24.11.2016
Pinchuk Elena Anatolyevna
Deputy chief physician for medical work, kmn, neurologist, doctor of physical and rehabilitation medicine
Belkin Vladimir Andreevich
Head of the Department of Early Medical Rehabilitation, Physician of Physical and Rehabilitation Medicine, Neurologist
Lipovka Nadezhda Sergeevna
Head of the Department of Medical Rehabilitation, Physician of Physical and Rehabilitation Medicine, Neurologist
Sobolev Arkady Igorevich
Doctor of physical and rehabilitation medicine, neurologist
Ischemic stroke has several stages of progression. The first stage is an acute period of ischemic stroke, which lasts up to the 21st day. During the first 3-5 days, perifocal cerebral edema develops, karyoplasmic and cytoplasmic cells shrink.
An important point in the acute period of ischemic stroke is to correctly diagnose. First of all, it is necessary to distinguish any other diseases of the nervous system from a stroke. Next, the nature of the stroke itself is determined, and what caused it (hemorrhage in the cerebral cortex or blood clot). At the last stage of diagnosis, the localization of the lesion is determined, as well as the pathogenesis of cerebral infarction during stroke.
Stages of diagnostics of the acute period
- Stage 1. The victim is urgently hospitalized. The doctor receives basic information from the words of the patient, his relatives or surrounding people. External signs of cerebral circulatory disorders, emotional background, physical stress, and blood pressure levels allow a diagnosis to be made fairly quickly and accurately. The patient's medical history is studied for the presence of other diseases that can provoke the development of ischemic stroke (arrhythmia, atherosclerosis, previous heart attack, etc.). However, the possibility of making an incorrect diagnosis exists in the case of an epileptic seizure, a brain tumor, a head injury, a hypoglycemic state, etc.
- Stage 2. The most important point of this stage is to quickly and accurately determine the nature of the disease. The tactics of first aid and further treatment will depend on this. A computed tomography scan of the brain is performed, since the clinical picture alone cannot provide completely reliable information.
- Stage 3. After a quick history has been collected, the clinical picture has been identified and a CT scan has been performed, the doctor begins to choose treatment tactics. The subtype of stroke is also determined (lacunar, atherothrombotic or cardioembolic, etc.). The correct choice of therapy will help not only provide timely assistance to the victim, including surgery, but also prevent a possible recurrence of a heart attack in the future.
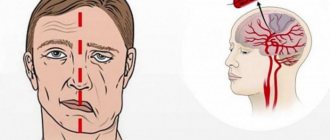
Strokes
Stroke (brain stroke) is a group of diseases caused by acute vascular pathology of the brain, characterized by the sudden disappearance or impairment of brain functions, lasting more than 24 hours or leading to death. A stroke is not a one-time event, but a process that develops in time and space - from minor functional changes to irreversible structural damage to the brain - necrosis.
Depending on the mechanism of development of acute vascular pathology of the brain, several types of stroke are distinguished:
· Most often (up to 80% of all cases), the disease develops as a result of an acute disruption of blood flow to a certain area of the brain (so-called ischemic stroke or cerebral infarction). · If brain pathology is caused by blood soaking a part of the brain, then this is a hemorrhagic stroke, or intracerebral hematoma (about 10% of all cases). · About 5% are subarachnoid hemorrhages that occur when the vessels of the meninges rupture. · The cause of the remaining 5% of strokes remains unclear.
For diagnosing a stroke, symptoms of impairment or loss of brain function are of paramount importance, often regardless of whether or not signs of a stroke are detected on a CT scan.
Prevalence and medical and social significance
According to the World Health Organization (WHO), stroke ranks third, after heart disease and cancer, among the causes of death in the adult population of the planet. Its average incidence in developed countries is about 2500 cases per 1 million population per year, while for transient ischemic attack the mentioned figure is about 500 cases. The risk of stroke is especially high in patients over 55 years of age. With each subsequent decade, their likelihood of developing a stroke almost doubles. Stroke is one of the main causes of disability in the adult population, since even in the case of timely provision of qualified medical care, a stroke patient experiences incomplete restoration of the functions lost during the acute period of the disease. Thus, according to the World Health Organization, more than 62% of stroke patients continue to have varying degrees of movement disorders, coordination disorders, sensitivity, speech, intelligence, and memory. In addition, after an ischemic stroke, there remains a fairly high probability of its recurrence, especially during the first year (about 10%). With each subsequent year of life, the risk of another stroke increases by 5-8%.
Risk factors for ischemic and hemorrhagic stroke
| Ischemic stroke | Hemorrhagic stroke |
| · elderly (80 years and older) age · male gender (in patients 50-80 years old) · arterial hypertension and often accompanying excess consumption of table salt · diabetes mellitus · transient ischemic attack · obesity and closely related overeating, low physical activity · coronary heart disease (especially in combination with hypercholesterolemia · heart rhythm disturbances (atrial fibrillation, sick sinus syndrome), regardless of the cause · heart failure, regardless of the cause · narrowing (congenital or acquired - atherosclerosis) of the arteries supplying blood to the brain · local expansion in the form of a sac (aneurysm) of the abdominal aorta · smoking · alcohol abuse · stroke in first-degree relatives · regular hypothermia | · caused by various reasons, changes in the natural structure of the vessels that supply blood to the brain · long-term constant or periodic increase in pressure in the vessels of the brain (arterial hypertension, migraine) · changes in the blood coagulation system due to taking blood thinning drugs (anticoagulants, antiplatelet agents, thrombolytics), blood diseases (hemophilia, thrombocytopenia, leukemia) · brain tumors · excessive alcohol intake · psychostimulant use (amphetamines, cocaine, etc.) · autoimmune inflammatory diseases of the cerebral vessels (vasculitis) |
Causes
About half of all cases of ischemic stroke are caused by atherosclerotic lesions of the carotid, vertebral and intracerebral arteries. Other causes include narrowing or blockage of smaller intracerebral arteries (arterioles) due to heart disease (see risk factors), blockage by a blood clot (thrombus), or thromboembolism of intracerebral vessels. As for hemorrhagic stroke, about half of all cases are caused by arterial hypertension. Pathology of the wall of intracerebral arteries, tumors and taking medications that thin the blood cause the development of hemorrhagic stroke in approximately equal proportions (10% each).
Clinical manifestations of acute cerebrovascular accident (ACVA).
ACVA includes transient cerebrovascular accidents (TCI) and stroke. PNMK – characterized by the sudden onset of focal (motor, speech, sensory, coordination, visual, etc.) and/or cerebral syndromes (headache, dizziness, nausea, vomiting, etc.) that develop in a patient with a general vascular disease (arterial hypertension , cardiac ischemia). PNMK lasts several minutes, less often – hours, but no more than a day and ends with complete restoration of impaired functions. If these focal neurological symptoms persist for more than 24 hours, a stroke is diagnosed.
Individual stroke prevention
Traditional medicine knows only two ways to combat stroke: prevention and symptomatic treatment of the consequences of the disease.
“It is easier to prevent than to cure” - this classic saying applies especially to stroke.
Prevention of stroke (and its recurrences) lies in the correct work and rest schedule, rational nutrition and sleep regulation, a normal psychological climate in the family and at work, and timely treatment of cardiovascular diseases: coronary heart disease, hypertension.
Prevention is aimed at eliminating risk factors - active identification and early adequate treatment of patients with arterial hypertension.
Non-drug treatments
· Limiting salt intake. · Reducing excess body weight. · Optimizing physical activity levels. · Reducing the effects of chronic stress and harmful occupational factors. · To give up smoking. · Limit alcohol consumption.
Targeted drug treatment is carried out under the supervision of a physician and is aimed at optimizing blood pressure levels, improving well-being and performance, and reducing the likelihood of developing a stroke.
NSA (National Stroke Association of the USA) has developed guidelines for the prevention of stroke, which are offered to you.
1. Know your blood pressure. Check it at least once a year. If it is elevated, consult your doctor to keep it under control. — High blood pressure is the leading cause of stroke. - If the top number (systolic pressure) is consistently above 140 or if the bottom number (diastolic pressure) is consistently above 90, consult your doctor. — If your doctor confirms that you have high blood pressure, he or she may recommend changes to your diet, regular exercise, or medication. — Drug therapy for arterial hypertension is constantly being improved. If you choose the right medications, you will not experience side effects and your quality of life will not suffer.
2. Find out if you have atrial fibrillation. — Atrial fibrillation (atrial fibrillation) is an irregular heartbeat that impairs cardiac function and allows blood to stagnate in various parts of the cardiovascular system. -Blood that does not move through the body can clot. - Heart contractions can release part of the thrombus into the general bloodstream, which can lead to cerebrovascular accident. — A doctor can make a diagnosis by carefully examining your pulse. — Atrial fibrillation can be confirmed by electrocardiography (ECG). If you have atrial fibrillation, your doctor may suggest taking anti-clotting medications.
3. If you smoke, stop. - Smoking doubles the risk of stroke. - As soon as you stop smoking, your risk of stroke will begin to decrease immediately. - In five years, your risk of developing a stroke will be the same as that of non-smokers.
4. If you drink alcohol, do so in moderation. — A glass of wine or beer every day may reduce your risk of stroke (unless there are other reasons to avoid alcohol). — Excessive alcohol intake increases the risk of stroke. - Remember that alcohol can interact with the medications you are taking and is dangerous in large doses.
5. Find out if you have high cholesterol. — Find out your cholesterol level. — Increased cholesterol levels increase the risk of stroke. - Lowering cholesterol levels (if they were elevated) reduces the risk of stroke. — Reducing cholesterol levels in most people can be achieved through diet and exercise, and only some require drug therapy.
6. If you have diabetes, strictly follow your doctor's recommendations for controlling your diabetes. — Diabetes can often be controlled by an adequate attitude towards your diet. — Work with your doctor and dietitian to create a nutrition program that meets your needs and your lifestyle. — Your doctor may suggest lifestyle changes and medications that will help you control your diabetes. — Having diabetes increases your risk of stroke, but by controlling your diabetes, you can reduce your risk of stroke.
7. Use exercise to increase your activity in your daily life. - Exercise daily. - Walking for 30 minutes every day can improve your health and reduce your risk of stroke. — Go for a walk with friends, it can become a habit. - If you don't like walking, choose other types of physical activity that suit your lifestyle: cycling, swimming, golf, dancing, tennis, etc.
8. A low-salt, low-fat diet is recommended - By reducing the amount of salt and fat in your diet, you will lower your blood pressure, and more importantly, reduce your risk of stroke. — Strive for a balanced diet with a predominance of fruits, vegetables, cereals and moderate protein content.
9. Consult a doctor if you have circulatory problems. — Strokes can be associated with problems related to the heart, arteries and veins, or the blood flowing through them. Your doctor can evaluate you for these problems. — Atherosclerotic plaques can impair blood flow through the arteries that carry blood from the heart to the brain. These arteries, located on each side of the neck, are called carotid and vertebral. - If the blood vessels are blocked, a stroke may occur. — If you have severe anemia or other blood disorders, consult your doctor. Improper management of these diseases can lead to stroke. — Circulatory problems are usually treated with medication. If your doctor recommends medications, take them. — Sometimes surgery is required to correct circulatory problems such as arterial thromboembolism.
10. If you notice the following signs of cerebrovascular accident, seek medical help immediately. - Sudden weakness or loss of feeling in the face, arm or leg, especially if it is on one side of the body; - Sudden loss of vision in one or both eyes; - Difficulty speaking or understanding simple sentences; - Dizziness, loss of balance or coordination, especially when combined with other symptoms such as impaired speech, double vision, numbness, or weakness; - Sudden, unexplained, intense headache.
Therapy for ischemic stroke in the acute period
In the first three weeks (during the acute period), general measures are taken:
- The required oxygen level is maintained;
- Blood pressure stabilizes;
- Cardiac activity is under medical supervision;
- The condition of the bladder and intestines is monitored;
- Passive gymnastics is carried out on all limbs of the victim;
- Prevention of bedsores;
- Antibacterial therapy, including taking antifungal drugs.
Depending on the specifics and subtype of ischemic stroke, special therapy is carried out.
Acute ischemic stroke may recur if the diagnosis is not reliable and not all emergency measures have been taken. In the acute period, secondary hemorrhage into damaged tissue of the cerebral cortex poses a great danger. As a rule, this occurs in the first 10 days after the onset of a stroke. It is almost impossible to detect this complication visually. Only with the help of computed tomography and x-ray examination do they find a new lesion and take action. The reason for this complication is the lack of necessary control over blood pressure, as well as reperfusion therapy. Some patients have serious contraindications for it.
Clinical Brain Institute Rating: 4/5 — 2 votes
Share article on social networks
Rehabilitation after a stroke: chances and opportunities
Stroke is a cardiovascular accident.
Each of us can make efforts to minimize the likelihood of its development, but no one can completely eliminate the disease.
The leading risk factor for stroke is age, and, unfortunately, it is impossible to influence it.
But there is also optimistic information: for at least 70% of patients, a stroke does not become fatal.
And this is where rehabilitation comes to the fore. What does its result depend on?
Three forecasts
Stroke is a disease for which it is very difficult to predict. Most doctors avoid promises and unambiguous statements, and they are right.
The development of events depends on many factors, including those that cannot be foreseen or assessed. The human nervous system is plastic and can literally be capable of miracles of self-healing, including in the case of the most extensive lesions. However, the severity of the consequences can still be assumed based on the type of stroke suffered.
An ischemic stroke occurs when a blood vessel in the brain or spinal cord is blocked, usually by a blood clot. This leads to oxygen starvation of the area of the brain that is supplied by the affected artery.
The brain reacts sharply to hypoxia - within a few minutes after the disaster, cells deprived of oxygen can die. If you quickly administer a drug that dissolves a blood clot, you can quickly restore blood supply and get by with “little blood.”
Programs:
Assessment of rehabilitation potential
Rehabilitation after stroke
Restoration of cognitive functions
Diagnosis of swallowing disorders and correction
Restoration and correction of speech disorders