Article for the “bio/mol/text” competition: Nowadays it’s difficult to find a person who has never heard of Alzheimer’s, Parkinson’s or Huntington’s diseases. These diseases belong to a group of neurodegenerative diseases that cause the death of neurons and the gradual destruction of the brain. Unfortunately, all of them are incurable. Therefore, scientists are actively working to uncover the mechanisms of development of these diseases and find therapy that will help save patients. In our study, we addressed a still little-studied question: what happens to the synaptic connection of neurons during the neurodegenerative process? The results of this work open a new direction for developing a cure for Huntington's disease and other neurodegenerative diseases.
Competition "bio/mol/text"-2013
This work took first place in the “Own work” category of the “bio/mol/text” competition 2013.
The competition is sponsored by the visionary Thermo Fisher Scientific. The sponsor of the People's Choice Award is Helicon.
As life expectancy increases, more and more people are suffering from Alzheimer's disease and Parkinson's disease. Unfortunately, years of research have not yet led scientists to discover the causes of the development of these diseases and possible therapy. This is mainly due to the fact that almost nothing is known about the factors that cause the disease, and also because very few patients have a genetic predisposition. Most often, these diseases are sporadic, i.e. the reasons for their occurrence have not been established. This leads to endless debate - no one knows how to artificially induce this disease in model animals for experiments and drug discovery. Therefore, more and more scientists are turning their attention to genetic diseases of the nervous system, such as Huntington's disease (HD). This disease, like Alzheimer's disease and Parkinson's disease, belongs to the group of neurodegenerative diseases, with which it shares a number of similar features: death of neurons in the central nervous system, accumulation of amyloid-like protein aggregates, cognitive and motor impairments in patients. At the same time, HD has an important advantage from the point of view of researchers, because it is known which mutation causes this disease. This makes it possible to create precise genetic models and study them in animals. This is important because if we understand the pathogenesis of Huntington's disease, it will be easier for us to understand sporadic neurodegenerative diseases. This is what we tried to do in our study.
What is Huntington's disease?
Huntington's disease (Huntington syndrome, Huntington's chorea, or Huntington's chorea) is a genetic, progressive neurodegenerative disease characterized by the gradual development of involuntary muscle movements affecting the arms, legs, face, and trunk, and the progressive decline of cognitive processes and memory (dementia).
Neurological movement abnormalities may include uncontrolled, irregular, fast, jerking movements (chorea, choreic hyperkinesis) and athetosis, a condition characterized by relatively slow, writhing, involuntary movements. Dementia is usually associated with progressive disorientation and confusion, personality disintegration, impaired memory control, anxiety, agitation, and other symptoms and signs. In patients with the disorder, the duration of the disease can vary from approximately 10 to 25 years or more. Life-threatening complications may occur as a result of pneumonia or other infections, injuries associated with falls, or other related processes as a result of the disease.
Huntington's chorea is transmitted as an autosomal dominant trait. The disease occurs as a result of changes (mutations) in the HTT gene. The HTT gene, located on the short arm (p) of chromosome 4 (4p16.3), encodes a protein known as “Huntingtin.” This gene contains a region with a repeating sequence of three nucleotide bases - cytosine-adenine-guanine (i.e., CAGCAGCAG...). The length of expanded repeats may influence the age at onset of symptoms. The specific symptoms and physical signs associated with Huntington's disease result from the degeneration of nerve cells (neurons) in certain areas of the brain (eg, basal ganglia, cerebral cortex).
Huntington's disease
Huntington's disease (HD, also “Huntington's disease” in Russian literature) is a hereditary disease of the nervous system that affects approximately 1 in 10 thousand people. The disease was first described by George Huntington in 1872, and has since been named after him, but the clinical symptoms of this disease were known in the 16th century under the name “chorea” (from the Latin choreus - dance). Signs of chorea included involuntary, uncoordinated rapid movements similar to convulsions; This is exactly how modern doctors describe the motor disorders characteristic of HD. The disease can sometimes last up to twenty years, but the outcome is invariably the same: the patient loses the ability to move independently, speak, and then think. Typically, symptoms of Huntington's disease begin between the ages of 30 and 50, although 5–10% of patients experience the onset of symptoms before the age of 20—the so-called juvenile form of the disease [1].
The first symptom of Huntington's disease is involuntary twitching of the limbs, torso and facial muscles. Quite often they are accompanied by sudden mood swings, depression, irritability, slurred speech and clumsy movements. As the disease progresses, these symptoms include difficulty or pain when swallowing, unsteady gait, loss of balance, impaired thinking and memory impairment. Eventually, the patient loses the ability to move without the help of others and usually dies from pneumonia, cardiac arrest or other complications.
An important feature of HD for doctors and researchers is that the disease is hereditary and is caused by a mutation in a single gene. It turned out that the development of HD is caused by an increase in the number of repeats of the CAG triplet encoding glutamine in the first exon of the huntingtin protein gene. Moreover, the greater the number of repeats of this triplet, the earlier the development of the disease begins. Normally, there are from 10 to 35 repeats in the human population. In patients with HD, the number of repeats can be from 36 to 121, in the juvenile form - from 50 and above [2]. Thanks to the identification of the genetic basis of the disease, diagnosing HD is currently not a problem; In addition, prenatal diagnosis of the disease and testing of embryos before implantation during IVF have become possible, which allows even carriers of the mutant gene to have healthy children.
Unfortunately, identifying the exact mutation still does not allow scientists to determine the cause of Huntington's disease and find appropriate treatment. The appearance in a cell of a mutant gene and, accordingly, an altered (mutant) protein can lead to the development of pathology in two ways: loss-of-function or gain-of-functin. In the first case, the mutant protein cannot perform the same function as a normal protein, and this leads to disruption of cellular processes. In the second case, the mutant protein interferes with the normal functioning of the cell, beginning to perform some kind of “extra function.” To understand what happens in HD, scientists are intensively studying both the function of the normal huntingtin protein and the behavior of its mutant form [3].
Unfortunately, attempts to determine the precise cellular function of huntingtin have so far been unsuccessful. Various studies indicate the involvement of this protein in a wide range of biological processes, including the transport of proteins and vesicles (membrane transport vesicles), cytoskeletal organization, clathrin-mediated endocytosis, postsynaptic signaling, transcription regulation and anti-apoptotic processes [4]. If it can be proven that disruption of any of these functions is key to the development of the disease, then drugs to support this function could save patients with Huntington's disease.
If the gain-of-function hypothesis is correct, special attention should be paid to the behavior of the mutant form of huntingtin. It turned out that the mutant protein forms aggregates, which are one of the characteristic features of HD development in both humans and model animals (see sidebar). At first, aggregates were described only in the nucleus, but subsequent work also revealed them in the cytoplasm and processes of neurons [5]. In recent years, many authors are inclined to believe that the formation of aggregates has a rather protective function, and the main pathogenic form of mutant huntingtin is a monomeric soluble protein [6].
What kind of disease is this?
Huntington's disease is a severe genetic pathology of the nervous system of a degenerative nature with irreversible consequences.
The second name is Huntington's chorea :
- Translated from Greek, “trochea” means dance.
- The disease got its name because of the main symptom - continuous uncontrolled movements, somewhat similar to dance dynamics.
The second main symptom is a disorder of intelligence to complete dementia (dementia). The prevalence is low - 5-7 cases per 100 thousand people. The disease most often does not manifest itself until the age of 30-35.
Reference ! Often the first signs are either completely ignored by the patient and his environment, or are interpreted completely incorrectly, followed by irrelevant treatment. For example, in psychiatric clinics.
The total duration of Huntington's chorea, as a rule, does not exceed 10-12 years from the moment the first symptoms appear and ends in death from secondary infections or suicide. Moreover, according to statistics, the percentage of suicides among the dead is quite high.
What kind of disease is this, what are its clinical manifestations and causes are shown in the video:
Models for studying Huntington's disease
Animal models of HD appeared more than 30 years ago. The first were models based on the introduction of neurotoxic substances into the striatum (for example, quinolinic acid, an NMDA receptor agonist), which caused neuronal death. Currently, most researchers are working on transgenic animal models, which include not only mice and rats, but also invertebrate animals - the fly Drosophila melanogaster and the worm Caenorhabditis elegans.
Mouse models of Huntington's disease differ from each other in the number of CAG repeats and the level of expression of the transgene - the artificially introduced huntingtin gene. Because The development of HD depends on these factors; different strains of mice differ from each other in the rate of development of pathologies. The most widely used models include the R6/2, R6/1, and YAC128 mouse strains, which were also used in our work. In mice of these lines, the symptoms of the disease are most pronounced and appear quite quickly. In addition, these animals develop cognitive and motor impairments with age and develop partial loss of neurons in the striatum and cortex.
Another way to model HD is to use cell culture. In the simplest case, cell cultures with stable transfection of the huntingtin gene are used. For example, these are PC12 cells containing an inducible transgene of the first exon of huntingtin or striatal neurons expressing huntingtin fragments of different lengths. In addition, primary cultures from neurons from transgenic mice or immortalized neurons can be used.
Signs and symptoms
Signs and symptoms of the disease (see video) most often appear in adults aged 30-50 years, but can appear at any age. Symptoms tend to worsen over 10-25 years.
Over time, Huntington's disease or its complications are fatal.
According to the Huntington's Disease Society of America, symptoms of the disorder can be similar to amyotrophic lateral sclerosis (ALS), Parkinson's disease and Alzheimer's disease all rolled into one.
Main symptoms include:
- personality changes, mood swings and depression;
- problems with memory and judgment;
- unsteady walking and uncontrolled movements (choreic hyperkinesis);
- difficulty speaking and swallowing;
- weight loss.
How the signs and symptoms of the disease progress depends on the individual. In some patients, depression occurs before motor skills are affected. Mood swings and unusual behavior are usually the first to appear.
— Early signs and symptoms.
Early symptoms may not be recognized if the disease has not previously run in the family. It may take a long time to establish a diagnosis.
Initial signs and symptoms include:
- slight uncontrolled movements;
- minor changes in coordination;
- minor mood changes;
- lack of attention, slight problems with concentration and difficulties at work;
- lapses in short-term memory;
- depression;
- irritability.
The patient may lose motivation and focus and appear lethargic.
— Middle and late stage.
Over time, symptoms become more severe.
These include physical changes, loss of control of movement, and emotional and cognitive changes.
- Physical signs.
The patient may experience:
- difficulties communicating, including searching for words and slurred speech;
- weight loss leading to weakness;
- problems with eating and swallowing, since the muscles of the mouth and diaphragm may not obey;
- risk of suffocation, especially in later stages;
- uncontrolled movements.
There may be uncontrolled body movements, including:
- uncontrolled facial movements;
- twitching of parts of the face and head;
- clicking or fidgety movements of the arms and legs.
As the disease progresses, uncontrolled movements occur more frequently and with greater intensity. Over time, they may become slower as the muscles become more rigid.
- Emotional changes.
Emotional signs may alternate rather than occur sequentially.
These include:
- aggressiveness;
- anger;
- antisocial behavior;
- apathy;
- depression;
- excitement;
- panic;
- disappointment;
- lack of emotion becomes more and more obvious;
- dejection;
- stubbornness;
- cognitive changes.
May occur:
- loss of initiative;
- loss of organizational skills;
- disorientation;
- problems with focusing;
- problems with multitasking.
- Late stage.
Over time, the patient can no longer walk or talk and requires full-time care.
However, sufferers tend to understand most of what is said and recognize friends and family members.
Why we decided to study the parameters of synaptic transmission in Huntington's disease
Synaptic transmission is the transmission of signals between neurons using synaptic contact. When one neuron is excited, its synaptic ending releases a mediator into the synaptic cleft - a chemical substance that exerts its excitatory or inhibitory effect on the synaptic ending of the second neuron (Fig. 1). Thus, synapses connect neurons with each other, ensuring the normal functioning of neural networks and the entire nervous system. If any of the brain systems stops functioning, the reason may lie either in a disruption in the functioning of individual neurons, or in a disruption in the communication between them, i.e. disruption of synaptic transmission.
Figure 1. Schematic representation of the synapse structure.
"Wikipedia"
Huntingon's disease affects a specific area of the brain called the striatum. The striatum is part of an important neural pathway, the extrapyramidal system, which is involved in controlling movement and maintaining muscle tone. The death of striatal neurons in Huntington's disease leads to the destruction of the extrapyramidal system, which is associated with loss of control over movements in the sick person. But when the first pathological symptoms appear (tremor, loss of coordination), the human brain is not yet damaged: neurons begin to die only several years after the onset of the disease. Those. the disease begins when something changes in the functioning of the neurons themselves or in synaptic transmission, and these disturbances subsequently lead to the death of neurons and irreversible consequences.
The research results accumulated in recent years make many scientists inclined to believe that it is the disruption of the normal functioning of the neuronal communication system, synapses and synaptic transmission that leads to early disturbances in the functioning of the extrapyramidal system. It turned out that neurons with mutations in the gene encoding the huntingtin protein exhibit a number of pathological changes that disrupt synaptic transmission. In such mutant cells, the formation and renewal of the supply of vesicles (vesicles with a mediator) is disrupted, the intracellular concentration of calcium, which is necessary for the normal release of the mediator into the synaptic cleft, changes, the amount of a number of proteins necessary for the functioning of the synapse is reduced, etc. [7]. All this leads to a reduced release of the transmitter into the synaptic cleft, and if there is not enough transmitter, then the neurons begin to “hear” each other worse, and the commands sent by the cerebral cortex will not be carried out to the fullest extent.
In 2013, the Nobel Prize in Physiology or Medicine was awarded to works that made clear the details of vesicular transport - the process of formation and transportation of membrane vesicles (vesicles) between cells: “Nobel Prize in Physiology or Medicine (2013): vesicular transport” [8]. - Ed.
The study of impaired synaptic transmission in HD was the topic of our study. Could it be that the malfunctioning of striatal neurons in the early stages of HD is caused by the fact that they do not “hear” the commands of cortical neurons? Can weakening of synaptic connections lead to irreversible changes in striatal neurons and lead to their death? What we learned while searching for answers to these questions is described below.
Diagnosis of Huntington's chorea
When diagnosing Huntington's chorea, the doctor primarily relies on family history, physical examination, and analysis of the patient's neurological condition. If suspected, laboratory and instrumental examinations are prescribed, without which a diagnosis cannot be made.
The main types of examinations for diagnosing Huntington's chorea:
- genetic research, DNA test;
- electroencephalography;
- computed tomography (CT) of the brain;
- magnetic resonance imaging (MRI);
- positron emission tomography (PET);
- blood chemistry;
- intrauterine genetic testing of the fetus.
Research Findings: Changes in Synaptic Transmission in Huntington's Disease
Synaptic transmission can be studied in various ways. For example, this can be done by penetrating the neural circuit using electrophysiological methods. A neuron expresses its activity using an electrical current that can be measured. If an experimenter takes a chain of two neurons and, after activating one neuron, records the electrical activity of the second, he can find out how well the signal travels. Another way to study the functioning of synaptic transmission is to study the morphology of the neuron. The fact is that many neurons (including neurons of the cortex and striatum) have special membrane outgrowths - spines, which they need specifically for the formation of synapses (Fig. 2). The more actively a neuron “communicates” with its neighbors, the more spines there are on its surface. Taking these two approaches, we decided to investigate how synaptic transmission works in HD.
Figure 2. Dendritic spines on the surface of a striatal neuron. Spines are small projections on the surface of neuronal processes; in the enlarged image they are marked with arrows.
photo of the author of the article
Figure 3. Neuronal culture from cortical and striatal neurons. Using specific antibodies, cortical neurons are colored red, and striatal neurons are colored yellow-green.
photo of the author of the article
As a model for studying Huntington's disease, a cell culture from neurons of the cortex and striatum was used. To prepare the culture, immature neurons from the studied areas of the mouse brain are planted in Petri dishes, where they form full-fledged neuronal processes and neural chains (Fig. 3). Wild-type mice (without mutations) and YAC128 mice, which carry a mutation in the huntingtin protein gene and are a recognized model of HD, were used. On days 14–15 after neurons are planted in a Petri dish, they reach a mature state corresponding to the state of neurons in the adult brain, and on days 19–20 neurons are considered “old”: they exhibit a number of cellular processes characteristic of the brain of elderly people. In addition, with age, mutant huntingtin protein and its aggregates accumulate in neurons of YAC128 mice, so studying neuronal culture at these two stages provides insight into what is happening in the brain of a patient with HD at the early and late stages of the disease.
Figure 4. Different types of spines on the surface of a dendrite - micrograph and schematic representation.
To begin with, we examined the morphological differences between the two lineages, i.e. compared their appearance. Normal striatal neurons are characterized by the presence of a large number of spines, which is why they are called medium spiny neurons (MSNs). It is the spines that form the majority of synaptic contacts between neurons of the striatum and cortex, and the presence of a certain number of them is important for normal synaptic transmission. The “quality” of spines is also important: in modern neurobiology they are divided into three groups according to size and shape (Fig. 4): mushroom-shaped, thin and stump-shaped. At the same time, different types of spines perform different functions: it is believed that only mushroom-shaped spines form active synapses, while thin and stump spines do not form contacts with other neurons. Thus, for the normal functioning of the neural chain and the effective transmission of information along it, the presence of a certain number of mushroom-shaped spines is necessary.
In order to find out how many mushroom-shaped spines there should be on the SCN normally, a culture of neurons from the brain of wild-type mice was used as a control at all stages of the morphological analysis. It turned out that the number of spines on the SSN of the striatum on day 14 of culture (young neurons) is the same in YAC128 and wild-type cultures, but on day 20 (in “old” neurons) significant changes are observed (Fig. 5). In an “aged” YAC128 culture, the total number of spines decreases, and the relative number of mushroom-shaped spines that form active synapses decreases by half [10]. It turns out that morphological changes in neurons, indicating a violation of synaptic transmission, develop only in “old age” (at a late stage of the disease). This means that in the early stages the root of the problem must lie in another area.
Figure 5. Morphological analysis of striatal neurons. a — neuron spines on days 14 and 20 of culture. Micrographs show areas of neuron dendrites. The relative number of spines of different types is marked on the pie chart: green - mushroom-shaped spines, red - thin spines, black - thin spines. On the 20th day of cultivation, the proportion of mushroom-shaped spines on the surface of YAC128 neurons decreases and the proportion of stump spines increases. b — Dendritic spine density (average number of spines per 10-μm-long dendrite) on wild-type and YAC28 neurons.
Therefore, we compared the electrophysiological characteristics of the two lines. This is possible thanks to the electrical activity of neurons, which can be recorded using a special method called patch clamp. To do this, a thin glass pipette with an electrode inside is applied to the surface of the neuron. When a neuron is activated, the voltage on its cell membrane changes, and this change is recorded by an electrode. If you take two neurons connected by a synaptic contact and, exciting one, record the response electrical activation on the second, you can measure the efficiency of signal transmission through the synapse (Fig. 6). If response activation does not always occur, then synaptic transmission is likely weakened. This method can detect synapse dysfunction before changes in neuron morphology.
Figure 6. Experimental design using combined optogenetics and electrophysiological recording. The cortical neuron is activated when illuminated with blue light, and the response activity is recorded on the striatal neuron in contact with it using a glass pipette with an electrode.
To activate a neuron, you can use several methods. A chemical can be added to the surrounding fluid to open ion channels, causing the neuron to become electrically excited. You can stimulate a neuron with an electrical current. But for our experiments we chose a more subtle tool for influencing neurons, namely optogenetics. This approach is based on the introduction of special light-sensitive proteins - opsins - into neurons, as a result of which the neurons themselves become sensitive to light (Fig. 7). As a result, by illuminating neurons with light of a specific wavelength, their activity can be changed. Illumination with blue light excites the neuron, and with yellow light it causes inhibition (i.e., it suppresses the activity of the neuron).
Optogenetic technologies these days even promise to restore vision to people with degenerative retinal lesions, imparting light sensitivity not to destroyed photoreceptors, but to ganglion cells: “Optogenetics + holography = insight?” [eleven]. - Ed.
Figure 7. Opsins are light-sensitive proteins that enable the movement of ions across the cell membrane and changes in neuronal activity. Channelrhodopsin (ChR2) causes membrane depolarization and neuron activation, halorhodopsin (NpHR) causes membrane hyperpolarization and neuron inhibition.
Symptoms
The primary manifestation of the disease can occur at any age, but most often the first symptoms appear between the ages of 35 and 40 years. The main clinical sign in the early stages is chorea, which is manifested by uncontrolled and erratic movements. Initially, it develops as minor incoordination with sudden, uncontrollable movements. These movements can be both sudden and slow. Subsequently, these signs are accompanied by symptoms of speech impairment, problems with the process of swallowing and chewing. Due to constant twitching and impaired muscle tone, a person grimaces and has trouble sleeping.
The early stages are characterized by minor (or complete absence) personality and cognitive disorders. First, there is a violation of the functions of abstract thinking, which is accompanied by the inability to plan actions, carry them out, and adequately evaluate them. Then memory disorders and personality changes occur: the person becomes aggressive, self-centered, sexually disinhibited, the main types of addictions (alcoholism, gambling addiction) become stronger, obsessions and phobias appear.
Thus, all patients suffering from Huntington's disease have similar symptoms, the only differences being the type of onset of the disease, its progression and the degree of physical, mental and cognitive disorders.
Optogenetics
Optogenetics is a method that combines the approaches of genetics and optics for fine control of the electrical activity of electrically excitable cells (neurons and muscle fibers) [9]. To do this, genes of special light-sensitive proteins—microbial opsins, which are ion channels or pumps—are introduced into the cells under study (Fig. 7). The first work showing the possibility of controlling the electrical activity of neurons using opsin was published in 2005. Over the next few years, a number of experimental works appeared that made it possible to refine this technique and prove its applicability under various experimental conditions.
In recent years, many different opsins have been discovered, of which halorhodopsins and channelrhodopsins have found the most application in optogenetics. When the opsin gene is delivered using genetic engineering methods into a neuron, light-sensitive channels appear on the plasma membrane, and the cell itself becomes light-sensitive. When exposed to blue light, the channelrhodopsin pore opens (maximum absorption - 470 nm), which causes the movement of positively charged ions into the cell, ensuring depolarization of the neuron membrane and the generation of action potentials. When exposed to yellow light, halorhodopsin is activated (maximum absorption - 580 nm), the neuron membrane is hyperpolarized, causing inhibition of the neuron. The high temporal resolution of optogenetics allows for very fine regulation of synaptic events and is therefore an important tool for studying interneuronal connections.
The combined use of optogenetics and classical electrophysiology techniques allows us to benefit from the positive qualities of each of these approaches. The precision of electrophysiological recording is combined with the ability to use light stimuli of varying durations and intensities to help scientists study the workings of neural connections in detail.
The electrical activity of neurons is expressed in sharp voltage surges on the cell membrane and the resulting appearance of an electric current. These sudden jumps are called spikes or action potentials and last a few milliseconds (Figure 8). We found that the longer a neuron is illuminated with blue light, the more spikes it creates during this time. If the illuminated neuron is connected by a synaptic contact with another neuron, then response activity can be recorded on the second neuron, also in the form of individual spikes.
Figure 8. An example of a recording obtained from electrophysiological recording of neuron activity. Spikes (action potentials) are reflected in the recording as vertical lines showing sharp jumps in membrane current.
In our experiments, we used a pair of young (14 days) cortical and striatal neurons connected by synaptic contact. The cortical neuron was activated with blue light, and the response activity was recorded on the striatal neuron. It turned out that for a response to occur on a striatal neuron, a certain duration of illumination (activation threshold) is required. If the duration of illumination was below the threshold value, then a spike on a striatal neuron did not occur in response to every flash of light. And most importantly, the activation threshold for neurons from the brains of healthy mice was different from YAC128 mice (with a mutation in the huntingtin gene). This difference was most clearly visible at 50% activation of the striatal neuron, i.e. the duration of illumination at which a spike occurs in response to every second flash of light. The threshold for 50% activation of a striatal neuron in response to irradiation of a cortical neuron for the YAC 128 cell culture was approximately two times (more precisely 2.3 ± 0.8) higher compared to the positive control [10].
It turns out that a mutation in the huntingtin protein leads to the fact that synaptic transmission deteriorates even in young neurons, and the disturbances occur at the functional level (without morphological changes). Could it be that it is these functional disorders that subsequently lead to the appearance of morphological changes, such as the disappearance of spines in old striatal neurons?
To answer this question, we again turned to optogenetics for help, but now with its help we suppressed the activity of neurons with light (Fig. 9a). If our assumption is correct, then the temporary absence of the activating influence of the cortex should lead to the disappearance of spines on striatal neurons in the YAC128 culture. Indeed, after the experiment, the number of spines in the positive control remained unchanged, but in the YAC128 culture it decreased significantly (Fig. 9b, c). It turns out that neurons modeling HD are especially sensitive to weakening the activating influence of cortical neurons , therefore, long-term weakening of the synaptic connection between these neurons leads to a decrease in the number of spines on the 20th day of cultivation [10].
Figure 9. Influencing neurons using optogenetics. a — suppression of cortical neuron activity using optogenetics. When a neuron is illuminated with yellow light (orange stripe), it becomes inactive—there are almost no spikes in the electrophysiological recording during this period of time. b — influence of long-term optogenetic inhibition on the morphology of neurons. Micrographs show a decrease in the number of spines on the dendrite of the YAC128 neuron. c — change in the density of dendritic spines after optogenetic inhibition. In the wild-type culture, the number of spines does not change, but in the YAC128 culture, spine density is significantly reduced.
In summary, we found that in our HD model there is a disruption of synaptic transmission that develops in two stages. At an early stage (young neurons, on day 14 of neuron culture), a functional weakening of the synaptic connection occurs, which at a later stage (old neurons, on day 20 of culture) leads to morphological disturbances of synaptic contacts.
Diagnostics
Huntington's chorea rarely causes difficulties in diagnosis due to a whole series of its clinical manifestations. Typical symptoms, a detailed family history and molecular genetic testing can confirm or exclude the diagnosis with maximum accuracy.
Genetic testing is the only optimal and reliable option for diagnosing this pathology. The polymerase chain reaction will determine with extreme accuracy the number of copies of the CAG triplet in the gene.
Important ! However, there is still no clear opinion regarding its use. Testing is strongly discouraged for anyone under 18 years of age.
There are repeated cases of suicide among adolescents after confirmation of the disease.
Doctors place great emphasis on the fact that a positive test result does not necessarily mean the presence of the disease. Each carrier of the gene must realize that the first signs may appear several years later, and he has every chance to live the most fulfilling life possible.
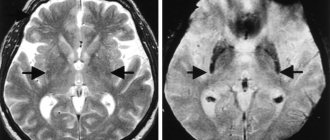
As additional methods, high-resolution computed tomography and MRI of the brain will help identify pathological changes in brain activity before the onset of the first symptoms.
Conclusion: synaptic transmission disorders and neurodegenerative diseases
The study confirmed our initial guess: disruption of the striatum in HD is associated primarily with disruption of synaptic transmission. The striatum neurons stop “hearing” the commands of the cortical neurons, and, as a result, the person begins to lose control over his movements. But at an early stage of the disease, these disorders are functional in nature and are probably reversible. If we find out the reasons leading to disruption of synapses, then it is possible to develop a drug that will help stop pathological changes, provide striatal neurons with the necessary level of activation and, thus, prevent the development of irreversible morphological disorders.
The results of this work also lead to another important conclusion: when studying neurodegenerative diseases, scientists should pay more attention to synaptic transmission and the interaction of neurons. We know quite a lot about how the accumulation of amyloid aggregates in Alzheimer's disease affects cell activity, and which neurons die during the development of Parkinson's disease, but this has still not led to the emergence of effective therapy. A possible reason for these failures is that we do not take into account the consequences of disruption of synaptic connections - those that we discovered in the study of Huntington's disease. We hope that our findings will point researchers in the direction of developing effective treatments for Huntington's disease, and Thirteen will finally be healthy!
The study was carried out in the laboratory of molecular neurodegeneration of St. Petersburg State Polytechnic University (head of the laboratory - Prof. Ilya Borisovich Bezprozvanny, University of Texas) under the guidance of Ph.D. Dmitry Nikolaevich Artamonov.
Classification
Extrapyramidal hyperkinesis is:
- Primary (for various neurodegenerative diseases, for example, Huntington's disease , neuroacanthocytosis , spinocerebellar ataxia ).
- Secondary (a symptom of autoimmune, vascular and metabolic diseases, heavy metal intoxication, encephalitis of various etiologies).
According to their prevalence, choreic hyperkinesis is divided into:
- Focal.
- One-sided.
- Generalized.
Huntington's chorea, what is it? This disease is associated with the destruction of neurons in the subcortical nuclei and cortex. The disease manifests itself as a combination of movement disorders, dementia and progressive cognitive impairment. Since chorea is not the only manifestation of the disease, the term "Huntington's disease" is more correct than the term "chorea". The disease appears at the age of 40-50 and affects both sexes equally. The main manifestations of the disease are steadily progressing.
Photos of symptoms
Already at an early stage of Huntington's disease, in addition to motor disorders, a pronounced speech disorder (slow arrhythmic speech) appears; a swallowing disorder appears in the later stages and becomes the cause of aspiration , asphyxia and pneumonia . Changes in the mental sphere are represented by impaired memory, attention, phobic disorders and depression with suicidal attempts.
Among the secondary forms, minor chorea (synonymous with Sydenham's chorea), which is a complication of rheumatism, . This is a generally recognized variant of rheumatic lesions of the nervous system, which is why rheumatic chorea is also called neurorheumatism . The first descriptions of an epidemic of rheumatic chorea were made in 1418, and a complete description of the disease was given by Sydenham 200 years later. In 1831, Bright established a connection between minor chorea and rheumatic fever and described severe forms of pseudoparalytic minor chorea.
In recent years, thanks to antirheumatic treatment, Sydenham's chorea is very rare, and rheumatism itself is considered by rheumatologists as a disease that is losing its relevance. In the early 80s, neurorheumatism (St. Vitus' dance) was diagnosed in 36% of children with rheumatism, and currently in 16% of patients. In this case, hemichorea (hyperkinesis of one side) and muscle hypotonia (moderate and severe), impaired coordination, handwriting and speech, increased tendon reflexes and emotional lability predominate.
Treatment of Huntington's disease
Once Huntington's disease is diagnosed, it is advisable for the patient to complete advance directives in the event of disability as soon as possible. In these instructions, the patient can explain what type of care he would like to receive at the end of his life.
Huntington's disease has no cure. However, some medications, including antipsychotics (such as chlorpromazine, haloperidol, risperidone, and olanzapine) and dopamine-reducing drugs (such as tetrabenazine and the high blood pressure drug reserpine), may help relieve symptoms such as abnormal movements and restlessness. .
If you have depression, antidepressants can be used.
Causes of Huntington's disease
The disease is inherited as an autosomal dominant trait. Human traits, including classical genetic diseases, are the product of the interaction of two genes, one passed on from the father and the other from the mother.
In dominant disorders, one copy of the disease gene (obtained from the mother or father) will be expressed as “dominant” over the other normal gene and result in the disease. The risk of passing the disorder from the affected parent to the offspring is 50% in each pregnancy, regardless of the sex of the child.
Huntington's chorea is caused by changes (mutations) in a gene located on the short arm (p) of chromosome 4 (4p16.3). Chromosomes are found in the nucleus of all cells in the body. They carry the genetic characteristics of every person. Pairs of human chromosomes are numbered 1 to 22, with an unequal 23rd pair of X and Y chromosomes for males and two X chromosomes for females. Each chromosome has a short arm (arm), designated by the letter "p", and a long arm, designated by the letter "q". The chromosomes are further divided into numbered bands.
This gene, known as HTT, controls the production of the protein Huntingtin, found in nerve cells (neurons) throughout the brain. However, the specific function of the protein is unknown. In patients, the HTT gene contains errors in the encoded “building blocks” that carry its specific genetic instructions.
The instructions in each gene consist of different patterns of four basic chemicals (nucleotide bases) called adenine (A), cytosine (C), guanine (G) and thymine (T). In people with the disease, the HTT gene contains abnormally long repeats of cytosine-adenine-guanine encoded instructions (trinucleotide CAG (CAG) repeat expansions). For example, people with the disorder have more than 35 CAG repeats in the HTT gene, with most having more than 39. However, people without the disorder have about 20 repeats in the gene.
The specific symptoms associated with Huntington's disease are caused by degenerative changes in nerve cells (neurons) in certain areas of the brain, including the basal ganglia and cerebral cortex. The basal ganglia are specialized nerve cells deep in the brain that play a role in regulating movement. The cerebral cortex, the outer region of the brain, is responsible for conscious thought and movement.
Disorders with similar symptoms
Symptoms of the following disorders may be similar to those of Huntington's chorea. Comparisons can be useful for differential diagnosis:
- Hallervorden-Spatz disease is a rare, progressive disease that affects muscle movement. The disorder is associated with degeneration of the nervous system. Hallervorden-Spatz disease is characterized by uncontrolled muscle movements (dystonia), muscle rigidity and loss of cognitive abilities (dementia). Symptoms of the disease usually begin in childhood, although sometimes the disease begins in adulthood.
- Multiple system atrophy (MSA) is a group of rare inherited diseases characterized by progressive degeneration of the cerebellar cortex and other brain tissues. Several different types of systemic atrophy have been identified, with symptoms varying widely depending on the type of MSA. Typically, these disorders are characterized by impaired ability to coordinate muscle movements, tremors, involuntary muscle jerks, speech impairment (dysphasia), loss of cognitive abilities and mental deterioration.
- Rheumatic chorea (Sydenham's chorea) is a nervous system disorder that occurs suddenly after a streptococcal infection, such as scarlet fever, pharyngitis or rheumatic fever. The disorder usually affects young children and teenagers. Sydenham's chorea is characterized by rapid, involuntary, non-repetitive muscle movements that may gradually become more severe and frequent. The muscles of the arms and legs are most severely affected. Speech may also be impaired. Other common symptoms may include a clumsy gait. Chore-like muscle movements tend to disappear with sleep. The disorder usually resolves in 3-6 months without permanent neurological or muscle damage.
- Wilson's disease is a rare genetic disorder characterized by excess copper in various tissues of the body, especially the liver, brain and corneas of the eyes. The disease is progressive and, if left untreated, can cause liver disease, central nervous system dysfunction, and death.
- Tourette syndrome is a neurological movement disorder that usually first appears between the ages of 2 and 16 years. Initial symptoms are often rapid eye blinking (nystagmus) or facial tics. Tourette syndrome is not a progressive or degenerative disease, and patients live a normal life expectancy.
Modern methods of treatment
“Treatment of Huntington’s disease,” explains neurologist Valentina Kuzmina, “is exclusively symptomatic.
To reduce hyperkinesis, antipsychotics and myospasmolytics are used, both in tablets and injectables. To reduce the akinetic-rigid form of the disease, antiparkinsonian drugs are used. For depression, tricyclic antidepressants and selective serotonin reuptake inhibitors are prescribed. For outbursts of aggression - antipsychotics. Rehabilitation will help expand the functional abilities of patients.
Improving the functional capabilities and social adaptation of such patients is a priority task for the doctor.