Risk factors for strokes
- Diseases of the cardiovascular system: atrial fibrillation, heart failure, hypertension, arrhythmia, tendency to form blood clots, etc.
- Regular stress, chronic fatigue, overexertion.
- Age over 45 years for men and over 50 years for women.
- Migraine.
- Alcohol abuse, drug addiction, smoking.
- Metabolic disease.
- Diabetes.
- Excess body weight, sedentary lifestyle, unhealthy diet: eating fatty, spicy, fried, smoked foods.
- Long-term (more than 5 years) use of hormonal drugs.
- Heredity.
- Infectious and inflammatory processes (systemic lupus erythematosus, etc.).
- Gender: The risk of stroke is higher in men than in women.
These factors lead to a decrease in the elasticity of blood vessels, increased load on them, the formation of atherosclerotic plaques, and an increase in the amount of sugar and bad cholesterol in the blood.
Patients at risk should regularly check their health with a doctor, undergo a CT scan or MRI of the brain, conduct a study of the cerebral cortex, take a blood test for sugar and cholesterol levels, blood clotting, etc.
St. Petersburg State Budgetary Healthcare Institution "Nikolaevskaya Hospital"
July 19, 2019
What is a stroke
Effective prevention of cerebral stroke is impossible without knowledge of the causes of the development of this disease.
A stroke is a serious (acute) problem with blood circulation in the brain. The cause may be a rupture of some, not necessarily large, vessel - this type of stroke is called hemorrhagic. Or a blood clot that blocks the flow of blood is a stroke, respectively, an ischemic stroke.
Depending on which part of the brain was damaged, the neurological functions for which it was responsible suffer. Someone loses their speech. Someone is paralyzed - partially or completely. Some people have breathing problems. Some people even die.
Stroke statistics are disappointing: 31% of patients who have suffered a stroke require special care, 20% cannot walk independently, and only 8% return to normal life after long rehabilitation. But the worst part is that stroke is difficult to predict. It’s not for nothing that it’s called a stroke: an acute brain disorder develops suddenly and quickly. Often literally out of nowhere: just now the person was laughing and joking, and now they call him an ambulance.
Who's at risk
Some people are more vulnerable to developing a stroke than others. And most often these are those who:
Suffering from hypertension. This is the most common cause of strokes.
Has some kind of heart disease (for example, heart failure or arrhythmia).
Suffering from diabetes. Diabetes damages blood vessels, including those of the brain, increasing the risk of hemorrhages.
Is overweight.
Takes certain medications. Dangerous medications include those that alter estrogen levels. For example, birth control pills.
Leads a sedentary lifestyle.
Has high blood cholesterol levels.
Smokes.
Suffering from sleep apnea.
Over 55 years old. According to statistics, every decade after age 55, the risk of having a stroke doubles.
Has a family history of strokes: one of his close relatives became victims of a stroke.
Is a man. Women have a significantly lower risk of stroke.
If at least a few points can be attributed to you, you need to take care of yourself. Preferably today.
What to do to prevent stroke
Stroke prevention comes down primarily to lifestyle modifications. Here's what, according to experts from a reputable research organization, should be done first:
- Control your blood pressure People suffering from arterial hypertension are especially likely to suffer from strokes. It is they who experience brain hemorrhages (hemorrhagic strokes). Moreover, two scenarios are possible: either one of the brain vessels ruptures, or blood leaks through its wall into the surrounding tissue for some time. In any case, high blood pressure (or pressure surges) plays a major role in this process. And for a hypertensive patient, it is very important to keep the situation under control and regularly take medications prescribed by a doctor to help maintain blood pressure at an optimal level - no more than 130/80 mmHg.
- Control your cholesterol levels Most strokes occur due to narrowing or complete blockage of the arteries in the brain (ischemic stroke). The cause is cholesterol plaques deposited on the walls of blood vessels. To minimize the likelihood of disease, it is necessary to adhere to a diet that involves limiting fat intake. It should be borne in mind that not all fats are harmful to the body (for example, polyunsaturated omega-3 and omega-6 fatty acids are very beneficial).
- Control your blood sugar levels According to statistics, the presence of diabetes increases the risk of stroke by 2.5 times. This is not surprising: diabetics often experience heart failure, excess weight and poor condition of the walls of blood vessels. In addition, when carbohydrate metabolism is disturbed, the rate of removal of water from the body increases, which increases the thickness of the blood. To avoid the development of a stroke, it is necessary to monitor your diet, limit the consumption of fast carbohydrates and monitor blood glucose levels by periodically taking appropriate tests.
- Watch your weight Excess weight brings with it several factors that increase the risk of stroke. This includes an increase in blood pressure, cardiovascular diseases, and the possible development of diabetes. Losing even 4-5 extra pounds will greatly improve your chances of avoiding a stroke.
- Eat more vegetables and fruits At least 4-5 servings (apple, coleslaw, grilled vegetables, etc.) per day. Plant foods lower blood pressure and improve vascular elasticity. And this, in turn, is an excellent stroke prevention.
- Quit smoking And also visit smoking rooms for company. Passive smoking, like active smoking, has a destructive effect on blood vessels.
- Exercise regularly Physical activity reduces the risk of developing all types of stroke. Aerobic training is especially good: walking, running, swimming, cycling, low-impact fitness. The exercises work comprehensively. They help reduce weight, improve the overall condition of blood vessels and the heart, and reduce stress. Try to increase the duration of your daily workouts to at least 30 minutes.
- Manage stress At the moment of nervous tension, a large amount of adrenaline is released into the bloodstream. Glucose levels rise sharply, the heart begins to work more actively, and blood pressure rises. There is a simultaneous load on the vessels, which can lead to a stroke. Of course, it is impossible to completely eliminate stress from life, but it is worth learning to control your reaction to stressful situations. People prone to nervousness may need to consult a doctor - he will recommend sedatives.
- Get an annual medical examination. A timely visit to the doctor will help to identify health problems in time and begin treatment on time. Unfortunately, it is impossible to reduce the risk of stroke to zero. Therefore, in addition to preventive measures, it is important to know what a stroke looks like and what to do if it happens to you or someone around you. Doctors have several hours to save a person. Everyone needs to know the symptoms of a stroke in order to recognize the disease in time.
Stroke is the second (after coronary heart disease) cause of death in Russia. A fifth of patients become severely disabled after a stroke. But many consequences can be prevented if you call a doctor in time.
The first 3-6 hours after a stroke are the “therapeutic window” - the time during which medical care is most effective. Sometimes a person does not immediately notice that something is wrong with him, or thinks that the ailment will go away on its own. Because of this, valuable time is lost. Therefore, it is important to know what a stroke looks like and what to do if it occurs.
Main signs of stroke
1. A sudden and severe headache begins.
2. The man loses consciousness.
3. Balance is disturbed, gait becomes unsteady.
4. Part of the body on one side, for example, half of the face, goes numb.
5. Speech problems appear: it is difficult to pronounce words.
6. Vision is lost in one eye or in both eyes at once.
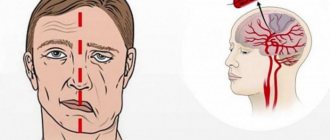
How to understand for sure that it is a stroke
Ask the person to do a few simple steps:
- Smile. If a person cannot smile or the smile comes out one-sided (and this was not the case before), sound the alarm.
- Speak. Ask the person to repeat a simple sentence after you or recite a poem. After a stroke, articulation is impaired and speech becomes slurred.
- Stick out tongue. If a person cannot do this, if the tongue involuntarily tilts to one side or looks askew, then this is a stroke.
- Raise both arms evenly. With a stroke, a person will not be able to control both hands equally well.
— Raise your hands in front of you and close your eyes. If one arm falls involuntarily, this is a sign of a stroke.
— Write an SMS. Researchers at Henry Ford Hospital noticed that patients who had no other signs of stroke were unable to type a coherent message, instead writing a nonsensical string of words without noticing it.
If a person has failed at least one of the tasks, this is enough to act immediately.
What to do if a person has a stroke
First, call an ambulance. Be sure to describe why you suspect a stroke: the headache began suddenly, the person lost consciousness or balance. Tell us what the patient cannot do: cannot smile, cannot raise both hands, cannot pronounce words.
If you have a stroke, you need professional help as quickly as possible.
After calling an ambulance, place the person on pillows, the elevation should start from the shoulder blades. Provide access to fresh air: open a window or door in the room, unfasten tight clothing.
Do not give water or food because organ functions may be impaired and the person may have difficulty swallowing.
If possible, measure your blood pressure. If it is elevated, give the person the blood pressure lowering drug that he usually takes. If there is no such pill, do not give anything.
Be healthy!
- Share:
- Livejournal
- Blogs@Mail.ru
- LiveInternet
- MySpace
Print page
Primary prevention
About 80% of all strokes are primary. Basic preventive measures:
- Lifestyle changes. The patient must give up bad habits and a sedentary lifestyle, and start eating right. The diet should consist mainly of steamed, boiled and stewed dishes, low-fat dairy products, and fish. Be sure to drink about 8 glasses of water. Physical training should be age-appropriate; sometimes it is enough to add walking. Diet and moderate exercise will help normalize weight and improve health. It is equally important to eliminate or minimize stress, overexertion, and sleep 8 hours a day.
- Blood pressure control. Normal values are 120-140 mmHg. Art. for the upper and no more than 80-90 mm Hg. Art. for the bottom. The change must be made at the same time every day. If your readings increase, you should consult a doctor, he will select treatment and prescribe medications to stabilize your blood pressure.
- Controlling blood sugar and bad cholesterol levels.
- Taking medications , such as antithrombotic drugs.
Stroke: will it happen or won't it?
The basis of secondary prevention is the identification of risk factors. If everything is relatively simple with a disease such as hypertension, then many other diseases may not make themselves felt for a long time and may not be detected during routine tests.
For example, atrial fibrillation, the most dangerous risk factor, if it is of an attack-like (paroxysmal) nature, cannot be detected on a regular ECG outside of an attack. Even daily ECG monitoring does not always allow it to be recorded. Currently, many experts recommend that patients who have suffered an ischemic stroke undergo ECG monitoring for 2-3 days. According to various sources, this makes it possible to detect paroxysm 15-20% more often - that is, to identify the cause of a stroke, which was not previously known, and perhaps even denied.
The same applies to atherosclerotic plaques. On one “vascular ultrasound” the specialist sees the plaque, on the other – not. Their sizes and assessment of the influence of blood flow vary. In some cases, to clarify the diagnosis, it is necessary to do angiography using computed tomography ().
It is not for nothing that the standards of medical care used in state medical institutions are called “medical and economic standards.” The volume of research conducted on them is reduced to the very minimum optimum. No matter how rude or sad it sounds, in the vast majority of cases it is dangerous and stupid to rely on this “conveyor belt” and think that everything is fine. Often everything turns out not to be good at all, a stroke happens again, but it’s too late. This does not mean that “the treatment there is bad” or “the doctors work bad”; it does not mean at all that you should refuse hospitalization and a visit to the doctor if there are signs of a stroke. Vice versa! Each medical organization and each doctor in it works according to the available capabilities, which in most cases are very limited, and it is pointless to expect more in this situation.
But it is worth remembering that the treatment and rehabilitation of a patient who has suffered a stroke is much more expensive in all respects - time, financial, psycho-emotional - than prevention and timely competent treatment. Indeed, in this case, the stingy person risks paying not only twice, but also a generally unacceptable price - life. That is why in our clinic we use an individual approach to the patient, choosing the optimal scope of examination for each case and methods of preventing such a terrible disease as stroke!
Secondary prevention
The main task of secondary prevention is to reduce the likelihood of developing a recurrent stroke to a minimum. Basic measures:
- Regular monitoring of blood pressure and reducing it to normal levels if necessary.
- Changing your diet: it is important to reduce the amount of salt consumed, eat more vegetables and fruits, low-fat dairy products, eliminate fatty, fried and smoked foods, and alcohol.
- Normalize weight, exercise for at least half an hour every two days.
- Drug therapy especially for patients with signs of atherosclerosis and patients who have experienced ischemic stroke or transient ischemic attacks. Medicines help lower cholesterol and blood pressure, cope with inflammatory diseases and exacerbations of chronic diseases.
- Regular visits to a neurologist. The doctor can monitor changes in the patient’s condition, adjust therapy, prescribe medications or procedures, and give recommendations regarding hospitalization.
Main symptoms and signs of stroke
It is important to know that when the first symptoms of a stroke appear, you should urgently call an ambulance. The main features are:
- a sharp feeling of weakness;
- feeling of numbness in the limbs, weakness;
- speech impairment (“porridge in the mouth”) and blurred vision;
- dizziness and headache;
- nausea, vomiting;
- impaired coordination and balance.
Sometimes the behavior of a person who has had a stroke outwardly resembles the behavior of a drunk. To recognize pathology, pay attention:
- on speech (it will be incoherent and difficult);
- on a smile (asymmetrically located corners of the lips - the first sign of a stroke);
- on hand movements (the handshake will be weak, hands raised up will lower spontaneously).
Call an ambulance immediately at the first suspicion of a stroke. The body cannot cope with the disease on its own.
Prevention of ischemic stroke
Measures to prevent ischemic stroke, in addition to those listed above, include drug therapy. All medications must be prescribed by a doctor. Typically these medications are:
- preventing the formation of blood clots;
- lowering cholesterol levels;
- increasing the tone of blood vessels and strengthening their walls;
- activating metabolism in the brain;
- having a calming effect.
If you or your family have experienced a stroke, take care of your health and contact. Rehabilitation after a stroke will allow you to recover and reduce the risk of developing a recurrent vascular accident.
Possible consequences
A stroke can result in temporary disability, disability, or even death. Only 20% of people who have had this disease can fully return to work. Every year in Russia, stroke occurs in about 450,000 people. According to statistics of recorded deaths from stroke, this cause ranks second among all deaths in our country. The most common consequences of the disease include:
- impaired movement, weakness in the limbs, numbness of various parts of the body;
- memory, speech, and urination disorders;
- loss of ability to care for oneself independently.
Anticoagulant therapy
It has been established that in more than 67% of cases, strokes develop against the background of cardiac pathology; and about 15% occur against the background of chronic atrial fibrillation.
A breakthrough in the secondary prevention of IS in patients with atrial fibrillation was the use of vitamin K epoxide reductase inhibitors (warfarin, dicumarol, acenocoumarol, phenindione), which reduced the incidence of recurrent strokes in atrial fibrillation from 12 to 4%. The mechanism of action of drugs in this group is the suppression of vitamin K-dependent synthesis of biologically active forms of blood coagulation factors II, VII, IX and X. Doses of drugs that ensure maximum effectiveness of oral anticoagulant therapy largely depend on the individual sensitivity of the patient, and therefore A prothrombin test and international normalized ratio (INR) are used to monitor therapy.
It must be emphasized that therapy with oral anticoagulants after non-cardioembolic ischemic stroke is not more effective than therapy with antiplatelet agents (acetylsalicylic acid - ASA), but leads to a greater number of bleedings [7, 32, 41. However, drugs in this group (with achieving the target INR level of 2 ,0–3.0) are the drugs of choice for the secondary prevention of cardioembolic stroke (in patients with non-valvular atrial fibrillation in both permanent and paroxysmal forms), as well as in most other conditions accompanied by cardiac embolism.
The advantages of warfarin over antiplatelet therapy in the secondary prevention of IS are most clearly demonstrated in the EAFT and ACTIVE W studies.
The EAFT (European Atrial Fibrillation Trial) study included 455 patients with non-rheumatic atrial fibrillation who had suffered a minor IS or TIA within 3 months before inclusion in the study. As the primary endpoint, the study analyzed the incidence of vascular death, nonfatal stroke, nonfatal myocardial infarction, and systemic (noncerebral) thromboembolic episodes recorded at least once every 4 months. Patients were prescribed an open-label oral anticoagulant (the drug was chosen by the attending physician) until an INR of 2.5–4.0 was achieved, or using a double-blind method—ASA (300 mg/day) or placebo. The rate of reaching the end point was 8% per year for patients receiving oral anticoagulants, 17% in the control group. Thus, indirect anticoagulant therapy is more effective than ASA therapy as secondary prevention of thromboembolic episodes in patients who have suffered an IS or TIA [21].
The ACTIVE W (Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events) study analyzed the effectiveness of warfarin therapy (up to an INR of 2.0–3.0) compared with combined antiplatelet therapy ASA (75–100 mg/day) and clopidogrel (75 mg/day). The study included 6702 patients with atrial fibrillation and one or more risk factors for stroke (age 75 years and older; hypertension; previous IS or TIA; decrease in left ventricular ejection fraction below 45%; peripheral atherosclerosis; coronary artery disease or diabetes in people 55– 74 years old). The primary endpoint was the incidence of IS, non-cerebral thromboembolic events, MI and vascular death. The safety criterion was the incidence of hemorrhagic complications. The study was interrupted in September 2005 due to evidence of superiority of warfarin over combination antiplatelet therapy: 5.64% of patients receiving antiplatelet therapy and 3.94% of patients receiving warfarin reached the end point (p = 0.0002). It should be noted that more than 3/4 of the patients were initially treated with warfarin. The risk of hemorrhagic complications in the study groups did not differ and amounted to 2.4 and 2.2% per year (p = 0.67) in the groups of combined antiplatelet and anticoagulant therapy [6].
However, despite the convincing evidence base, the use of warfarin and other drugs in this group is associated with a number of clinical problems, such as genetically determined resistance to therapy, variability of the anticoagulant effect depending on the diet and concomitant therapy, as well as the need for monthly INR monitoring, which is not always done by patients.
Recent years have been marked by the emergence of several drugs whose anticoagulant effect does not require laboratory monitoring. The drugs dabigatran, a direct thrombin inhibitor, and rivaroxaban, a selective and reversible inhibitor of factor Xa, have proven their effectiveness in the primary and secondary prevention of stroke due to atrial fibrillation, comparable to warfarin, and well tolerated in the RELY [17] and ROCKET AF studies [33 ] respectively.
Anticoagulant therapy after cardioembolic stroke must be carried out for a long time or for at least 3 months after IS that occurred against the background of acute MI [44]. There are conflicting opinions about when anticoagulant therapy should be started. After a TIA or minor stroke, therapy (with warfarin, dabigatran or rivaroxaban) should begin immediately, but in the case of a severe stroke with signs of extensive infarction, according to neuroimaging methods (for example, when the lesion size is more than a third of the blood supply of the middle cerebral artery), anticoagulant therapy is necessary start in a few weeks (the issue must be resolved individually in each case).
Patients with atrial fibrillation and stable coronary artery disease should not combine oral anticoagulants with ASA [26]. Anticoagulant therapy may be preferable for patients with aortic atheroma [20], fusiform basilar artery aneurysm [22], or cervical arterial dissection [24].
Today, according to evidence-based medicine, the use of oral anticoagulants for the purpose of secondary prevention is recommended for patients with atrial fibrillation who have had a stroke, as well as for patients with verified cardioembolic origin of stroke. Moreover, if warfarin is used as an oral anticoagulant, the target INR level is 2.0–3.0 [28, 29]. When using rivaroxaban or dabigatran, INR monitoring is not required.
1.General information
Acute cerebrovascular accidents (ACVA) to this day remain one of the most acute and complex problems of neurology. Along with cardiovascular and oncological diseases, strokes occupy the top positions both in the statistics of the causes of medical mortality and in the lists of the most common causes of disability.
The term “cerebral stroke” in modern medicine has almost been replaced by a more general definition of stroke. A stroke is the mass death of cells in the cerebral cortex due to hemorrhage (hemorrhagic stroke) or a sharp reduction in blood supply to any area (ischemic stroke; it occurs much more often than hemorrhagic, so we will talk below mainly about ischemic strokes). One of the main diagnostic criteria for a stroke is the presence of persistent or irreversible impairment of any functions that are normally controlled by the affected area of the brain, for example, speech, memory, tone of any muscle group, etc. This is the difference between a stroke and acute cerebrovascular accidents in general: strokes, with all their danger, can be transient, transient, not leaving behind gross functional decline or complete failure, while a stroke is always catastrophic to one degree or another.
A must read! Help with treatment and hospitalization!