Ependymoma is a pressing problem in oncology, neurology and neurosurgery. The most complex organ of the human body is the brain, which consists of tissue called ependyma. All the internal cavities of the brain are filled with this tissue. Under the influence of various factors, ependyma can change - grow, transform into a tumor of ependymocytes (epithelial-like cells). The location of emendioma is usually the posterior cranial fossa. People of all ages are susceptible to the disease. Mostly the neoplasm is benign. It is more common in pediatric patients: 60% of patients with ependymoma are children under 5 years of age. Moreover, unlike adults, in children the tumor is in most cases malignant. Low-grade ependymoma can metastasize and treatment should begin immediately. Removal of the ependymoma is generally recommended.
Causes of ependymoma formation
What serves as the driving force for tumor development is not known exactly. Oncologists identify only factors that precede the appearance of a tumor of this type:
- heredity: if close relatives have a history of cancer, the person is at increased risk;
- harmful working conditions: regular exposure of the body to carcinogenic, chemical, nuclear substances contributes to the occurrence of various kinds of diseases, including central nervous system tumors;
- radioactive radiation;
- infection with oncogenic viruses such as herpes, papilloma, etc.;
- poor ecological environment;
- bad habits.
People with reduced immunity and survivors of cancer are also at risk of developing ependymoma.
A comment
Ependymomas of the cauda equina of the spinal cord belong to the group of “extramedullary tumors” and represent a separate pathomorphological subgroup of the so-called myxopapillary ependymomas. An interesting fact is that myxopapillary ependymomas, according to the classification of CNS tumors, belong to absolutely benign tumors (Grade 1) and theoretically should have a better prognosis than intramedullary ependymomas (Grade II) of adults. The clinical series of 197 patients presented in this work clearly demonstrates all the difficulties and problems in the treatment of “invasive” ependymomas of the cauda equina. Indeed, for some reason, a number of myxopapillary ependymomas behave aggressively, infiltrate surrounding structures, recur, and give drop metastases. Unfortunately, the authors did not analyze what factors may influence the “biological behavior” of myxopapillary ependymoma. My experience shows that one of these factors may be the size of the tumor at the time of surgery, which indirectly reflects the timeliness of diagnosis. Thus, with tumors up to 5 cm in length, signs of arachnoid infiltration are almost never observed. Long-term chronic compression of the surrounding neural structures by the tumor for unknown reasons leads to their infiltration. Another factor is the radical nature of the first operation. I have repeatedly operated on patients with so-called “relapse,” which was essentially progression of residual tumor. In such situations, even repeated surgery can be radical and lead to a cure. A large and essentially “unsolvable” problem is caused by giant (5-7 levels) ependymomas with destruction of the dura mater and vertebral bodies. These tumors always infiltrate both the roots, conus, arachnoid, and dura mater, even destroy it and penetrate into the soft tissues. All the patients whom I operated on with such giant tumors were observed for a long time by various specialists, sometimes even with an MRI diagnosis, and “walked” toward surgery for years (and some even decades). Such examples are a clear illustration of the importance of timely diagnosis and early surgical treatment for ependymomas of the cauda equina. A simple delay in surgery for several years turns a potentially treatable condition into an incurable one. The role of radiation therapy in the treatment of infiltrative tumors is rightly noted by the authors. At the same time, I am sure that we should look for improved results of treatment of myxopapillary ependymomas in timely diagnosis and high-quality surgery, and not in adjuvant therapy.
Yu.V. Kushel
(Moscow)
Classification of ependymomas
Today, doctors distinguish four types of tumors of this type according to their etiology and degree of malignancy:
- Mixopapillary type.
A benign neoplasm is located in the lower parts of the spinal cord. It occurs more in adult patients. The prognosis after treatment is favorable. - Sudappendymoma.
A benign formation is located inside the ventricles of the brain, grows slowly, and there are practically no symptoms. Relapses are rare. - Classic type ependymoma.
The most common type of pathology. Recurs frequently and progresses to the next stage. - Anaplastic type - ependymoblastoma.
This type is diagnosed in a quarter of all cases of ependymoma. The malignant tumor grows rapidly and metastasizes in all cases.
In most cases, removal of brain ependymoma is performed.
Discussion
Tumors of the cauda equina are very rare against the background of other neurosurgical pathologies.
Ependymomas of this localization are even less common. The series of patients studied, published in this article, is the largest in the CIS countries and one of the largest in the world. For example, at the Research Institute of Neurosurgery named after. A.P. Romodanova (Kyiv, Ukraine) operated on 62 patients over a 20-year period (from 1988 to 2007) [3]. In most cases, ependymomas located extramedullary do not cause motor deficits unless there is compression of the conus spinal cord. L. Meneses et al. [4], having analyzed a group of patients with cauda equina ependymomas, divided the symptoms into local pain (31.25%), radicular pain (56.25%) and paraparesis (12.5%). A decrease in motor function was noted only in every 10-12th patient in the series and was accompanied by impaired urination, defecation, and sexual dysfunction. At the same time, pronounced local and radicular pain syndrome and sensory disorders caused significant discomfort and were the main reason for disability and visits to a doctor.
Early symptoms of the disease are usually considered to be sensory disturbances in certain sensory areas on one side of the body. Gradually spreading from the level of the tumor down to the feet, sensory disorders become bilateral. This phenomenon progresses along with the increase in tumor size.
Urinary dysfunction, like sexual dysfunction, develops in a small number of patients. The appearance of such symptoms is associated with compression of the conus of the spinal cord. The conus spinal cord includes segments of the sacral plexus, which are responsible for the function of the pelvic organs. In our series of observations, only 4 of 18 patients with dysfunction of the pelvic organs had tumors at the level of the conus spinal cord. The remaining 14 patients with dysfunction of the pelvic organs had a tumor located distal to the conus and, in our opinion, more pronounced symptoms. Thus, in 6 cases, dysfunction was accompanied by urinary incontinence and stool retention. Unfortunately, this manifestation of the disease did not regress during the postoperative observation period after tumor removal, even taking into account the specific therapy performed. This may be due to impaired microcirculation in the roots of the cauda equina caused by long-term compression by the tumor, although we did not find confirmation of this in the literature. It is noteworthy that in most cases (13 patients) when the patient’s pelvic organs were dysfunctional, the tumor had an “infiltrative” growth pattern.
The division of tumors into two types of growth (“infiltrative” and encapsulated), which influence the results of treatment, was carried out in their series by P. Sonneland et al. [2], E.I. Slynko, A.G. Karleychuk [3]. Of course, we were not talking about true infiltrative growth, but about exophytic growth, since cauda equina ependymomas do not grow into surrounding structures. In our practice, we very often observe the inclusion of the roots of the cauda equina into the tumor’s own capsule. Often such ependymomas reach gigantic sizes. Among the patients in our series, 2 had giant ependymomas. Tumors of the cauda equina were large and extended over 7 segments (ThX-SIII) of the spine. These tumors compressed the conus of the spinal cord and occupied all the space inside the membrane, ending in the sacrum. In these cases, destruction of bone tissue was observed, the tumor stretched the presacral fascia and penetrated into the pelvic area (Fig. 8).
Rice. 8. MRI and SCT examination of patient K., 54 years old, with relapse of myxopapillary ependymoma ThXII-LI. The patient underwent surgery at his place of residence in 1988 and 1989, and in 1991 underwent a course of radiation therapy with a dose of 44 Gy.
We examined treatment outcomes reported in large worldwide series of patients. Thus, in the series presented by E. Kucia [5], total removal of ependymomas was achieved in 80% of cases, in the series by M. Nakamura [6] - in 73.4%, according to P. Sonneland et al. [2], radical removal was obtained in only 59% of patients. In a series of patients operated on at the Research Institute of Neurosurgery named after. acad. N.N. Burdenko, total tumor resection in group 1 was achieved in 33 (91%) cases, in group 2 - in 9 (64%). These data certainly indicate a large number of unsatisfactory results among patients undergoing reoperation.
Removing a tumor with an “infiltrative” type of growth, tightly adherent to the roots of the cauda equina, was a difficult task. Total removal of this type of ependymoma was carried out with extreme caution. The basic principle of removal was observed: “maximally safe resection” [2, 5, 9]. During the operations, it was necessary to clearly correlate the degree of radicality of tumor removal and the risk of developing neurological deficits in the postoperative period. To prevent neurological complications, we used neurophysiological monitoring with the study of motor and sensory evoked potentials. The need to use neurophysiological monitoring in their work was emphasized by M. Meneses et al.
According to P. Sonneland et al. [2], tumor recurrences occurred in 19% of cases, according to E. Kucia et al. [5] - 10%, according to E.I. Slynko and A.G. Karleichuk [3] - in 7.4%, M. Meneses et al. [4] did not detect a single relapse in a series of 16 patients with a follow-up period of 2 to 84 months.
According to the national guidelines of the National Comprehensive Cancer Network (NCCN) [9] of 2013, developed in the USA, for the management of patients with primary spinal cord tumors, it is recommended to resort to the most gentle resection (“maximally safe resection”) with follow-up and regular follow-up MRI studies. If continued growth or recurrence is detected, repeat surgery or radiation therapy is recommended. Based on the experience gained, the spinal department of the Research Institute of Neurosurgery has developed tactics for the treatment and observation of patients with extramedullary tumors of the spinal cord (see diagram).
Treatment tactics and monitoring of patients with cauda equina ependymomas.
If a radiologically verified intradural tumor—cauda equina ependymoma—is detected, according to contrast-enhanced MRI, the patient undergoes surgery to remove the tumor. Depending on the radicality of the operation and the histological diagnosis, the tactics for further treatment of the patient are determined. In case of total tumor removal, the patient is recommended to undergo contrast-enhanced MRI at 3, 12, 36 months and 60 months after surgery, regardless of the type of tumor growth, followed by consultation with a neurosurgeon. After subtotal removal or in case of a high risk of recurrence, the patient is consulted by a radiologist and, if necessary, undergoes a course of radiation therapy. For patients in whom tumor recurrence was detected during observation and there is no progression of neurological symptoms, stereotactic irradiation of the tumor is recommended. If neurological symptoms associated with motor or sensory deficits increase, repeated surgery is performed, and radiation therapy in this case is not the method of choice.
In our series, we did not use chemotherapy or targeted therapy to treat patients. However, chemotherapy in the treatment of ependymomas in adult patients is limited and is used in the absence of effect from radiation therapy. In a study conducted by A. Korshunov et al. [10], among 127 patients with anaplastic ependymoma, 44 patients received cisplatin, lomustine and vincrestine. In this study, patients who received chemotherapy had better outcomes in terms of longer disease-free interval and stabilization of tumor growth compared with patients who did not receive therapy (78% vs 48%; p
=0,01).
A number of authors also note the effectiveness of chemotherapy or targeted therapy in patients with continued growth of Grade III ependymoma. Thus, N. Fakharai et al. [11] published a clinical case of the use of imatimab in a patient with continued growth of a cauda equina tumor (Grade II ependymoma), which was observed for 11 months. Regression of neurological symptoms and positive dynamics on MRI in the form of a decrease in tumor volume were noted. Oncologists at Norris Cancer Center, LA, CA, USA achieved good results in the form of stabilization of ependymoma growth [12]. The study involved 10 patients diagnosed with Grade III anaplastic ependymoma, who were treated with etoposide 50 mg/m2 per day daily over 2 cycles of 21 days with a 14-day break. In 5 (50%) patients, a stable, good result was achieved in the form of stabilization of tumor growth. However, the majority of patients in the study group—9 (90%) patients—experienced complications from the gastrointestinal tract and hematopoietic system.
The complex of symptoms inherent in the disease
The following signs of pathology are distinguished:
- severe and chronic headaches;
- dizziness;
- nausea, vomiting;
- impaired coordination of movements;
- unsteadiness of walking;
- difficulty swallowing;
- impairment of auditory and visual functions;
- epilepsy attacks;
- mental retardation (in a child);
- increased intracranial pressure;
- irritability;
- constant feeling of fatigue;
- impaired fine motor skills;
- decreased concentration.
If the tumor has involved nearby tissues, the following symptoms appear:
- sharp and severe back pain;
- gastrointestinal disorders;
- urinary incontinence.
Symptoms vary depending on the location of the tumor.
Signs of ependymoma at different stages
Symptomatic manifestations of the disease are associated with the location of the tumor, its histological shape and aggressiveness.
The initial stages of pathology in children are accompanied by the following symptoms:
- head size increases;
- the child becomes irritable and restless;
- numbness occurs in certain areas of the body;
- appetite disappears;
- vomiting appears;
- urine leaks involuntarily;
- coordination is impaired;
- weakness and lethargy are observed.
Malignant ependymoma in adults is accompanied by:
headaches;- nausea and dizziness;
- memory impairment;
- hallucinations;
- lack of coordination.
Ependymomas of any size, belonging to any histological type, degree of malignancy, lead to serious changes in the body:
- compress the brain structures that are responsible for vital processes occurring in the body;
- cause the development of closed hydrocephalus;
- lead to the spread of metastases along the cerebrospinal fluid outflow pathways and various membranes within the boundaries of the central nervous system, as well as beyond its borders.
Some stage 3 tumors develop rapidly, and there is a need for symptomatic treatment with new generation drugs. Such drugs are always available in oncology clinics in Israel and are actively used in cancer therapy.
Diagnosis of the disease
In order to determine the history of the origin of the pathology, the stage of the disease, the size of the tumor, the neurologist prescribes:
- Computed tomography.
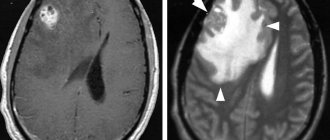
— Magnetic resonance imaging.
- Puncture of cerebrospinal fluid to confirm the diagnosis.
These methods allow you to examine the tumor as accurately as possible. After making a preliminary diagnosis, it is recommended to:
- angiography;
- stereotactic biopsy;
- ultrasonography;
- ventriculoscopy;
- electroencephalography.
MRI and CT are the most modern and effective methods for diagnosing tumors.
New in treatment
New horizons in the treatment of ependymoma have been opened by radiosurgery, which makes it possible to deliver maximum doses of radiation to the tumor while keeping the surrounding brain tissue intact. The most effective methods of radiosurgery today are Novalis, Gamma Knife and Cyber Knife.
The undeniable advantages of radiosurgical treatment include:
- absolute non-invasiveness of the method
- no postoperative complications
- exclusion of anesthesia
- painlessness
- shorter course of treatment compared to traditional radiation therapy
— precise delivery of the prescribed dose of radiation
— safety of irradiation for surrounding organs and tissues.
Radiosurgery methods can be used even in those clinical situations where surgical intervention is considered impossible for one reason or another.
If you or your loved ones have been diagnosed with ependymoma, contact the specialists at Global
Medical today to find out what assistance our Russian-speaking staff can offer you in choosing a medical institution and specialists with positive experience in treating this disease.
Treatment method for ependymoma
Today, the following methods of treating the disease are used:
- Operation
. Surgical removal of brain ependymoma is the main method of treating the pathology. If the formation is malignant, then even complete excision gives a survival rate of no more than five years. The most disappointing prognosis for epindymoblastoma. In our clinic, neurosurgical operations are performed by experienced doctors using new generation equipment and technology.
If the tumor is localized in the posterior cranial fossa, access to it is limited and complete excision is impossible. After surgery, radiation therapy is performed. If the patient is a child, radiation exposure is minimized or replaced with chemotherapy.
- Stereotactic radiosurgery
. Used as an alternative to surgery to treat patients over 14 years of age. Irradiation of the tumor is performed using a CyberKnife. The radiosurgery method is effective for the treatment of myxopapillary tumor and subepindymoma. Impairment of neurological processes may persist after treatment.
- Radiation therapy
. The technique involves influencing the formation of radiological radiation. The main indication for use is localization of the tumor in a hard-to-reach place, and also as an addition to a set of measures after surgery. The advantage of the method is that the radiation is directed strictly to the affected tissues, without the risk of damaging healthy cells, unlike surgery.
You can make an appointment at our clinic using the contact number. Diagnosis, treatment and monitoring of the patient’s condition are carried out by qualified doctors.
Diagnostic methods
Determining the nature of the disease is carried out by a highly specialized specialist - a neurologist. If the first signs of cerebrospinal fluid blockage appear in infancy, the primary diagnostic method is neurosonography performed through the fontanel zone.
A general picture of the electrical conductivity and activity of brain tissue is provided by a diagnostic method such as electroencephalography. It allows you to differentiate tumor processes from other, similar in symptoms, disorders of brain activity. Accompanying signs of pathology require consultation with an ophthalmologist and ENT doctor. The spread of the disease to the spinal structures is determined by taking a lumbar puncture, followed by examination of the cerebrospinal fluid in the laboratory. Only if there is direct suspicion of the described anomaly, a stereotactic biopsy is prescribed, which is designed to show the condition of the cells - ependymocytes.
Neurological symptoms, first epileptic seizures, increase in intracranial pressure are a direct reason for prescribing such hardware diagnostic procedures as:
- Computer scan of the brain. A visualizing radiographic method that helps to study the condition and functionality of an organ. In some cases, it is contraindicated due to the use of ionizing radiation.
- MRI of the head brain. The most effective, informative and preferred method for patients of all age categories. Gives a complete picture of the developed pathology, size, location, malignancy and presence of metastases. All adjacent structures, liquor channels, nerve fibers, and vascular network are visualized. During screening, no radioactive radiation is emitted, which is suitable for young patients and pregnant women.
Magnetic resonance examination is a mandatory diagnostic stage for suspected tumors. Scanning is not carried out in all district clinics, as it requires a high-tech base, modern equipment and trained personnel. You can find the nearest MRI diagnostic center on the unified city service Mrt-v-msk. The website provides a complete list of clinics providing consultations in the desired area. Organizations are ranked by location, rating and prices for scanning services. In addition to general and contact information, on the site you can find reviews for each clinic and leave your own comment.
Booking a time for a session at the selected center is carried out using a single customer service phone number located at the top of the page. Operators will provide complete information about the nearest medical organizations, prices, and make an appointment for a free date and convenient time. Remote consultation and time booking are free of charge.
How is a treatment plan made?
After the final diagnosis, a treatment plan is drawn up. In order to create the most individualized treatment program specifically tailored for a specific patient (risk-adapted therapy), the treating team must take into account certain factors that affect the patient’s prognosis (so-called prognostic factors or risk factors).
Important prognostic factors in children with ependymoma are the specific type of tumor, where exactly it grew, how far it has spread, and whether it has metastasized. Doctors receive this information after a complete diagnosis, which we discussed above. In addition, the age of the child and the general state of his health matter. When drawing up an individual treatment plan, specialists take into account all these factors in order to obtain the most effective treatment result.
Table of contents
- What are ependymomas?
- Where do ependymomas grow and how do they spread throughout the central nervous system?
- How common are ependymomas in children?
- What are the histological types of ependymomas?
- Why do children get ependymoma?
- What are the symptoms of the disease?
- How is ependymoma diagnosed?
- How is a treatment plan made?
- How is ependymoma treated?
- What protocols and registries are used to treat children?
- What are the chances of being cured from ependymoma?
- Additional Information
Main types of ependymoma
Ependymomas are divided into 2 categories:
- Benign tumors.
- Malignant tumors.
Benign ependymomas include:
Tumors develop in the ventricular system of the brain and have the shape of a node. Their structure includes auxiliary cells of the nervous system.
Ependymogliomas or subependymomas.- Papillary ependymomas. Tumors form in the lumbar and sacral areas. Their structure includes cords, plates, villi, and septa.
- True ependymomas. The most common type of benign tumor. Such neoplasms include pathological cells surrounding the channels and vessels.
- Micropapillary ependymomas. Tumors often develop in the cauda equina (the region of the lumbar and sacrum), and the source of their development is the adjacent spinal structures. The neoplasm is capable of melting tissue structures and is characterized by mucous cyst formation. Dystrophic changes occur in the area of tumor development.
Malignant ependymomas are:
- Ependymoblastoma. A rare and aggressive type of tumor that develops from embryonic cells. This neoplasm is typical for children under five years of age. The prognosis for this tumor is not very good; in the absence of adequate treatment for ependymoma abroad, a low survival rate is predicted.
- Anaplastic ependymoma. The tumor is characterized by the third degree of malignancy, which means that the pathology is very dangerous. The tumor quickly metastasizes and produces many immature cells. This type of ependymoma is quite common and requires immediate treatment.
What are the symptoms of the disease?
Just like other brain tumors, the symptoms of ependymoma depend primarily on the age of the child, where exactly in the central nervous system [CNS] the tumor grew and how far it has already spread throughout the body. At the same time, experts talk about general symptoms (nonspecific) and local symptoms of the disease (specific).
Nonspecific general symptoms appear regardless of where exactly the tumor has grown. In general, these symptoms also appear in other diseases that are not related to CNS tumors. For example, a child has a headache and/or back pain, dizziness, loss of appetite, vomiting on an empty stomach in the morning, the child loses weight, begins to get tired faster, his performance decreases, concentration is lost, the child’s personal characteristics change, his behavior changes, there are delays in development.
These symptoms appear when pressure gradually builds up inside the skull and puts pressure on the brain structures. The tumor itself, which is growing, can compress, and/or due to the tumor (as, for example, with medulloblastoma), the circulation and outflow of cerebrospinal fluid (CSF, cerebrospinal fluid) is disrupted. Due to a violation of the outflow of cerebrospinal fluid, the child may develop water on the brain (hydrocephalus). If dropsy appears in infants and young children, when the fontanelles have not yet closed, then their head greatly increases in volume (macrocephaly).
Specific symptoms may indicate where exactly the tumor has grown in the central nervous system and which control centers it is disrupting. For example, if an ependymoma has grown in the cerebellum area, the child’s gait and balance may be impaired. If a tumor grows in the cerebrum, then the child experiences seizures, and if it grows in the spinal cord, then some part of the body is paralyzed in children. If a child has problems with vision, consciousness, or sleep, this may also indicate where the tumor has grown (although these symptoms are often less informative).
Types of ependymoma according to the nature of development
Depending on the growth pattern of ependymomas, there are:
- extramedullary - such tumors develop in tissues that surround the structures of the brain and spinal cord, but do not grow into them;
- intramedullary - tumors can develop around the structures of the spinal cord and brain and grow into them.
The second type of ependymoma is more dangerous. If it is detected, you should contact oncology centers abroad, where specialists will conduct a repeated comprehensive examination and develop an optimal treatment algorithm based on innovative developments.
Clinical symptoms of spinal cord ependymoma
Ependymomas, which are benign in nature, develop slowly. The first signs of the disease appear 1-1.5 times from the approximate start of tumor growth. A person seeks help after about 4-5 years. The severity of symptoms depends on the level of spinal cord damage. The first symptom of the disease is local pain in the spine. Most patients - about 70% - note the intensity of pain when taking a horizontal position. Some categories of patients experience reticular pain.
Sensory disorders manifest themselves in segments. Dyesthesia is expressed by specific pain in the form of sensations of heat or cold in the corresponding limbs. Characterized by disturbances of superficial sensitivity with preservation in deep layers. The development of the tumor entails sensory disturbances, with expansion in the underlying areas. Unilateral or bilateral paresis is recorded, and with progression - central paraparesis, localized below the boundaries of neoplasia, dysfunction of the pelvic organs.
Peripheral failure is accompanied by a decrease in muscle tone and weakening of tendon reflexes. Increased reflexes and muscle hypertonicity indicate the central nature of paraparesis.
Ependymoma in the cervical spinal cord causes dizziness, intense headache localized in the occipital region, hoarseness, coughing attacks, dysphagia, spastic tetraparesis. The initial signs of a tumor in the cauda equina area are pain of the radicular type, localized in the lower limb on the affected side. The progression of the disease leads to bilateral pain. Paresis affects peripheral paresis of the distal parts of the lower extremities. The development of urinary retention is typical.
How common are ependymomas in children?
Ependymomas are very rare tumors. In the group of diseases that experts call “primary tumors of the central nervous system,” they make up only about 10%. Children can get this type of cancer at any age. But most often this type of tumor occurs in children under the age of 3-4 years. The average age of children when they are diagnosed with ependymoma is about 6 years.
In Germany, between 35 and 45 new cases of ependymoma in children and adolescents are reported annually. In other words, out of 1,000,000 children, approximately 3 people get sick. Boys get sick slightly more often than girls (ratio: 1.2:1).
Reasons for the development of the disease
The reasons influencing the development of cancer pathologies are still being studied to this day. Some scientists are of the opinion that ependymoma develops against the background of heterotopy of ependymal cells, which occurs due to partial closure of the neural tube in the initial stage of embryo formation. Others believe that the formation of a tumor is influenced by a complex of factors that can be divided into groups:
- Exogenous. These include the influence of radiation, carcinogenic additives, food and industrial dyes, household chemicals, some metals, and chemicals that pollute the atmosphere. Unfavorable factors have a mutating effect on cells and cause the development of pathological growth.
- Endogenous. Internal factors include decreased immunity against tumor development. Insufficient protection ensures the preservation of the viability of the mutating cells that make up the tumor.
- Hereditary. There is a theory of genetic predisposition to the development of neoplasia. Hereditary predisposition explains familial forms of cancer, predisposition to the pathological development of Recklinghausen neurofibromatosis, and familial polyposis.
Pathogenesis
The cells lining the spinal canal, which form the ependymal lining of the spinal canal, form an ependymoma when they grow uncontrolled. Pathological qualities are acquired by ependymocytes and contribute to increased reproduction. Most often, ependymoma of the spinal cord is benign. The symptoms correspond to a compression effect on the spinal cord due to an increase in the number of tumor cells.
Compression of the spinal cord causes disruption of the functioning of neurons in the injured area. Next, a disturbance of sensitivity develops in the corresponding zones of innervation. In the future, the process is aggravated by paresis. Compression of the pathways leads to extensive denervation of tissues located below the damaged area. Extradural growth leads to tumor growth into the subcutaneous tissue of the suprasacral region. Ependymoma, which is malignant in nature, destroys spinal cord tissue and develops destructively.