What it is?
Photo 1. Girl with Dandy-Walker syndrome
Dandy-Walker syndrome belongs to a group of incurable congenital defects that affect the functions of the nervous system. In the ICD-10 the disease is assigned code Q03.1: “Atresia of the foramina of Magendie, Luschki .
The defect was first described in 1921 by neurosurgeon Walter Edward Dendy. He studied the causes of hydrocephalus. Independently of each other, the study was also carried out by Arthur Earl Walker. In 1942, his article about the absence of ducts in Luschka and Magendie was published. The work of neurosurgeons is taken as the basis for the study of the defect.
Features of Dandy-Walker syndrome:
- formed during the period of intrauterine formation of the brain;
- the cause is considered to be chromosomal disorders;
- the defect is detected by ultrasound at 13–23 weeks of gestation;
- one case per 25 thousand fetuses and infants is diagnosed;
- the defect is more often detected in girls;
- in children with the syndrome, the skull may not be deformed;
- children with cerebellar anomalies are more likely to die at an early age;
- compression of the brain by a cyst affects the functions of internal organs through the nervous system;
- often accompanied by other congenital defects.
Photo 2. Signs of Dandy-Walker syndrome
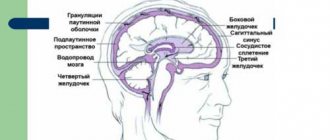
Dandy-Walker syndrome is characterized by an anomaly in the structure of the cerebellum and hydrocephalus. The fourth ventricle of the brain expands. At the same time, a cyst with cerebrospinal fluid forms in the area of the posterior cranial fossa, since the circulation pathways (foramina of Luschka, Magendie) are narrowed or absent. An anomaly of the vermis is also identified: the connecting structure of the cerebellar lobes does not develop or is formed incorrectly.
As a result of Dandy-Walker syndrome, the circulation of cerebrospinal fluid is disrupted . The increasing volume of fluid inside the skull increases pressure, compressing brain tissue. This disrupts the functions of the organ, inhibits the child’s mental development, causes headaches and muscle spasms. The accumulation of cerebrospinal fluid from the inside expands the skull, puts pressure on the nuclei of the brain nerves, deforms the head, and impairs the functioning of the central nervous system. As a result of the disease, life expectancy decreases and the death of the child may occur .
Clinical signs
As a result of fluid accumulation, intracranial pressure increases. Clinically, this manifests itself in the form of the following symptoms of hydrocephalus:
- Feeling of heaviness in the head and pressure on the eyeballs. Typically, patients complain of discomfort at night or in the morning. After the patient wakes up and gets out of bed, the heaviness and pain quickly go away on their own.
- Headache that occurs at night or early in the morning. It has no specific localization and seems to be spread all over the head. The heaviness and pain in the head is pressing or bursting in nature and can intensify when lying down.
- Attacks of nausea or vomiting in the morning or at night. The symptom has nothing to do with eating or drinking liquids, but often accompanies a headache. After the vomiting stops, the patient feels relief.
- Prolonged and frequent attacks of hiccups.
- Severe weakness and rapidly increasing fatigue, pre-fainting.
- Constant sleepiness with yawning.
- Distracted attention, the patient cannot concentrate even on the simplest and most familiar actions, complains of “dullness.”
- Mental disorders - apathy or increased irritability.
- Frequent changes in blood pressure and heart rate.
- Sweating.
- A characteristic external sign is dark circles under the eyes. If you slightly pull back the skin of the lower eyelid, the expanded capillary network becomes clearly visible.
When a significant amount of cerebrospinal fluid accumulates, local symptoms of compression or infringement of brain structures may develop. They directly depend on the level at which the compression occurred.
These include:
- Visual disturbances - double vision, inability to focus, decreased visual acuity, swelling of the optic discs, atrophy of the optic nerve fibers with loss of part of the visual fields or its complete loss, strabismus, lack of pupillary response to light stimuli. A foggy veil may appear before the eyes.
- Clinical signs of vestibular ataxia include gait instability, dizziness, noise in the head and ears, and nystagmus.
- The patient's head takes an unnatural position.
- Increased tone of skeletal muscles and tendon reflexes.
- Paralysis or paresis of skeletal muscles, most often affecting the limbs on one or both sides.
- Impaired sensitivity - possible loss of tactile, temperature and other types while simultaneously increasing the threshold of pain sensitivity.
- Formation of spastic contractures - the muscle tone of the limbs increases significantly, as a result of which the arms or legs freeze in a bent position and cannot be straightened.
- Signs of cerebellar ataxia are disturbances in gait and coordination of movements, changes in handwriting. All movements become sweeping. This phenomenon is observed only in a closed form with localization of the process in the cerebellum (in the posterior cranial fossa).
- Emotional disturbances - lability, causeless euphoria can abruptly give way to a state of apathy. Possible neurasthenia. With a sharp increase in intracranial pressure, outbursts of aggression are possible.
- Epilepsy attacks develop.
- In severe cases, breathing becomes impaired and depression of consciousness develops, leading to coma.
- In the chronic form of hydrocephalus in adults, the clinical picture increases more slowly. Confusion and dementia develop. The patient loses the ability to care for himself.
- In advanced cases, urinary and fecal incontinence is possible.
Causes and triggers in children
Evidence-based medicine experts have not established the exact causes of congenital cerebellar anomalies. Doctors believe that Dandy-Walker syndrome occurs due to a genetic disorder, a chromosomal disorder, or excessive production of cerebral fluid. Triggers (provoking factors) include the influence of toxic and harmful substances that poison a woman’s body.
Reference! The risk of a congenital defect in the fetus during a second pregnancy does not exceed 7% if there is no genetic prerequisite for the mother or father.
The risk of fetal defects increases in pregnant women:
- alcoholics;
- smokers;
- drug users;
- taking medications with embryotoxic or teratogenic effects.
A genetic disorder can be caused by radiation or cytomegalovirus, rubella, or other viral infections during pregnancy. A trigger is also considered to be the presence of diabetes mellitus, an autoimmune disease, or a metabolic disorder in a woman. Heredity plays a major role, that is, congenital defects have already been recorded in the family history.
Symptoms and signs
Before the birth of the baby, the pregnant woman does not experience any disturbance or complication of gestation. In the fetus, ultrasound reveals only cerebellar defects: underdevelopment, enlargement of the fourth ventricle, and the formation of a cerebrospinal fluid cyst.
After birth, unnatural behavior of the baby is added to the ultrasound signs of Dandy-Walker syndrome. Because of his headache, he constantly cries. Compression of the brain by a cyst leads to convulsions, twitching of the limbs, and increased muscle tone. This is manifested by impaired motor skills, involuntary rotation of the eyes, and the joints of the arms and legs are bent.
Signs of a congenital defect of the cerebellum and cerebrospinal fluid tract include:
- large size of the top of the head;
- soft skull;
- protrusion of the fontanel;
- deformation of the face, back of the head;
- stopping breathing (apnea);
- dropsy of the brain (not everyone);
- fusion of fingers or other congenital defect;
- long-term failure of fontanelle to heal.
As you grow older, mental retardation and impaired motor skills (coordination) appear. The child is capricious, irritable, cannot walk smoothly or stand steadily. Seizures occur periodically. In the morning, vomiting, nausea occur, and the headache intensifies. During the examination, visual impairment is revealed.
50% of children have no significant symptoms. A child from this group does not have a deformed head. But coordination of movements is impaired, the gait is swaying, and the legs are widely spaced while walking. There is a slight lag in the development of psychomotor skills and mental activity.
Reference! Rarely, symptoms and signs of a birth defect appear in children after 4 years of age or in adults.
Classification of hydrocephalus
In clinical practice, there are several classifications of pathology. They are built on the basis of various criteria. Depending on the causes, mechanism of development and duration of the course, the following varieties are distinguished:
- Closed hydrocephalus (occlusive, obstructive) - develops in cases where there is an obstacle to the exit or outflow of fluid. The obstruction can be located in various openings (interventricular, Luschka, Magendie). As a result, cerebrospinal fluid does not enter the subarachnoid space and brain cisterns. Depending on the location of the obstruction, hydrocephalus of one or both lateral ventricles may develop. When the foramen of Luschka or Magendie are blocked, fluid accumulates in all structures of the brain.
- Open (communicating) - develops in cases where cerebrospinal fluid is not absorbed into the systemic circulation, and no obstacles to the movement of fluid have been identified. The accumulation of fluid leads to increased intracranial pressure, expansion of the ventricles and subarachnoid spaces, and atrophy of the brain substance. Typically, this picture develops with inflammation of the meninges or hemorrhages.
- Congenital hydrocephalus is formed during intrauterine development. Symptoms appear in the first months after birth. The most common causes of congenital hydrocephalus are developmental defects and anomalies, hemorrhages in the ventricles of the brain, intrauterine infection, and birth trauma. Usually congenital forms of the disease are closed.
- Acquired hydrocephalus develops in children after birth or in adults as a result of infectious and inflammatory diseases, hemorrhages, traumatic brain injuries, tumors, strokes, and parasitic diseases.
- Replacement hydrocephalus is a condition that accompanies primary atrophy of the cortex and subcortical formations. As the volume of the medulla decreases, its place gradually begins to fill with cerebrospinal fluid. In this case, the balance of fluid production and absorption does not occur; this form does not require additional treatment. The exception is the normal pressure type of hydrocephalus, in which the pressure of the cerebrospinal fluid remains normal, but the walls of the ventricles are excessively stretched. A similar picture can develop in elderly and elderly people, with various encephalopathies.
- Depending on the duration and nature of the course, acute and chronic forms of the disease are distinguished. The acute type begins very quickly, and the patient’s condition can deteriorate sharply within a few days. This course is inherent in the closed form of the pathology. The acute form requires immediate neurosurgical treatment. The chronic form requires a period of six months or more to develop. The increase in pressure and expansion of structures occurs gradually and slowly. Neurological symptoms also increase gradually. The chronic course is more typical for open forms of hydrocephalus.
- Based on the localization of the pathological process, external and internal forms of the disease are distinguished. In the external form, cerebrospinal fluid accumulates in spaces located outside the brain tissue, but inside the meninges (subarachnoid space). Inside the ventricles, hydrodynamic parameters do not change. The external form usually accompanies cortical atrophy. In the internal form, fluid accumulates in the ventricles and cisterns of the brain.
- Based on the severity of the condition, hydrocephalus is divided into compensated and decompensated forms. With the compensated type, excess cerebrospinal fluid does not compress the brain tissue and does not cause characteristic symptoms. In the decompensated form, accumulated fluid compresses the brain structures, resulting in the development of characteristic neurological signs.
- Another classification of severity divides hydrocephalus into moderate and severe. Such characteristics of the pathological process are given based on MRI results. However, it should be taken into account that the MRI picture can change repeatedly over a short period. In order for the diagnosis of moderate or severe hydrocephalus to be as reliable as possible, it is necessary to conduct the examination several times with a break of 2-3 weeks.
Dandy-Walker syndrome in adults
Statistics contain information when a cerebellar defect was diagnosed after a person reached adulthood. The disorder is more often referred to as a type of cerebral hydrocele. In these cases, the signs and symptoms of Dandy-Walker syndrome appear gradually after age 18.
As the condition worsens:
- the volume of the head increases;
- the occipital bone moves outward;
- I have a headache and medications don’t help;
- convulsions occur periodically;
- increased muscle tone - muscles are tense, sometimes to the point of spasm;
- Coordination deteriorates - unsteady gait, unclear movements;
- motor skills slow down;
- movement of the eyeballs is partially uncontrolled.
Intellectual impairments include memory impairment and loss of acquired skills. A person stops recognizing relatives and friends, becomes irritable, forgets how to read, dress, write, and so on.
Forms
During the prenatal period, doctors classify complete and incomplete forms of the defect. In the first case, the cerebellum is undeveloped: the vermis is absent, the cyst is connected to the fourth ventricle. In the second type, the defect is partially formed. The structure between the lobes is visible in places on ultrasound; the fluid cavity does not communicate with the entire surface of the worm.
After childbirth, doctors distinguish open and closed forms of the defect. The difference between these types is based on the patency of the liquor pathways. In the first case, there is a communication of the ventricle through the foramina of Luschka and Magendie with the subarachnoid space. In the closed form, the ducts are closed.
Diagnostics
A woman is examined by ultrasound once every trimester. Ultrasound scanning is harmless to the fetus and can detect abnormalities in the early stages. A brain scan can reveal developmental abnormalities as early as 2.5 months of pregnancy. But to confirm Dandy-Walker syndrome, an ultrasound is repeated at 20–23 weeks of gestation. At this stage, a cerebrospinal fluid cyst, abnormal structure of the cerebellum, and deformation of the fourth ventricle are already visible.
If signs are detected again, the woman is prescribed an MRI. Based on the form of the birth defect, doctors assess the severity of Dandy-Walker syndrome. Due to the incurability of the disease, termination of pregnancy is recommended. But the final decision is made by the child’s parents.
After birth, the doctor examines the baby, feels and measures the head. Doctors evaluate the symptoms and external manifestations of the disease, then the child is sent for an ultrasound of the internal organs and neurosonography. From the mother, the doctor finds out the family history, lifestyle, course of pregnancy, cases of self-medication and the type of drugs used. It is advisable for the mother to consult a geneticist.
Important! The inexperience of an uzist or doctor increases the risk of error. To confirm the diagnosis, a pregnant woman must consult and/or undergo further examination with 2–4 doctors from independent medical institutions.
Principles and methods of treatment
The main method of radical treatment of cerebral hydrocephalus is surgery. During the operation, the patient is fitted with a special shunt, which allows excess cerebrospinal fluid to be drained into the bloodstream. As a result, fluid leaves the cranial cavity freely. Intracranial pressure normalizes, and the symptoms of the disease disappear.
All operations aimed at eliminating hydrocephalus can be divided into 2 large groups. The first group includes interventions with the release of cerebrospinal fluid into the vascular bed:
- installation of a shunt between the ventricles or cisterns of the brain and the abdominal cavity (this shunt is called ventriculoperitoneal);
- implantation of a shunt connecting the brain and atria;
- installation of a shunt connecting the skull with the pleural cavity;
- implantation of a tube connecting the cranial cavity to the bladder;
- connection of the peri-cerebral spaces with the venous bed.
The second group includes methods of so-called internal bypass. In this case, channels are created in the cranial cavity for the free passage of cerebrospinal fluid. These include:
- Torkildsen operation (ventriculocisternostomy) - a silicone catheter is installed between the lateral ventricles and the occipital cistern, which is passed along the occipital region under the skin.
- Endoscopic ventriculostomy of the third cerebral ventricle. With this type of intervention, the bottom of the interpeduncular cistern is dissected in the area of the gray tuberosity. As a result, a free passage for liquid is formed.
- Stenting of the Magendie and Luschka holes - installation of special expanding elements (stents).
- Plastic surgery of the aqueduct is the expansion of its lumen to ensure normal flow of cerebrospinal fluid.
- Fenestration (dissection) of the interventricular septum. This creates an opening through which cerebrospinal fluid can circulate freely.
The opinions of specialists regarding this method of treatment today are ambiguous. Even if the operation is successful, this is not a lifelong guarantee of getting rid of hydrocephalus. In children, the head can grow, the size and proportions of brain structures can change, which affects the state of the cerebrospinal fluid flow. In addition, shunts and catheters can become clogged, become infected, etc. To avoid the development of complications, it is necessary to constantly be observed and treated by a neurosurgeon, undergo regular examinations and promptly eliminate all negative changes.
Drug therapy
In some cases, surgical treatment can be replaced with conservative treatment. For this purpose, diuretics are used, which remove excess fluid from the body, thus reducing intracranial pressure. This method is suitable for the treatment of acquired forms of the disease (post-traumatic, developed against the background of inflammation or hemorrhage in the cerebral ventricles). Diuretics can also be used in complex therapy in preparation for surgery. In this case, their use is a forced emergency measure to prevent the death of the patient.
For treatment, the drugs Furosemide, Diacarb, Mannitol, Fonurit are used. The use of these medications does not eliminate the cause of the disease and is only an auxiliary measure.
If the cause of hydrocephalus is an inflammatory process, antibacterial and anti-inflammatory drugs are prescribed.
Treatment of hydrocephalus of the brain in an adult includes means to improve the trophism of brain tissue. The patient is prescribed metabolites, nootropics and vascular drugs - Actovegin, Vinpocetine, Glatilin, Cortexin, Semax, etc.
Treatment methods
Patients with congenital defects and their parents are provided with palliative care. This includes methods of supportive therapy, consultations with psychologists and social workers.
Drug and surgical treatment are used for severe symptoms of the defect. If there is no intracranial hypertension, hydrocephalus and other dysfunctions of internal organs, the child is under medical supervision. He should be regularly examined by a neurosurgeon, neurologist, and pediatrician.
Children with Dandy-Walker syndrome are given maintenance therapy with vitamin-mineral complexes and amino acids. Medicines are also prescribed to eliminate the severe symptoms of the defect. To restore the functioning of the heart, kidneys, and other organs, drugs are selected individually according to medical indications.
Drugs prescribed for Dandy-Walker syndrome:
- Sedatives and sedatives - eliminate the child’s irritability and capriciousness.
- Antispasmodics and analgesics - relieve pain.
- Vitamin B - increases the transmission of impulses to neurons.
- Plasma replacement solutions inhibit the development of complications of Dandy-Walker syndrome. They support the vital activity of cells, the functioning of the brain and internal organs.
- Corticosteroids - reduce the production of cerebrospinal fluid in the ventricles of the brain.
- Vasodilators - expand the lumen of blood vessels, facilitate the outflow of cerebrospinal fluid in open forms of the defect, and blood circulation.
- Diuretics - the diuretic effect helps remove excess fluid from the vessels. This reduces intracranial pressure.
- Beta blockers - relieve swelling of brain tissue.
Physiotherapy is also prescribed . It includes exercise therapy, balneotherapy - therapeutic mud, swimming, salt baths. The doctor also prescribes massage. These methods are aimed at reducing the patient’s muscle tone, as well as improving his psycho-emotional state.
The operation is indicated to restore the outflow of cerebrospinal fluid in another way. Two methods are used: ventriculoperitoneal shunting or endoscopic ventriculostomy. In the first case, a soft tube is inserted into the ventricle. Then the catheter is directed subcutaneously behind the ear and in the collarbone area into the abdominal cavity. Liquid will flow into it and dissolve.
During ventriculostomy, a hole is made in the cranial bone, a neuroendoscope is advanced into the ventricle, and excess cerebrospinal fluid is drained. The procedure is minimally invasive, short-lived, the patient is discharged on day 3, no late complications were recorded.
Reference! Surgical treatment eliminates only hydrocephalus and intracranial pressure. Mental abilities, coordination of movements or central nervous system functions are not restored by the operation.
Diagnostic methods
Diagnosis of hydrocephalus syndrome is carried out on the basis of examination of the patient, clinical data and results of laboratory and instrumental studies. It can be somewhat easier to recognize pathology in a child even by external signs - an increase in the volume of the head, the characteristic position of the eyeballs, etc. In an adult, it will not be possible to identify intracranial hypertension only by external signs. Upon examination, no external changes will be detected, and general cerebral and focal symptoms can be caused by other neurological disorders.
To make an accurate diagnosis, it is necessary to carry out the following set of measures:
- Questioning and examining the patient - the doctor clarifies the nature and severity of subjective complaints, the time of their appearance, the presence of concomitant pathologies, information about past infections, injuries, surgical interventions, strokes, etc.
- The next step will be to examine the patient with special neurological tests to assess coordination of movements, muscle tone, function of the extraocular muscles, etc. The simplest to perform are the finger-nose test, assessing stability in the Romberg position, and identifying nystagmus. The severity of tendon reflexes is also assessed.
- In children, measuring head circumference is of diagnostic importance. If this indicator increases by more than 1.5 cm per month, there is a high probability of developing hydrocephalus. In an adult, any increase in the volume of the head can be a sign of hydrocephalus.
- Spinal puncture is an invasive diagnostic and treatment method. A cerebrospinal fluid sample is taken to determine the value of intracranial pressure and the presence of inflammatory processes.
- Examination of the fundus can reveal swelling of the optic nerve head and pathological changes in the retina inherent in neurological diseases.
Instrumental studies
After a thorough examination, the specialist can prescribe the patient a set of instrumental examinations to establish an accurate diagnosis and the cause that caused it.
- Computed tomography allows you to examine the condition of different parts of the brain, ventricles and subarachnoid spaces. In addition, the condition of the skull bones is assessed, possible pathologies are identified - tumors, cysts, vascular aneurysms, areas of hemorrhage. The diagnostic criterion for hydrocephalopathy is the expansion of the cavities of the ventricles and subarachnoid spaces, and a decrease in the volume of brain structures.
- Magnetic resonance imaging is a method that allows you to determine the amount of fluid in the cranial cavity, the shape and severity of hydrocephalus. In addition, based on the data obtained, a preliminary conclusion can be made about the possible causes of the pathology.
- X-ray of the skull can reveal characteristic changes in children - changes in the shape of the skull, the appearance of characteristic “finger impressions” on the bone tissue. In adults, this method may be less revealing.
- Angiography of cerebral vessels is performed with the introduction of a special X-ray contrast agent. Using this method, you can assess the condition of the vessels, the degree of expansion and thinning of their walls, the presence of obstacles to blood flow, etc.
- Cisternography is an x-ray examination method with the introduction of a contrast agent. The method is used to clarify the nature of the movement of the cerebrospinal fluid, the form of hydrocephalus and the presence of obstacles in the structures of the brain.
- Echoencephalography is an ultrasound diagnostic method that allows one to identify dilations of the cerebral ventricles and cisterns and the presence of pathological changes in them.
Peculiarities of childhood
In children of the first year of life, neurosonography - ultrasound examination of the skull - is of diagnostic value. At this age, the fontanel is not yet closed, and the state of the central nervous system can be assessed. In children older than one year and adults, the fontanel usually becomes overgrown, the bone tissue becomes very dense, so it is pointless to use this method.
This method provides very approximate information and cannot in itself serve as a basis for making a diagnosis. However, changes in neurosonography may be an indication for computed tomography or magnetic resonance imaging.
Prevention
There is no specific prevention. A woman should lead a healthy lifestyle and avoid contact with harmful substances. During pregnancy planning, you need to be re-examined and cure any identified sexually transmitted infections. During pregnancy, you should not take medications with teratogenic or embryotoxic properties. These drugs also cause birth defects and defects.
For prevention purposes, you should not skip scheduled visits to the gynecologist and ultrasound. Early detection of infectious and inflammatory diseases and their treatment reduces the risk of birth defects.
Possible complications and consequences
The prognosis of the disease depends on the severity, form, general condition of the patient and the presence of concomitant diseases. The cause of consequences dangerous to the life and health of hydrocephalus is prolonged compression of the brain structures by excess fluid. The sooner the disease is detected and treatment is started, the better the prognosis. In the early stages, dropsy is considered curable. If you do not begin to treat dropsy of the brain in a timely manner, this can lead to the development of the following complications:
- decreased tone and strength of skeletal muscles, movement coordination disorders;
- atrophic tissue changes;
- deterioration of visual acuity and hearing;
- decrease in memory and intellectual functions up to total dementia;
- disturbances in mental activity, deterioration in concentration;
- violations of respiratory and cardiac function;
- pathological shift in water-salt balance;
- the occurrence of epileptiform seizures;
- partial or complete loss of performance and self-care skills.
In such cases, the patient may be recognized as disabled. Only timely and properly selected treatment can prevent the development of such complications.
What do you need to remember?
- Dandy-Walker syndrome belongs to congenital severe and incurable cerebellar defects.
- The disease can be caused by a virus or any factor affecting the formation of the embryo.
- External signs include head deformation; other symptoms include crying, poor coordination, and mental retardation.
- In adults, signs of the defect appear late.
- The defect has two forms and may be accompanied by dropsy of the brain.
- Symptomatic therapy drugs are used for life; surgery is performed to restore the outflow of cerebrospinal fluid.
- Complications include disruption of the functioning of internal organs and the central nervous system.
- People with severe birth defects do not live long.
- General recommendations are used as prevention: a healthy lifestyle, timely treatment.
Literature
- Neurology and neurosurgery / ed. A.N. Konovalova, A.V. Kozlova; E.I. Gusev, A.N. Konovalov, V.I. Skvortsova: textbook: - vol. 1. - 2009. - 624 p.
- Nikiforov A.S., Konovalov A.N., Gusev E.I. (ed.) Clinical neurology: In 3 volumes - Vol. 3, part 1, part 2. - M.: Medicine, 2004.
- Benda C. Dandy-Walker syndrome or so-called atresia of the foramen Magendie // J. Neuropathol. Exp. Neurol. 1954. Vol. 13. P. 14.
- Snyders RJM, Nicolaides KX Ultrasound markers of fetal chromosomal defects. M.: Vidar, 1997. 192 p.
- Conford E, Twining P. The Dandy-Walker syndrome: the value of antenatal diagnosis // Clinical Radiology. 1992. Vol. 45. P. 172-174.
- Yudina E.V., Medvedev M.V. Perinatal outcomes in congenital malformations. Dandy-Walker syndrome // Ultrasound diagnostics in obstetrics, gynecology and pediatrics. 2000. No. 4. P. 266-271.
- Osenbach RK, Menez,es AH Diagnosis and management of the Dandy-Walker Malformation: 30 years of experience // Pediat. Neurosurg. 1992. Vol. 18. P. 179-189.
- Nyberg D., Mahony B., Hegge F. et al. Enlarged cisterna magna and the Dandy-Walker malformation: factors associated with chromosome anomalies. Obstetrics and Gynecology. 1991. Vol. 77. P. 436-442.
- Congenital malformations: prenatal diagnosis and tactics / Ed. B.M. Petrikovsky, M.V. Medvedeva, E.V. Yudina // M.: RAVUZDPG, Realnoe Vremya, 1999. 254 p.