They are very slow, and the child’s speech is slurred, with incorrect pronunciation of sounds and words, impaired speed and rhythm. From the motor sphere, oscillatory movements of the eyeballs are typical. The child cannot normally move his gaze from one object to another and focus his vision on a specific object.
When the disease begins in childhood and adolescence, experts note bradykinesia and muscle stiffness as the main symptoms. Children do not demonstrate violent movements, as with classical chorea in adults. Also, juvenile chorea is characterized by disturbances in behavior and learning with rapid progression of the entire symptom complex.
When the disease begins in a later age, chorea itself is its leading symptom, and its heredity is very easy to identify. Most often, the parents of an adult patient are no longer alive, since they simply do not live to see the moment when their offspring begin to experience severe symptoms of chorea.
Free consultation on training issues
Our consultants are always ready to tell you about all the details!
Diagnostics
Photo: wagnertour.de
Diagnosis of chorea begins with the collection of complaints and anamnesis of the disease. The time of occurrence of the first involuntary movements is specified, with what frequency they appear, and what precedes them. It is also important to find out whether anyone in the family had similar symptoms (only blood relationships are taken into account). In addition, since in some cases chorea occurs as a result of taking certain medications, you should find out which drugs the person has been taking for a sufficiently long period of time.
When examining the patient, the existing involuntary movements are assessed. Muscle tone is also assessed, which will be increased with chorea, and a decrease in muscle strength is noted. In addition to the neurological examination, a general examination is performed, which includes auscultation, percussion and palpation of vital organs. This is necessary to assess the general condition of the body. In addition, it allows you to identify signs of Wilson-Konovalov disease (liver enlargement, brown spot on the cornea of the eyes (Kayser-Fleischer ring)), which can also cause the development of chorea.
General laboratory tests are not able to establish changes in indicators specific to chorea. If Wilson-Konovalov disease is suspected, the amount of copper in the blood and the level of ceruloplasmin (a protein that transports copper ions in the blood) are determined. The presence of Wilson-Konovalov disease will be indicated by a decrease in ceruloplasmin, which leads to impaired copper metabolism. Liver function will also suffer, so a biochemical blood test will reveal an increase in the level of liver enzymes.
Among the instrumental research methods, CT (computed tomography) and MRI (magnetic resonance imaging) are used. These studies allow us to assess the condition of the brain. MRI makes it possible to study the structure of the brain layer by layer; the state of the basal ganglia, which are responsible for regulating tone and coordinating movements, is of particular interest.
EEG (electroencephalography) is used to assess the functional state of the brain. This is the most accurate research method, reflecting the slightest changes in the function of the cerebral cortex and deep structures. Based on recording in the form of a curve of bioelectric signals coming from each brain cell. Deciphering the resulting graphic curve allows us to determine the consistency of the work of various parts of the brain and assess the depth and degree of dysfunction of neurons.
Mental changes
The psyche in HD undergoes gradual pathological changes. A decrease in a person’s ability to fully think is characterized, first of all, by problems with memory and a decrease in the critical threshold for perceiving one’s own state. The patient becomes anxious, irritable or, conversely, apathetic. In severe cases, hallucinatory or delusional syndromes develop. Suicidal behavior is also common in the context of severe depression.
Also, the following mental symptoms may appear:
- aggressive outbursts;
- insomnia;
- impulsiveness and spontaneity in behavior;
- social alienation.
Delusions and hallucinations are much less common. As for mental disorders, as the disease progresses, patients gradually lose memory acuity, logic and concentration. They find it difficult to make independent decisions and give clear answers to even the simplest questions. Over time, they learn new information worse and worse, which is an obvious sign of progressive dementia.
Stages of flow
Dr. A. Scholsen from Georgetown University (USA) proposes five stages of chorea development as a classification:
- early The patient has been diagnosed with Huntington's chorea, but so far his full functions have not been impaired;
- intermediate early. A person is able to work and have normal contact with society, but difficulties in thinking, movement and behavior are already making themselves felt. Patients can still cope with everyday activities and work;
- intermediate late. The patient is no longer able to work, but he still does household chores himself;
- late initial. The patient loses independence, but at home retains a number of functions - subject to the regular participation of other people in his daily life;
- late. Help is needed all the time, including professional care. Note that the late stage of the disease requires a special approach and skills from the people around the patient.
Clinical case of detection of Huntington's disease
Huntington's disease is an autosomal dominant neurodegenerative disorder characterized by progressive cognitive decline, involuntary movements, and incoordination beginning in middle age.
George Huntington first described the condition in 1872 after studying a familial case of the disease in Long Island residents.
The prevalence of Huntington's disease is approximately 10 cases per 100,000 population, and, given its late onset, approximately 30 people in 100,000 have a 50% risk of developing it in their lifetime. Although the disease most often manifests itself at the age of 35-40 years, the age range of its onset is quite wide: the earliest onset is noted at the age of 3 years, and the latest at 90 years.
Chorea begins gradually. The first signs of Huntington's chorea appear at the age of 25-50 years, less often in childhood. Men get sick more often than women; the first symptoms may be restlessness, fussiness of movements, which is not regarded by the patient and his relatives as a disease. Over time, however, movement disorders increase and can lead to disability. Characterized by frequent, sudden, irregular convulsive movements of the limbs or torso. Spasms of the facial muscles, sobbing, and articulation disorders are possible. Coordination of movements when walking suffers: the gait becomes “dancing” (trochaic). Memory remains intact until the later stages of the disease, but attention, thinking and executive functions are impaired already at the very beginning of the disease. Depression, apathy, alienation, irritability, and periodic disinhibition are often observed. In some cases, delusions and obsessive states develop, which is why schizophrenia is initially misdiagnosed.
The duration of the disease varies, but the average is 15 years. At early onset (before 20 years), the disease is accompanied by rigidity, ataxia, cognitive impairment and progresses more quickly (average duration is 8 years). Epileptic seizures rarely occur in late-onset Huntington's disease and often occur in early-onset Huntington's disease.
Typically, Huntington's chorea manifests itself in the 4th-5th decade of life as progressive choreoathetosis, which is accompanied by severe mental disorders (dementia, depression with frequent suicidal attempts, disturbances in emotional control with frequent outbursts of irritation and aggression). Sometimes it manifests itself in adolescence as an increasing akinetic-rigid syndrome.
The disease is characterized primarily by damage to the striatum. At the advanced stage, CT or MRI reveals atrophy of the caudate nuclei, which form the lateral walls of the lateral ventricles. Microscopic examination does not reveal pronounced changes (such as amyloid plaques and neurofibrillary inclusions in Alzheimer's disease). Gliosis and death of predominantly GABAergic neurons in the caudate nucleus and putamen are characteristic. Cholinergic neurons remain relatively intact. In the basal ganglia, the concentrations of GABA and glutamate decarboxylase, an enzyme involved in the synthesis of this mediator, are significantly reduced. Concentrations of other mediators, including substance P and enkephalins, are also reduced. Magnetic resonance spectroscopy reveals an increase in lactate concentration in the basal ganglia. In animals, administration of 3-nitropropionic acid, a succinate dehydrogenase inhibitor, causes a condition resembling Huntington's disease.
The diagnosis is confirmed by genetic testing.
The Huntington's disease HD gene is located on segment 4p16.3, contains CAG trinucleotide repeats, and encodes a protein called huntingtin. This protein is found in neurons of various parts of the brain; its function is unknown. Inactivation of a homologous gene in mice in a homozygous state causes the death of the embryo; heterozygous individuals do not differ phenotypically from the norm. Mice with an increased number of trinucleotide repeats in this gene develop progressive motor disorders. An increase in the number of CAG repeats leads to the appearance of a long polyglutamine region in the protein encoded by this gene, which may be the cause of the disease. The long polyglutamine stretch is believed to interfere with protein binding as well as other cellular processes, such as mitochondrial activity. Impaired binding of huntingtin to glyceraldehyde phosphate dehydrogenase has been reported. In addition, there is evidence of increased neuronal apoptosis in this disease.
Detection of an increase in the number of CAG trinucleotide repeats in the HD gene underlies the gene diagnosis of Huntington's disease. If the number of CAG repeats is 38 or more, then the disease will inevitably develop with age. The probability of inheriting an abnormal gene and, consequently, developing Huntington's disease in children of such patients is 50%. The more trinucleotide repeats a gene contains, the earlier the disease begins. However, in most cases the number of repeats is 40-49, and within these limits there is no relationship between the number of repeats and the age of onset of the disease. For unclear reasons, the risk of a significant increase in the number of trinucleotide repeats and the development of the juvenile form of Huntington's disease (a form of anticipation) is higher if the patient's father is sick.
Blood relatives may be advised to undergo genetic testing. Careful genetic counseling is necessary before DNA testing is performed on healthy individuals at high risk for Huntington's disease, as positive DNA testing can result in severe emotional distress.
Medical genetic counseling and DNA analysis are used not only in determining the risk of Huntington's disease, but also in the differential diagnosis of this disease. Thus, the mutant HD gene is sometimes found in sporadic “senile” chorea. In diseases resembling Huntington's disease, such as schizophrenia, benign familial chorea, hereditary ataxias, abetalipoproteinemia and familial Alzheimer's disease, the number of trinucleotide repeats is not increased.
There is no specific treatment. Treatment is predominantly symptomatic.
Clinical case
Patient S., 57 years old, was admitted for treatment to the II neurological department on December 7, 2014. with complaints of general weakness, progressive decline in memory, attention, dizziness, unsteadiness when walking, headaches, irregular involuntary violent muscle twitching in the torso and all extremities.
From the anamnesis it is known that for several years he has been suffering from hypertension with moderate blood pressure, widespread osteochondrosis of the spine, discirculatory encephalopathy with vestibulo-atactic syndrome.
The condition worsened for about 1.5 years, when the clinical picture showed irregular involuntary violent muscle twitching in the torso and all extremities, and slowly progressive cognitive impairment began to be noted.
In neurological status: Conscious, contactable, oriented. Emotionally labile. The background mood is reduced. Markedly fixed on her feelings, anxious, hypochondriac. There are no meningeal signs. CMN: Palpebral fissures D=S. Pupils D=S. Photoreactions are live. Movement of the eyeballs is not limited. There are no sensory disturbances on the face. The exit points of the trigeminal nerve are painless. The face is symmetrical. There is no nystagmus. The pharyngeal reflex is preserved. Swallowing and phonation are not impaired. Tongue in the midline. There are no paresis. Tendon reflexes are animated, with an expanded zone, S=D. Pendulum-like twitching of the legs is noted when examining knee reflexes. No pathological foot signs are detected. Paravertebral points and spinous processes in the cervical and lumbar regions are painless. No sensory disturbances are detected. Romberg's posture is unsteady. Dysmetry when performing PSP, PCP on both sides. Muscular dystonia. Spontaneous non-rhythmic choreoathetoid hyperkinesis is detected in all limbs, trunk, and facial muscles. The gait is hyperkinetic with elements of ataxia.
Taking into account the patient's complaints, medical history and clinical picture, a differential diagnosis was made between the onset of Huntington's disease and chorea minor. The patient underwent an MRI of the brain, which revealed a picture of dyscirculatory encephalopathy and mixed atrophic hydrocephalus; EEG: The main resting rhythm is not sufficiently expressed, “flattened”, probably as a manifestation of dysfunction of the lower brain structures. Duplex angioscanning of the BCA, which revealed non-stenotic atherosclerosis of the extracranial parts of the brachiocephalic arteries; rheumatoid tests (C-reactive protein, antistreptolysin-O, rheumatoid factor) - within normal limits. Based on the data from the additional examination, the diagnosis of minor chorea seemed unlikely.
The patient was referred for consultation to the Research Institute of Neurology of the Russian Academy of Medical Sciences. The diagnosis of Huntington's disease was confirmed by the results of a medical genetic study.
The patient was prescribed the experimental drug Pridopirin, which she is currently taking with some positive effects (memory, attention have improved somewhat, self-care skills have improved - the patient goes to the store on her own, prepares food).
In December 2015 The patient underwent a planned course of vascular-metabolic therapy in the II neurological department of Clinical Hospital No. 1, and was discharged with improvement, a decrease in the severity of vestibulo-atactic manifestations, and stabilization of the background mood.
Forms of the disease
Based on the specifics of symptoms, the following forms of chorea are distinguished:
- hyperkinetic. It is characterized by spontaneous motor acts, which, as noted earlier, are not subject to conscious control. Also, speech disturbances due to hypertonicity of the facial muscles are typical for the hyperkinetic form of chorea. Sometimes patients have convulsions and uncontrolled oculomotor acts during sleep;
- akinetic-rigid. Severe muscle hypertonicity;
- mental. Dementia gradually develops, and the patient's personality undergoes destructive changes.
Psychotic phenomena for the latter form are also a characteristic feature.
Clinical manifestations
Choreic movements are short, fast and irregular, often twisting, uncontrollable and sometimes strange. With severe forms of chorea, a person can be practically excluded from everyday life. Symptoms may worsen with emotional stress.
Mild initial symptoms of chorea disease:
- minor dyskinesias – restlessness, grimaces (motor imperfection);
- movements that seem purposeful;
- manifestations are mainly on the arms and legs.
Fully expressed chorea:
- dance movements standing and walking;
- severe motor imperfection;
- choreic movements of the torso and limbs;
- hyperkinetic dysarthria;
- swallowing disorders in the oral phase.
Non-drug treatment
In some cases, patients respond well to non-drug therapy in the form of:
- psychotherapeutic influence;
- exercise therapy;
- classes with a qualified speech therapist;
- breathing exercises;
- occupational therapy.
Regular use of these methods (of course, if the patient’s condition allows) can significantly reduce the intensity of pathological symptoms both physically and mentally. It has been proven that patients’ psycho-emotional background improves, they begin to better control their voluntary movements. Walking becomes more stable, as do swallowing and balance.
Physical exercise is one of the effective ways to slow down the development of movement disorders. There are special exercise therapy programs developed for such patients, which have repeatedly shown their effectiveness.
Drug treatment
Doctors use strong medication treatment in severe cases of chorea. One popular drug is tetrabenazine. It was developed specifically for the treatment of Huntington's chorea as a drug that reduces hyperkinesis.
Antipsychotics and drugs used for Parkinson's disease are also prescribed. The administration of antiparkinsonian drugs improves motor functions, and antipsychotics (for example, haloperidol, chlorpromazine, clozapine, etc.) alleviate the condition of patients with delusional and hallucinatory phenomena. If the patient is depressed, he is prescribed antidepressants; for insomnia, sedatives and sedatives are prescribed.
Special therapeutic procedures
Chorea, for which there is no cure as such, may be relieved to some extent by deep brain stimulation. But there are only a few case reports of its use, with conflicting results and prognosis.
Very good effects are seen in late motor complications of Parkinson's disease, where deep stimulation of the subthalamus and internal genital bone has already become part of clinical practice.
Valproate or carbamazepine are used in the treatment of paroxysmal choreoathetosis.
For some diseases, there are a number of treatment procedures. For example, drug-induced chorea can be affected by stopping the use of the drugs causing the problem. But sometimes the late effects of taking antipsychotics can persist for a long time after the drug is discontinued.
Sydenham's chorea (even without treatment) is characterized by spontaneous regression, but relapses are also common.
Antibiotic therapy plays an important role in the treatment of the disorder; Corticosteroids may help, and plasmapheresis has been tested with varying effects.
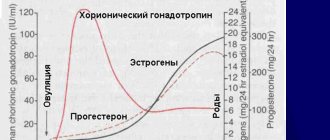
Signs that appear during pregnancy recede after childbirth, which are sometimes caused prematurely (in severe clinical illness).
In the treatment of chorea in Wilson's disease, specific treatment is carried out with chelates or zinc.
Choreic symptoms in autoimmune diseases respond favorably to treatment of the underlying disease. Corticosteroids and other immunosuppressive or modulatory therapies provide significant and early relief.
If the disorder occurs with hyperthyroidism or thyrotoxicosis, a positive response is provided by the correction of these disorders.
Traditional methods for muting symptoms are ineffective.