Medical information is reliable Checked by Samoshkin Anton Aleksandrovich
Our clinic treats Parkinson's disease in Moscow using complex therapy. The best specialists find an individual approach to each person and select the best methods. Since the disease cannot be cured, the goal of providing assistance is to slow down its progression, reduce the severity of movement disorders and improve a person’s quality of life. Thanks to correct and timely actions, it becomes possible to maximize the period during which the patient can move independently, serve himself and perform feasible work.
What is Parkinson's disease
Parkinson's disease is a degenerative pathology associated with disruption of the central nervous system (CNS). It has a chronic and gradually progressive course. In terms of frequency of development in older people, the disease is in second place after Alzheimer's disease. According to world statistics, this problem occurs in every 500 inhabitants on the entire planet. In children, the deviation is practically not observed; the risk group includes people after 40-50 years of age.
Treatment of Parkinson's disease must be carried out with a full understanding of the origin of the disorder and the reasons for its occurrence. Long before the first symptoms and abnormalities are detected, the destruction of CNS cells and associated disorders begins.
The basal ganglia of the central nervous system are responsible for all movements made by a person in the process of life. They are controlled by the cerebral cortex and help with drawing, writing, walking and other activities. These structures determine the muscle group that must be involved in order for everything to work out accurately and efficiently. The cortex gives them active impulses, and the basal formations slow them down a little through the release of dopamine. This allows movements to be precise and targeted in a normal healthy person.
Parkinson's disease occurs due to damage to certain areas of the ganglia, in which atrophy of nerve cells occurs and disruption of the structure and function of the fibers that conduct impulses to the muscles. At the same time, there is a decrease in dopamine, so the signals are not inhibited, but go directly to the muscles. The result is trembling, tremor, constant tension (rigidity), and difficulty making voluntary movements.
Nursing home for elderly people with Parkinson's disease
Constant attention to an elderly person, creating situations in his life that give a person positive emotions from delicious food, communication with loved ones and pets, interesting activities on vacation...
With high-quality care and constant monitoring of the patient in a specialized boarding house, it is possible to achieve partial, in some cases, complete restoration of impaired motor functions for a long time, with minimal risk of side effects of drugs. Moreover, the correct rehabilitation technique allows not only to maintain preserved motor abilities, but also to develop new skills in those suffering from Parkinson's disease.
Our staff has knowledge and experience working with patients suffering from Parkinson's disease and other cognitive disorders that often occur in older people.
Our nurses and carers know how to care for patients with brain disorders . Our boarding house has done everything for the comfort and safety of such residents. We provide:
- premises equipped for accommodation of people with cognitive impairments;
- constant supervision and care of patients by trained personnel;
- dietary nutrition taking into account age needs and medical recommendations;
- assistance to needy patients in eating, hygiene procedures, careful care for bedridden patients;
- necessary medical procedures, exercises to maintain and develop cognitive skills;
- psychological assistance during rehabilitation of people suffering from Parkinson’s disease...
Find out more about the living conditions, care, recovery and rehabilitation of elderly people with dementia in a nursing home near Moscow...
Causes of Parkinson's disease
For a still unknown reason, Parkinson's disease affects men more often. But among coffee and cigarette lovers it is less common. Currently, research is still underway to determine the exact cause of the disease. But the factors that provoke it are already well known:
- aging;
- hereditary predisposition;
- impact of negative factors;
- long-term use of certain drugs;
- traumatic brain injuries;
- infectious diseases of the brain;
- some have chronic pathologies;
- stress and poor nutrition.
Disruption of the structure of the nerve fiber very often occurs due to age-related changes. It is not uncommon for tremor to appear in people who have relatives with this problem, especially for young patients. The toxic effects of poisons, heavy metals, and radiation can also lead to atrophy of brain tissue. The use of antidepressants and antipsychotics helps reduce the level of dopamine and the sensitivity of nerve synapses to it.
Treatment of Parkinson's disease in Moscow begins with identifying and eliminating the main cause of the development of the pathology. Ganglion structures are affected after encephalitis, meningitis, or injury as a result of injury. Psycho-emotional overload, constant lack of sleep, eating low-quality foods, and lack of necessary substances also contribute to disruption of the central nervous system.
Parkinson's disease symptoms and treatment
Treatment of Parkinson's disease is best started when the first symptoms of the disorder appear, this will slow down the progression of the pathology. The patient's relatives should closely monitor his condition. The initial stage of the disease is characterized by the following symptoms:
- decreased expressiveness of facial features;
- slowing down of movements while walking, blinking, eating and dressing;
- difficulty performing precise actions using fine motor skills (fastening buttons, tying shoelaces);
- change in handwriting (it becomes smaller and more illegible);
- decreased energy and fatigue;
- difficulty getting up from a sitting or lying position;
- choosing a shower when washing, since you need to get into and out of the bath;
- difficulty chewing and swallowing;
- increased salivation (salivation) and constant need to wipe your mouth with a napkin;
- drowsiness during the day and problems falling asleep at night;
- slow speech and monotonous pronunciation of phrases;
- decreased ability to learn and perceive new things.
Some people in the early stages of the disease experience symptoms that are in no way associated with parkinsonism. They experience constipation, decreased sense of smell, and absent-mindedness. Relatives notice the patient's unusual behavior during the REM sleep stage (he begins to actively move his arms and legs).
During the period of manifestation, Parkinson's disease is characterized by the presence of the following symptoms:
- Tremor.
Trembling of the upper extremities predominates; it is much less common in the legs. Unlike other neurological pathologies, there is practically no head tremor with this disease. But fine vibration of the tongue and jaw is often observed, especially at a later stage. The maximum severity of the symptom is observed at rest, for example, when a person’s hands lie on the knees or the arm of a chair. If movement is made, the shaking is greatly reduced.
- Rigidity and slowness of movements.
An important symptom of Parkinson's disease is muscle rigidity. It manifests itself in increased tone and the appearance of constant resistance during passive movement. Here a differentiation should be made with spasticity, in which resistance occurs only at the beginning, that is, the “jackknife” syndrome is observed.
Rigidity in Parkinsonism most often affects all muscles of the body. But a number of patients have a predominant disorder of the flexor muscles. This determines the characteristic posture of a person with bent arms and legs (at the knees and elbows), while the arms are pressed tightly to the body (the “petitioner” pose).
Together with increased muscle tone or even in its absence, the “gear wheel” symptom is often observed. It manifests itself during the examination, when the doctor, when flexing and extending the patient’s limb, feels uneven resistance, similar to the sliding teeth of a gear.
- Balance disorders.
Treatment of Parkinson's disease in Moscow and its diagnosis begins with studying the safety of the so-called postural reflexes. In a healthy person, they allow you to stand upright, sit down or stand up, and maintain your posture when exposed to external influences (a push, a stumble). A patient with Parkinsonism is characterized by imbalance. He often falls, and when he sits down, he immediately leans back in the chair or armchair. It is this deviation that leads to a change in gait.
At the same time, the upper part of the body seems to go forward, and the lower part catches up with it, taking quick and short steps. If there is a need to stop immediately, it becomes difficult for the patient to do this, and he may fall. Typically, imbalance, up to the inability to move independently, is observed at a late stage of the disease.
Parskinson's disease, in addition to impaired movement, stiffness and tremors, is accompanied by other non-motor abnormalities:
- depression;
- cognitive problems;
- vegetative symptoms;
- high fatigue;
- lack of sleep or drowsiness;
- dementia and personality changes;
- apathy;
- muscle pain syndrome;
- respiratory disorders.
Sometimes Parkinson's disease develops atypical symptoms, which can make it difficult for even an experienced specialist to diagnose the disease. These include dystonia and dyskinesia. In the first case, contractions of muscle fibers are observed, accompanied by painful sensations. This sign requires differentiation from arthritis. Dyskinesia manifests itself in involuntary twitching and movements of the arms and legs, which decrease somewhat after taking drugs with dopamine.
24/7 CONSULTATION BY PHONE: +7
- Surgery
- Oncology
- Neurosurgery
- Radiology and Radiation Therapy
- Gynecology and new reproductive technologies
- Traumatology and Orthopedics
- Cardiology
- Neurology
- Laser surgery
- Urology, andrology and microsurgery
- Plastic surgery
- Mammalogy
- Lithotripsy
- Psychological support service
- ECO
- Weight loss
- Pressure chamber
- Endovascular surgery
- Pituitary adenomas
- Arnold-Chiari malformation and syringomyelia
- Parkinson's disease
- Hydrocephalus
- Hemifacial spasm
- Herniated discs
- Violent movements
- Brain tumors
- Vascular diseases of the brain
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Essential tremor
Parkinson's disease
is a progressive neurodegenerative disease associated with the loss of dopaminergic nigrostriatal neurons. Parkinson's disease belongs to a group of diseases called movement disorders and is characterized by muscle rigidity, tremors, slowness of movements (bradykinesia) and, ultimately, the absence of muscle movements (akinesia).
Primary symptoms result from excessive stimulation of the motor cortex by the basal ganglia, resulting from insufficient dopamine synthesis by dopaminergic neurons in the substantia nigra. Secondary symptoms may include cognitive and speech impairment. The disease is chronic and progressive.
Pathophysiology
The main finding in pathological examination in Parkinson's disease is the loss of pigmented dopaminergic neurons and the presence of Lewy bodies in the substantia nigra. A decrease in the number of dopaminergic neurons is observed mainly in the ventrolateral part of the substantia nigra. By the time clinical symptoms of the disease appear, the number of dopaminergic neurons decreases by 60-80%. Lewy bodies found in Parkinson's disease are a characteristic feature of idiopathic Parkinson's disease. Parkinson's disease accounts for 75–80% of parkinsonism cases.
Lewy bodies with neurons of the substantia nigra
According to global data, the incidence of the disease is 4.5 - 21 cases per 100,000 per year. In Russia, according to various sources, there are from 117,000 to 338,000 patients with Parkinson's disease. Parkinson's disease is one of the most common diseases of older people (after 65 years, its prevalence reaches 1%, and in the population over 85 years of age, 2.6%). The prevalence of Parkinson's disease in the general population is about 140 cases per 100,000 population. The average age of onset of Parkinson's disease is 55 years. At the same time, in 10% of patients the disease debuts at a young age, before 40 years of age (early-onset parkinsonism) or before 20 years of age (juvenile parkinsonism). The male to female ratio in Parkinson's disease is approximately 3:2. Parkinson's disease is sporadic, but approximately 5% of cases have a positive family history.
Clinical symptoms of the disease
Initially, the symptoms of the disease may be subtle. The onset of Parkinson's disease manifests itself gradually, the neurological manifestations are asymmetrical, usually starting with tremors (tremors) or awkwardness in one arm (about 20% of cases) or leg, less often difficulty in gait or general stiffness. The tremor usually occurs in one limb. There may be fluctuations in the degree of its severity. The amplitude of the tremor increases after stress and decreases after sleep. The patient may notice limited mobility when moving the affected arm, and a foot hitting the floor. After some time, the posture becomes more and more stooped and a shortening of the step length is observed.
Classic image of a patient with Parkinson's disease
At first, patients often complain of pain in the limbs or back, muscle cramps. Some patients experience soreness or a feeling of tightness or pressure in the shoulder or calf area. The initial symptoms of Parkinson's disease can be nonspecific and include fatigue, depression, and sleep disturbances. Autonomic disorders are also characteristic: constipation, orthostatic hypotension, impotence, urination disorders, sweating disorders, seborrheic dermatitis.
When the disease has developed, the main symptoms are:
1. Hypokinesia (slowness, difficulty initiating voluntary movements). Hypokinesia is characterized by slowness of movements (bradykinesia), difficulty initiating movements, inability to generate muscle force of adequate strength and pace (hypometry), for example, when changing body position, a rapid decrease in amplitude and speed during repeated movements (oligokinesia), for example, when squeezing and unclenching brushes Hypokinesia is manifested by the following symptoms:
- Hypomimia (poor reaction of facial expressions).
- Rare flashing.
- Hypophonia (quiet speech).
- Micrography (small handwriting).
- Brachybasia (shortened step length).
- Acheirokinesis (decreased swinging of arms when walking).
- Difficulty getting up from a chair, turning to the sides, or walking.
2. Rigidity (increased muscle tone). Muscle rigidity is an increase in muscle tone, manifested by increased resistance to passive movements. The increased resistance may be monotonous (wax doll phenomenon) or intermittent (cogwheel phenomenon).
3. Rest tremor with a frequency of 4 – 6 Hz (tremor that occurs in resting limbs, head). There are several types of tremor possible. Classic parkinsonian resting tremor with a frequency of 3-6 Hz, in the hand looks like “rolling pills” or “counting coins”. Tremor occurs in a resting limb, decreases with movement in it, but intensifies at rest, with active movements in other limbs, when walking and when attention is distracted. Parkinsonian tremor is often asymmetrical or unilateral (over time becoming bilateral). Most often, resting tremor occurs in the arms, sometimes the legs are involved (usually in the distal parts of the arm or leg), chin, lips, and very rarely the head. Tremor is observed in 80–85% of cases. Postural tremor occurs when maintaining a posture (tremor of arms extended forward or to the sides). Postural tremor is often combined with resting tremor and, as a rule, it is of the same frequency and localization. A differential diagnostic sign that distinguishes postural tremor in parkinsonism from essential tremor is that it does not appear immediately after stretching the arms forward, but after a few seconds. In a number of patients with parkinsonism, high-frequency (6-12 Hz) postural-kinetic tremor is detected, reminiscent of essential tremor, which sometimes appears several months or years before the development of the main manifestations of parkinsonism.
4. Postural instability (instability when changing body position or walking). Postural reflexes ensure the maintenance of balance and vertical position of the body. Their weakening or loss is manifested in an impairment of the ability to maintain balance when changing body position or when walking, which, in combination with hypokinesia and rigidity, leads to impaired walking and falls. When the patient initiates walking or tries to change the direction of his movement, it seems that he is marking time, leaning more and more forward. At the same time, he tries to catch up with the center of gravity of the body with small mincing steps (propulsion), which often ends in a fall.
Classification of Parkinson's disease.
The classification of stages of Parkinson's disease proposed by Hoehn and Yarh (1967) is generally accepted: Stage 1.0 - only unilateral manifestations. Stage 1.5 - unilateral manifestations involving the axial muscles. Stage 2.0 - bilateral manifestations without signs of imbalance. Stage 2.5 - mild bilateral manifestations. The ability to overcome induced retropulsion is preserved. Stage 3.0 - mild or moderately severe bilateral manifestations. Slight postural instability. But the patient does not need outside help. Stage 4.0 - severe immobility; however, can still walk or stand without support. Stage 5.0 - Confined to a chair or bed without assistance.
Drug treatment
Therapy for Parkinson's disease includes treatment of motor disorders (akinesia, rigidity, tremor, postural instability) and non-motor syndromes (mental, autonomic, sleep disorders, etc.). Currently, there is no pathogenetic therapy for Parkinson's disease, i.e. There is no treatment proven to slow or stop the loss of dopaminergic cells. There are two areas of treatment for movement disorders - neuroprotective and symptomatic therapy, the latter being the main one at present. Neuroprotective therapy is designed to slow the loss of dopaminergic neurons, and thereby slow down the progression of the disease. Currently, there are no neuroprotective agents with proven effectiveness. MAO-B inhibitors (selegiline (Yumex), rasagiline), dopamine receptor agonists (pramipexole (Mirapex), ropinirole) and amantadine (Midantan, PC-Merz) are considered as possible neuroprotective drugs. The main goals of treatment are to ensure maximum functional (primarily motor) preservation and quality of life of the patient. In general, therapy is aimed at correcting and alleviating motor and other non-motor symptoms, as well as minimizing side effects, primarily as a result of the use of levodopa. Levodopa is the most effective drug for the treatment of movement disorders in Parkinson's disease; it provides good control over the symptoms of the disease for 4 to 6 years. Long-term use of levodopa is complicated by side effects, the most common of which are motor fluctuations (fluctuations in motor activity) and dyskinesias (hyperkinesis), which increase the patient's maladjustment and are difficult to correct. The current paradigm for the treatment of Parkinson's disease is to initiate levodopa as late as possible through the use of less potent dopaminergic agents that do not contain levodopa. This approach is not shared by all clinicians. Treatment of motor symptoms in persons under 50-60 years of age with moderate severity of the process (stage I-II according to Hoehn and Yarh) begins with dopamine agonists (ropinirole, pramipexole, bromocriptine) or with MAO-B inhibitors (selegiline, rasagiline) or amantadines (midantan , PC-merz). In elderly patients, the drugs of choice are levodopa at all stages of the disease. When a patient is initially diagnosed with stage III (with the development of postural instability) stage of the disease according to Hoehn and Yarh, or when the disease moves to stage III and the therapy used is not effective (even with increasing dosages of drugs), levodopa is usually prescribed, seeking, if possible, a delay in its use and using the minimum effective dose of the drug. The latter is possible, in particular, through the combined use of levodopa and a dopamine agonist (MAO inhibitor, amantadines). If a patient develops side effects of levodopa, in particular a combination of the “wear-out” phenomenon (resumption or significant increase in symptoms of the disease less than 4 hours after taking the last dose of levodopa) and inclusion dyskinesia (peak dose dyskinesia), a reduction in the dose of levodopa and its combination with COMT inhibitor (or dopamine agonist, or MAO inhibitor). In patients with treatment-resistant motor fluctuations or tremor, surgical intervention—deep brain stimulation—can be performed. If rest tremor predominates in the clinical picture of the patient, anticholinergic drugs (cyclodol, akineton) can be prescribed to relatively young patients in the early stages of the disease, or to patients over 60 years of age with the tremulous form of Parkinson's disease (if levodopa is insufficiently effective). In relation to action tremor (postural and kinetic), obzidan is a more effective drug. In general, all antiparkinsonian drugs are less effective against tremor than against akinesia and rigidity, and least effective against postural instability. All of the drugs listed below do not provide a cure for Parkinson's disease, but they can alleviate its symptoms. Typically, treatment must be taken for the rest of your life to prevent symptoms from returning.
Surgical treatment of Parkinson's disease.
Destructive operations. Before the discovery of levodopa and the advent of stimulation of deep brain structures, it was used quite widely. The operation is a surgical destruction (destruction) of certain brain structures (so-called palidotomy, thalamotomy). Currently, destructive operations are a rather rare treatment method, since the consequences of the operation are irreversible. The Federal Center for Neurosurgery, created on the basis of the Federal State Budgetary Institution "Treatment and Rehabilitation Center" is the only institution in Russia that performs destructive operations for Parkinson's disease using modern equipment using a Cosman-Roberts-Wells stereotactic frame
Unilateral destructions:
- thalamotomy
- pallidotomy
Bilateral destruction increases the risk of swallowing disorders, dysarthria, and memory impairment by up to 20%, which is why they are not currently used. The indication for unilateral thalamotomy is disabling tremor, predominantly in one arm. The operation has a fairly high success rate (elimination of symptoms in 80-90% of patients), but does not affect rigidity and bradykinesia in these limbs. Complications of the operation (hemiparesis, dysarthria, memory impairment) are observed in up to 20% of patients, persistent neurological complications - in 10% of patients.
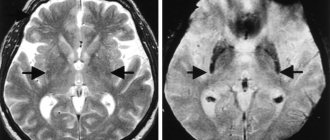
MRI of a patient after performing a right thalamotomy.
The indication for performing unilateral pallidotomies is the presence of severe drug dyskinesia while taking medications. The operation leads to a decrease in tremor, stiffness and bradykinesia in the contralateral limbs (on the side opposite to the destruction).
MRI of the patient after left pallidotomy.
The advantages of destructive operations are their low cost, the possibility of performing them for patients who do not have the opportunity to regularly visit a doctor due to a persistent effect, the absence of the need to correct the parameters of implanted equipment and eliminate the breakdown of components. The disadvantages of destructive operations are the possibility of only unilateral destruction, the impossibility of correcting bilateral disorders, irreversibility of side effects, a relatively high risk of persistent side complications (10% of patients have permanent neurological disorders in the form of dysarthria, hemiparesis, memory impairment). Neurostimulation (DBS, deep brain stimulation) A modern treatment method that is a minimally invasive neurosurgical operation. Beginning of clinical use since the 1990s (stimulation of the globus pallidus, stimulation of the subthalamic nucleus). Currently, more than 55,000 patients have been operated on in the world. Neurostimulation is a proven effective treatment for idiopathic Parkinson's disease, essential tremor and primary generalized dystonia.
This method is used in cases where:
- Despite correctly selected drug therapy, the patient cannot achieve a significant reduction in symptoms.
- progression of the disease leads to the need to increase doses of medications, and the side effects of the drugs become intolerable.
- the patient is socially active and is afraid of losing his job due to the disease.
- the patient becomes incapacitated and becomes dependent on his family to perform daily activities.
Contraindications to neurostimulation are:
- History of lack of effectiveness of L-dopa drugs
- Low intelligence, severe depression, history of suicide attempts
- Unused reserves of drug therapy
- Psychological unpreparedness of the patient for long-term surgery
- Decompensation of diabetes mellitus, severe hypertension, cardiovascular failure, coagulation disorders
- Contraindications for MRI (pacemaker)
- Poor family relationships (need for frequent consultations in the postoperative period)
- High expectations from surgery
- Age over 70
The essence of the method: the therapeutic effect is achieved by stimulating certain brain structures responsible for controlling body movements with a precisely calculated small amplitude electric current. To do this, thin electrodes are inserted into the patient's brain, which are connected to a neurostimulator implanted subcutaneously in the chest area under the collarbone. The operation itself is usually carried out in two stages. At the first stage, under local anesthesia with the help of magnetic resonance imaging and stereotactic neuronavigation, electrodes are introduced into the deep structures of the brain responsible for the control of movements - in the region of the subthalamic nucleus (STN).
Patient with a stereotactic frame fixed to the head
Test stimulation is then performed, during which the patient reports the somatosensory sensations that occur under various stimulation parameters. If the result is positive, the second stage is carried out: the patient is implanted with subcutaneous parts of the system - connectors and a pulse generator (neurostimulator). Usually the second stage is carried out under anesthesia. In the postoperative period, the neurostimulator is programmed and the patient is trained. The patient has the opportunity to adjust the stimulation settings himself (within the limits specified by the doctor) depending on his own well-being and the characteristics of the activity being performed.
Control MRI of the patient's brain after bilateral stimulation of the subthalamic nucleus.
Results of the operation: the period of effective control over the symptoms of the disease increases, the need for anti-Parkinsonian drugs is significantly reduced
Benefits of DBS:
- Allows non-invasive adjustment of stimulation settings as the disease progresses.
- Unlike palidotomy and thalamotomy, it is reversible.
- Can be bilateral (that is, effective for symptoms on both sides of the body).
- It is easily tolerated and is a relatively safe method.
Disadvantages of DBS:
- High cost of equipment
- Contraindications to MRI and electromagnetic therapy
- The need for regular visits to the doctor to correct generator settings and check the possible duration of therapy
- The need to replace the generator after 3-7 years (except for the Restore generator)
- Possibility of technical breakdown, displacement of electrodes (up to 15%) with the need for repeated operations
- The risk of infectious complications is up to 3-5%
- Risk of sudden shutdown of the neurostimulator when passing through an electromagnetic field with the need to turn it on using a special patient remote control
It must be remembered that deep structure stimulation surgery DOES NOT CURE Parkinson's disease , but allows for temporary control of some symptoms!
Classification of the disease and rate of development
Treatment for Parkinson's disease depends on the stage of development of the disease. To determine it, the Hoehn-Yahr classification is used, based on the severity of the manifestations of pathological symptoms:
- Zero.
Some parts of the brain cells begin to deteriorate, but no obvious abnormalities are observed. A manifestation of absent-mindedness is possible, which many at a young age take as a sign of overwork, and at an older age – as normal aging of the body. Sometimes the perception of smells may change slightly.
- First.
The first manifestations begin in the form of trembling of the limbs on one side of the body (hemiparkinsonism), increased tremor is noted after stress. Some deviations can be found in the pronunciation of words, gestures, and posture. The precise movements required when grooming (shaving, combing hair) begin to take longer than before. There is a decrease in mood, loss of strength, and depressive symptoms.
- Second.
The progression of the disease leads to damage to both parts of the body (bilateral parkinsonism), mild postural instability appears, coordination is impaired, and significant fatigue occurs when performing physical activity. Shaking of the head becomes noticeable, the face loses expressiveness, and speech becomes monotonous.
- Third.
All signs and symptoms characteristic of the previous stage become even more pronounced. The balance is noticeably disturbed, but the opportunity for free movement and self-service still remains. The patient's gait changes, it becomes uncertain, and he moves in small mincing steps.
- Fourth.
A person almost completely loses the ability to act independently and care for himself and requires constant care and supervision. He can stand and move with difficulty only with support.
- Fifth.
There is a complete loss of independence and ability to move. The person constantly lies in bed or sits in a wheelchair. Due to impaired swallowing, exhaustion occurs; nutrition is most often provided parenterally.
The transition from one stage to another cannot be determined by a time frame, since it is an individual process. It depends on age and treatment method. In young people, life expectancy after the manifestation of pathology can be up to 40 years, in middle-aged people - up to 20 years. In an elderly patient, the period will be up to 7 years. If you do not take medications or use other methods of assistance, your life time can be significantly reduced.
The duration of each stage can be measured from several months to ten years. There are often cases when a jump occurs from the first stage of stasis to the third, bypassing the second. With the correct selection of treatment, it is possible to transfer the patient with this disease to a lower stage for some time.
Diagnostics
Treatment of Parkinson's disease is impossible without making a correct diagnosis. He diagnoses clinically based on the symptoms of the disease. In this case, three main features are taken into account:
- tremor at rest;
- muscle stiffness;
- hypokinesia.
It is important for the doctor to obtain objective information about the medical history. Therefore, when contacting the clinic, the patient or his relatives must provide the following information:
- at what age deviations began to be detected;
- the first signs of disturbances (handwriting, behavior, facial expressions, gait, tremor);
- gradual or sudden onset;
- absence or presence of cognitive problems (depression, hallucinations);
- whether there are other people in the family with neurodegenerative disorders;
- the presence of traumatic brain injuries, infectious pathology;
- working conditions and hazards;
- established other diseases;
- name of medications taken.
To confirm the disease, you must contact a neurologist; in case of cognitive disorders, you may need to consult a psychiatrist. The basis for establishing a diagnosis is the following criteria:
- unilateral initial manifestation;
- tremor at rest;
- progressive course;
- positive dynamics after taking levodopa;
- course of the disease for 10 years or more.
For differential diagnosis, it is enough to confirm three or more signs. MRI, CT, and ultrasound of brain vessels are used as instrumental methods. They are required to exclude other diseases and concomitant pathologies.
Treatment methods for Parkinson's disease
Treatment of Parkinson's disease in Moscow and other cities should begin with its first manifestations. It is best to involve experienced specialists in this problem who will help you choose the best methods of assistance and rehabilitation.
The lack of therapy or the wrong approach to it significantly shortens the life of a patient suffering from Parkinson's disease. After ten years, and sometimes earlier, he becomes disabled or dies, and after 15 years from the onset of the disease, the mortality rate is already 80%. And even with a sluggish form, without taking medications and using modern techniques, strong everyday disadaptation quite soon occurs, a person’s ability to work and socialization decreases. The quality of life suffers greatly, and the patient himself becomes a heavy burden for family and friends.
Treatment for Parkinson's disease includes:
- taking medications;
- physiotherapy;
- psychological assistance;
- therapeutic exercises;
- special diet.
To correct dopamine, drugs are used that help:
- increase dopamine levels;
- stimulate dopamine receptors;
- inhibit the reuptake of this substance;
- reduce its destruction.
The following medications are used for this:
- Levodopa drugs.
They are among the most effective medications for the treatment of Parkinson's disease, which are used in both early and late stages of the disease. They are recommended in case of disorders associated with functional adaptation, and to a lesser extent these drugs affect tremor. The dose is selected individually; the patient needs to monitor the condition during therapy, since levodopa drugs have multiple side effects.
- Dopamine agonists.
They allow direct stimulation of dopamine receptors and are also recommended for use at any stage. Treatment of Parkinson's disease with their help is carried out in combination with levodopa drugs. Recent studies indicate that the use of dopamine agonists early in the disease helps reduce the likelihood of dikinesia or significantly delay its onset.
- Anticholinergic drugs.
They help reduce the manifestation of tremor and do not have a special effect on the phenomenon of bradykinesia. They are preferable to start treatment of Parkinson's disease in young patients and middle-aged people with a predominance of limb tremors and the absence of cognitive impairment.
- COMT inhibitors.
These medications can increase the concentration of levodopa drugs in the blood plasma. This allows you to achieve the desired effect of therapy using lower dosages of the main drug. Recommended for treatment at any stage of the disease.
- Antidepressants.
This group of drugs helps with depression and decreased social activity of a person. Best used in conjunction with the work of a psychotherapist.
If the disease is at an early stage, the person may not be prescribed medications. His normal activity is maintained with the help of physical therapy, massage, and physiotherapeutic procedures. Psychological assistance is provided to the patient and his environment with the help of experienced specialists.
24/7 CONSULTATION BY PHONE: +7
Postoperative prognosis
Surgery for Parkinson's disease is a matter of last resort. It is resorted to if conservative therapy does not give hope for improvement, or the patient has contraindications to taking medications.
Statistical results on the treatment of Parkinson's do not yet represent a breakthrough in medicine - 55% of patients have significant improvements after surgery, in a third of patients the improvements are questionable, and the condition of 15 percent of those operated on remains unchanged.
However, surgical intervention for such a disease is actively used in medical practice and therapy of this complex disease.
Contraindications
Surgical interventions for Parkinson's disease are not performed for all people suffering from this disease. For some people, hopes for treatment with surgery remain unfulfilled due to the presence of contraindications to surgery. It can be:
- severe depressive states;
- mental disorders;
- decompensated diseases of internal organs;
- focal lesions of brain tissue;
- coagulopathies (blood clotting disorders);
- dementia (dementia).
The surgical method is used in individual cases for patients with severe speech disorders. Therefore, for patients with speech disorders, operations do not guarantee an improvement in the situation and in some cases are not used.
They are not always inclined to perform surgery in cases where patients suffer from severe concomitant pathologies or are at risk of developing severe complications.
Types of surgical interventions
Help with the disease can be provided by several types of surgical intervention. For Parkinson's disease, operations are performed with fundamentally different approaches to eliminating the signs of pathology.
Thalamotomy
Surgical intervention using the thalamotomy method began to be performed for parkinsonism in the 50s of the last century. This was one of the first methods to help people with Parkinson's disease, and therefore thalamotomy had a number of side effects, as well as low postoperative effectiveness.
The essence of the surgical intervention was the destruction of the pathways in the thalamus and the destruction of the nuclei responsible for the occurrence of the impulse.
For a long time, thalamotomy was the only choice in the surgical approach to treating Parkinson's, and was also used in the treatment of other neurological pathologies.
In a modification of stereotactic thalamotomy, the operation involves the introduction for a certain period of time of electrodes that produce electrical stimulation of brain structures. During the destruction (destruction) of pathological foci, impulses in the ventrolateral and subthalamic nuclei either do not arise or are not carried out.
For parkinsonism, the operation gave good results - positive dynamics were noted in seventy percent of operated patients, however, statistics show that almost 65% had relapses.
Neurotransplantation
Neurotransplantation is a novelty in the surgical treatment of Parkinson's. The first operations were carried out by Swedish specialists more than thirty years ago. At first, the success of such an operation was not obvious, since it was not possible to completely cure people from parkinsonism, however, positive trends increased significantly, especially while taking medications.
The Swedish experience began to spread everywhere, and many clinics around the world began to use this method of radical therapy for parkinsonism. Patients were implanted with either a piece of tissue or a cell suspension. The transplant was embryonic tissue from four embryos of the first trimester of development.
As further studies confirmed, dopaminergic activity in the area of the transplant increased in the operated people . This made it possible to achieve the following results:
- Almost all patients experienced a decrease in motor symptoms of the disease to one degree or another.
- The duration of action of the key drug, Levodopa, increased.
- The characteristics of tremor changed, especially the indicators of movement deceleration and their ability to adapt.
- Improvements after surgery became obvious much earlier - in some patients they occurred immediately after surgery, and in others - within 3-6 months after surgery.
There are practically no complications in the surgical treatment of Parkinson's disease, since the embryonic tissue has a high survival rate and does not provoke postoperative risks.
To date, several hundred patients have already been operated on using this technique, but it is still difficult to compare the results, due to the difference in supportive conservative treatment in the postoperative period, various rehabilitation methods, etc. Reviews about the results of the operation are both positive and negative.
Pallidotomy
Pallidotomy is a type of surgery to treat Parkinson's disease. The operation was first performed in the 60s of the last century, but it was postponed for twenty long years due to hopes for the use of drugs for conservative treatment.
The technique became widespread only in the 90s. XX century Today, surgery is practically not used, since it has been replaced by deep brain stimulation.
The indication for surgical treatment by pallidotomy is the preservation of cognitive abilities in patients with motor abnormalities and “on-off” phenomena. Pallidotomy is also performed in patients with muscle spasms and hyperkinesia. When performing surgery for Parkinson's disease using pallidotomy, it is possible to intervene on only one side.
If surgery is necessary on the second side, it is performed no earlier than six months after the first operation . It has been noted that bilateral surgery is more fraught with complications than unilateral surgery, and in general, the unilateral method is better tolerated by patients, especially in old age.
Before surgery, all medications are stopped half a day before surgery. The surgeon makes a trefination hole in the skull and places an electrode near the area of interest.
During the intervention, a conversation is held with the patient, his ability to think, speak, see and hear is assessed (operation under local anesthesia).
During the operation, stimulation is performed at several points.
The first positive results can be seen after the operation. Surgery is much better tolerated than thalamotomy, but there is also a risk of complications.
Deep brain stimulation
Deep stimulation surgery is new. Used in patients with severe symptoms of Parkinson's disease. Surgical treatment of Parkinson's disease with this method makes it possible not to destroy brain cells, affecting healthy tissue.
The purpose of the procedure is to block electrical signals emanating from pathological foci . It is used as a method of therapy in seriously ill patients whose symptoms cannot be controlled with medications.
Non-drug methods
Treatment of Parkinson's disease in our clinic is not limited to the selection of medications. To improve the condition, it is recommended to use a diet. According to the research results, the patient has positive changes in motor function with certain dietary habits:
- reducing the amount of protein food;
- sufficient fluid intake (in the absence of contraindications);
- frequency of meals – up to 4-5 per day, in small portions;
- complete cessation of alcohol consumption;
- regular intake of caffeinated drinks;
- consumption of berries high in anthocyanins (strawberries, raspberries, currants);
- a decrease in vitamin D levels in Parkinson's disease requires constant intake of fish and seafood, as well as regular walks in sunny weather.
Great importance is given to doing exercises. Physical therapy for neurodegeneration helps:
- improve cerebral and peripheral blood flow;
- accelerate the production and action of dopamine;
- reduce oxidative stress;
- reduce the severity of tremor;
- strengthen muscle tissue and prevent its atrophy;
- prevent falls and injuries, normalize coordination.
The specialist selects certain exercises that should be performed regularly, for 20 minutes, 2-3 times a day, only in this case can you count on the formation of muscle memory. This complex includes stage plastique movements, training in relaxation and proper breathing. This takes into account the age and degree of endurance of the person, the presence of complications and other factors.
The frequency and duration of movements depends on the stage of the pathology and the person’s activity. They are selected in such a way that all muscle groups are trained, but with an emphasis on areas that require more correction.
Treatment of Parkinson's disease in Moscow involves the use of physiotherapy. Various methods of exposure can be used already in the first stages of the disease. They help reduce pain symptoms, remove hypertonicity of muscle fibers, and improve tissue trophism. The positive effect of physiotherapeutic treatment methods on the central, autonomic and peripheral nervous systems, as well as the condition of the musculoskeletal system, has been proven.
The following types of therapy are recommended for patients with parkinsonism:
- transcranial magnetic brain stimulation;
- pulsed electrotherapy on the cranial area;
- magnetic therapy;
- pulsed low-frequency electrostatic therapy on the lower leg muscles;
- pressotherapy in the lower extremities and lower back;
- electrophoresis with drugs to relieve spasms and pain;
- electrosleep;
- ultraviolet irradiation;
- balneotherapy and mud therapy.
If you make an appointment at Dr. Isaev’s clinic, you can not only significantly improve the condition of a loved one. An important aspect of the treatment of Parkinson's disease is family consultations with a psychologist. The patient’s relatives are explained the features, causes and signs of the disease, told how to care for a person with this problem, and taught how to properly communicate with him.
Parkinsonism syndrome
The main evidence of Parkinson's disease is the syndrome of the same name, which is expressed in stiffness of all muscles, slowness of movement, uncertainty in walking, trembling of the arms and legs in a calm state.
At first, all these symptoms appear only on one side (left or right), then they spread to the patient’s entire body.
The earlier and more accurately the diagnosis of the disease is made, the better it is possible to determine the method of treatment and long-term support for the patient’s high quality of life.
When you discover the first disturbances in the behavior and condition of a loved one, you should contact a neurologist who specializes in movement disorders. A neurological examination will evaluate the person's coordination, gait and fine motor skills and neuropsychological status.
Questions and answers
How quickly does Parkinson's disease develop?
This disease tends to progress very slowly, and therefore for years the person and his environment are not aware of his problem. The developmental stage with clinical manifestations occurs after the death of more than 60% of dopamine neurons. There are no early signs due to a compensation mechanism in which healthy areas take on the functional responsibilities of damaged ones. For young people, life expectancy with this diagnosis can be 20-40 years; for older people, the prognosis is less optimistic; they live on average 6-7 years.
Is it possible to cure this disease forever?
Currently, medicine does not have the means and capabilities to completely cure this disease. But with a competent and comprehensive approach, it is possible to significantly improve the patient’s quality of life and delay the development of motor and other disorders for a long time. It is almost impossible to do this on your own at home. Therefore, you should contact experienced specialists and follow their recommendations.