If the brain dies, this means the onset of biological death. The death of the tissues that make it up is irreversible. Without neuron signals, the body will not be able to maintain heartbeat and breathing.
In the world, it is customary to distinguish several types of death - biological, clinical, brain death.
Clinical death is considered reversible. Degenerative processes begin to occur, from which a person can die, but there is still a chance to restore the vital functions of the body. If the outcome is favorable, you can fully regain your health and continue to live a full life. In this case, necrosis of tissues and organs does not occur.
Biological death is associated with the death of all organs and systems. This process is already irreversible, as neuronal damage and necrosis are observed. Vital functions are completely lost, death occurs.
What are the criteria for brain death? It is associated with the death of neurons. If the brain dies, this process is also irreversible. The body is no longer able to maintain vital functions; the respiratory and cardiovascular systems do not work. This is analogous to biological death. When brain death occurs, necrosis of its tissues is necessarily observed.
Sometimes brain decortication is performed - partial surgical removal of the cortex. Such a serious operation is performed only for special indications.
Causes
Brain death can be caused by different reasons, but they trigger the development of the same pathological processes. Blood circulation is impaired, and this dysfunction is persistent. This provokes acute oxygen starvation, which causes metabolic products to stagnate in the tissues. Irreversible brain damage develops.
The main reasons are as follows:
- diseases, including inflammatory processes in brain tissue;
- injuries;
- circulatory disorders (hemorrhagic or ischemic stroke);
- multiple organ failure;
- poisoning (alcohol, lithium, drugs);
- tumor (cancer causes numerous tissue destructions);
- heart diseases, etc.
The phenomenon of vascular occlusion is extremely dangerous. At the same time, their patency is impaired, and oxygen starvation of the tissues occurs. Occlusion of arteries and veins that lead to the brain is especially dangerous. Often, pathological anatomy of the deceased reveals complete blockage of blood vessels. This can be a consequence of injury, disease and causes damage to neurons.
The brain stem may be damaged primarily or secondary. With a primary lesion, direct damage occurs (if there is a fracture of the base of the skull, the functions of the trunk itself are impaired). In case of secondary damage, the trunk suffers due to the resulting edema and dislocation syndrome. With swelling, the tissue begins to protrude strongly through the opening of the back of the head, due to which the trunk is excessively compressed, blood circulation stops and necrosis begins. This is why protecting the brain from swelling is so important.
All of the above reasons are considered extreme; they have an extremely negative effect on neurons. The brain stem and its cortex are primarily affected. The task of the trunk area is to maintain cardiac activity, breathing, control blood pressure, and the cortex is responsible for thought processes, consciousness, etc.
Cardiac arrest does not immediately lead to brain death, but everything happens very quickly. A person without blood circulation can live only a few minutes. 3 minutes without blood supply can lead to irreversible death of neurons, resulting in coma. If the cerebral cortex has died, vital functions will be lost and death can occur almost immediately.
The time that the body can survive without cardiac activity is influenced by a whole range of factors:
- age;
- general condition of the body;
- presence of diseases;
- the reason that caused this condition;
- ambient temperature, etc.
After just three minutes of oxygen starvation, neurons begin to die. This is an irreversible process, since dead tissue is not restored. In a healthy young person, brain death may slow down slightly. If the ambient temperature is low, the brain will die more slowly. If resuscitation is performed correctly at this time, the person can be brought back to life.
The consequences of circulatory arrest can be unpredictable. Sometimes a person wakes up from a coma, blood supply to the brain is restored, but it turns out that a significant part of the neurons have already died. If the brain dies, but the heart works, it will no longer be possible to return the victim to normal life. He can only exist, and is not even able to breathe on his own.
Stages of diagnosing brain death
To accurately determine whether the brain is alive or whether irreversible and incompatible changes have already occurred in it, clear recommendations have been developed that should be followed by every specialist who encounters a patient in serious condition.
Diagnosis of brain death includes several stages:
- Accurate determination of the cause of the pathology.
- Exclusion of other brain changes that are clinically similar to his death, but under certain conditions can be reversible.
- Establishing the fact of cessation of activity of the entire brain, and not just its individual structures.
- Accurate determination of irreversibility of brain damage.
Based on clinical data, a doctor has the right to make a diagnosis of brain death without using additional instrumental diagnostic methods, since the developed criteria make it possible to determine the pathology with absolute accuracy. However, in our time, when the conclusion about any disease is based on a variety of objective results, instrumental and laboratory tests are involved in the diagnostic process.
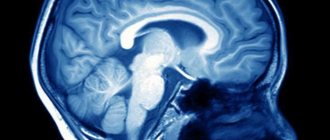
brain perfusion on MRI is normal (left), with brain death (center), with a vegetative state (right)
Additional examinations are not excluded from diagnostic algorithms for brain death, but are not strictly required. Their purpose is to speed up the establishment of the fact of brain death, especially in clinically complex cases, although it is quite possible to do without them. In Russia, only electroencephalography and angiography of the carotid and vertebral arteries are allowed as the only reliable ones in determining signs of irreversibility of brain disorders.
Symptoms
The following symptoms indicate brain death:
- there is no consciousness, and this process is persistent;
- there are no reactions to tingling, stroking, handling, no tactile sensitivity;
- no movement of the eyeballs;
- the heart has stopped, as evidenced by a straight line on the ECG;
- there is urinary and fecal incontinence;
- breathing is impaired, the chest does not rise.
Determining whether a patient has died is an extremely important task. Doctors do not immediately diagnose death. Even if all of the listed signs are detected, the person is monitored in the hospital for up to 12 hours. Sometimes, although rarely, signs of brain activity may appear. If during this time the patient does not react in any way, there are no trunk reflexes, then biological death can be stated.
It is important how the brain dies, what triggered the death of neurons. If poisoning has led to such serious consequences, the patient should be monitored for at least a day. If the cause is TBI, the observation time is reduced to 6 hours. The specific decision must be made by the neurosurgeon. It is important that the doctor monitors the patient from the onset of this condition, then he will have a complete picture of events that will allow him to make the right decision.
The onset of biological death is determined exclusively by a neurologist. It is based on subjective and objective criteria. If signs of brain death are clearly identified, the person must be disconnected from life support. This difficult decision is especially difficult to make if the disaster happened suddenly. Often relatives are literally horrified by such a message. If a person is sick for a long time, his loved ones eventually become at least a little accustomed to the idea that their loved one will be gone. In any case, this decision is very difficult.
How long does the brain live after cardiac arrest?
Most studies have shown that the process of brain activity after the heartbeat stops is individual for each person. Although the cessation of oxygen flow is almost instantaneous, there is no specific duration of clinical death at which a functioning brain clearly dies. The most vulnerable cells are neurons, which suffer fatal damage in just 10 minutes without oxygen. However, the damaged cells do not actually die for a very long time. If resuscitation is successful, some areas may resume operations. Find out more. what happens to the brain at the moment of cardiac arrest can be found here - https://reactor.space/news/chto-proisxodit-s-mozgom-v-moment-ostanovki-serdca/.
Diagnostics
When diagnosing, the doctor must collect anamnesis. He must find out how long ago the patient fell into such a dangerous state, under what conditions he lost consciousness, and whether he had speech or motor activity. It is important to know what event preceded the loss of consciousness. An examination is carried out by a neurologist, he necessarily assesses the patient’s level of consciousness and checks his reflexes.
It is extremely important that the doctor excludes all those factors that can cause simulated brain death. It is sometimes caused by severe poisoning, including drugs. For this reason, a toxicological analysis is prescribed. It will help detect toxins or drugs that mimic the appearance of death.
Body temperature must be measured. If the temperature is below 32.2°C, it may distort the picture and show a false death. In this case, the person may be alive, but tests will show the opposite, since physiological processes literally freeze from the cold.
A blood test is prescribed that will help determine whether the metabolism is disturbed, whether there is hormonal dysfunction, and at what level the glucose levels are.
To correctly diagnose brain death, inpatients resort to instrumental research:
- encephalogram (EEG);
- contrast study of cerebral vessels;
- test with irritation of the eardrums (ice water is dripped onto them through the ear canal);
- apneic oxygenation test.
Oxygen starvation is extremely destructive for neurons, even if it is not long-term. Literally after a few minutes of complete lack of oxygen supply, tissues begin to die. The electroencephalogram in this case will show a zero line. This means that there is no brain activity at all.
Encephalography examines brain activity. In this case, the device registers biocurrents, their work is reproduced on paper in the form of curves.
The diagnostic protocol also includes the study of cerebral vessels using a contrast agent. It cannot always be accomplished, as there may be financial restrictions, and sometimes there is simply no equipment. The essence of the test is that a contrast agent is injected, which enters the brain vessels through the bloodstream and identifies possible areas of necrosis. If the brain is dead, the substance does not enter its vessels. This is one hundred percent confirmation of death.
Apneic oxygenation involves temporarily removing the patient from a ventilator. The goal is to observe whether spontaneous respiratory movements have appeared. The monitor monitors the level of carbon dioxide in the blood. It is carbon dioxide that stimulates the body to produce breathing movements. If after 8-10 minutes breathing does not appear, and the level of CO2 in the blood jumps by 20 mm Hg. Art. higher than the original, we can definitely talk about death.
Brain death
1. Introduction
Brain death is the irreversible loss of function of the central nervous system, including the cerebrum, brainstem, pons, midbrain, and cerebellum.
The diagnosis of “brain death” is established with a beating heart and artificial ventilation and is the equivalent of human death.
The most common causes of brain death:
- severe traumatic brain injury;
- massive aneurysmal subarachnoid or intracerebral hemorrhage;
- extensive ischemic cerebrovascular accident with edema and dislocation of the brain;
- massive cerebral edema with fulminant liver necrosis;
- hypoxic and ischemic brain damage during prolonged cardiopulmonary resuscitation or asphyxia.
Brain death after restoration of blood circulation during cardiopulmonary resuscitation develops during the first week from the moment of circulatory arrest, which in some cases may be preceded by a period of initial improvement in neurological symptoms.
2. Conditions necessary to make a diagnosis of brain death
The decisive point in diagnosing brain death is proof of the complete and irreversible cessation of brain function, which requires:
2. 1. Determine what is the cause of brain damage, and whether it can lead to a complete and irreversible loss of its function.
2. 2. Exclude all potentially reversible conditions with similar clinical manifestations.
These conditions are:
- Hypothermia.
- Hypotension.
- Effect of alcohol, sedative drugs, muscle relaxants
- Severe electrolyte and hormonal disorders, acid-base imbalances, hypoglycemia.
The diagnosis of brain death cannot be established if:
- body temperature below 32.2 degrees Celsius,
- mean arterial pressure less than 55 mm. rt. Art. In case of hypotension, blood pressure is maintained by replenishing the volume of circulating blood and adrenergic agonists.
- the presence in the blood of toxic concentrations of sedatives, narcotic drugs, alcohol, muscle relaxants. At subtherapeutic doses, the decision is made in accordance with the clinical situation.
2. 3. Determination of brain death is based on the results of repeated clinical examinations of the patient. Only cerebral angiography demonstrating lack of filling of the internal carotid and vertebral arteries above the level of entry into the cranial cavity can be the basis for a diagnosis of brain death. All other instrumental diagnostic methods are of an auxiliary nature and serve to shorten the observation period.
3. Clinical signs of brain death
3. 1. Lack of consciousness. 3. 2. Lack of motor reactions in response to painful stimuli. 3. 3. Absence of brainstem reflexes. 3. 4. Apnea.
4. Instrumental studies confirming the diagnosis of brain death
4. 1. Electroencephalography (EEG).
Conducted according to generally accepted standards. A minimum of 8 leads are used. The distance between the electrodes is at least 10 cm, the impedance is in the range of 100-10000 Ohms. Recording is carried out with a time constant of at least 0.3 seconds. with a sensitivity of no more than 2 µV/mm (the upper limit of the frequency bandwidth is not lower than 30 Hz). The electrical silence of the cerebral cortex under these conditions should remain for at least 30 minutes of continuous recording. If there is doubt about the electrical silence of the brain, repeated EEG registration is necessary. Assessment of EEG reactivity to light, loud sound and pain: the total stimulation time with light flashes, sound stimuli and painful stimuli is at least 10 minutes. The source of flashes, fired at a frequency of 1 to 30 Hz, should be located at a distance of 20 cm from the eyes. Intensity of sound stimuli (clicks) -100 dB. The speaker is located near the patient's ear. Stimuli of maximum intensity are generated by standard photo and sound stimulators.
4. 2. Cerebral hagiography
Contrast double panangiography of the four main vessels of the head (common carotid and vertebral arteries) is performed with an interval of at least 30 minutes. Mean arterial pressure during angiography should be at least 80 mm Hg. Art. If angiography reveals that none of the intracerebral arteries are filled with a contrast agent, then this indicates cessation of cerebral circulation.
4. 3. Nuclear magnetic resonance angiography
The research in its information content is close to classical angiography. Demonstration of the absence of blood flow in the main cerebral arteries can serve as confirmation of brain death.
4. 4. Transcranial Doppler ultrasonography
A bilateral study is carried out. The sensor is applied in the area of the temporal bone above the zygomatic arch. The diagnosis of brain death is confirmed by the absence of diastolic and reflected blood flow, with the presence of small systolic peaks at the beginning of systole. The complete absence of blood flow is not a reliable sign, as it may be associated with technical problems during Doppler ultrasound.
4. 5. Cerebral scintigraphy.
Confirmation of brain death is the absence of accumulation of the isotope in brain tissue.
5. Algorithm for declaring brain death
To determine brain death, all of the following questions must be answered positively:
5. 1. Is the cause of coma known and can it lead to complete and irreversible loss of brain function?
Coma of unknown etiology (no signs of injury, stroke, hypoxic or hypotensive damage) requires a detailed examination before declaring brain death.
5. 2. Is it possible to exclude the effect of alcohol, sedatives, drugs, muscle relaxants, hypothermia, hypotension, hypoglycemia, electrolyte, hormonal disorders as the cause of the coma and the results of the neurological examination?
5. 3. Can all existing movements be attributed to spinal reflexes?
The diagnosis of brain death cannot be established by adopting any specific posture (decerebrate or decortication), the presence of trembling, or defensive movements of any limb or head in response to pain. The motor response to pain upon irritation of the supraorbital region and compression of the nail phalanges by a hard object is studied.
5. 4. Is there no reaction of the pupils to light?
The reaction of the pupils to bright light should be absent on both sides. Round, oval, or irregularly shaped pupils are compatible with a diagnosis of brain death. In most cases, during brain death, the pupils are in the middle position, their size is 4-6 mm, but the diameter of the pupils can range from 4 to 9 mm. Dilated pupils are compatible with the diagnosis of brain death because the innervation of the radial muscle fibers of the iris by the cervical sympathetic nerves is preserved.
5. 5. Is there no corneal reflex?
5. 6. Are oculocephalic and oculovestibular reflexes absent?
The oculocephalic reflex is not examined in the presence or suspicion of traumatic injury to the cervical spine. To assess it, the patient’s head is turned 90 degrees to one side and held in this position for 3-4 seconds. , then in the opposite direction for the same time. If, when turning the head, no eye movements occur, and they firmly maintain a median position, this indicates the absence of oculocephalic reflexes.
To study the oculovestibular reflex, a bilateral caloric test is performed. Before performing this procedure, it is necessary to ensure that there is no perforation of the eardrums. The patient's head is raised 30 degrees above the horizontal level. A small catheter is inserted into the external auditory canal, and the external auditory canal is slowly irrigated with cold water (50 ml at 0 degrees Celsius). When the function of the brain stem is preserved, a deviation of the eyes in the direction of irritation appears. The absence of nystagmus or deviation of the eyeballs during a caloric test for 1 minute indicates the absence of an oculovestibular reflex. The test on the opposite side is carried out no earlier than 5 minutes after the first.
5. 7. Are cough and pharyngeal reflexes absent?
The presence of cough and pharyngeal reflexes is determined by irritation of the posterior wall of the pharynx and aspiration of tracheal contents.
5. 8. Is there any spontaneous breathing?
The test for absence of spontaneous breathing requires special care to prevent hypoxia and possible complications. It is carried out only after all other data confirming brain death have been received. The necessary conditions:
- Body temperature is at least 36.5 degrees Celsius.
- Systolic blood pressure is at least 90 mm. rt. Art.
- Normovolemia (positive fluid balance during the 6 hours preceding the test)
- Eucapnia is the partial pressure of carbon dioxide in arterial blood (PaCO2) before the test is at least 40 mm. rt. Art.
- The level of partial pressure of oxygen in arterial (PaO2) blood is at least 200 mm. rt. Art.
Test technique:
- Before starting the test, PaCO2 and PaO2 levels are measured.
- The endotracheal (tracheostomy) tube is disconnected from the breathing circuit of the ventilator.
- An oxygen flow of 6 l/min is supplied to the patient's respiratory tract through a catheter. The optimal position of the catheter is at the level of the carina.
- Careful monitoring of the presence of respiratory movements of the abdominal and chest muscles is carried out for 8 minutes.
- After which the levels of PaCO2 and PaO2 are re-monitored.
- If there are no respiratory movements and the PaCO2 level increases to 60 mm. rt. Art. or more, or increases by 20 mm. rt. Art. in relation to the initial level, the test result is considered positive.
- If during observation the blood pressure decreases, arrhythmia develops, hemoglobin saturation drops sharply, arterial blood is drawn and the test is interrupted. It can be considered positive if PaCO2 increases to 60 mm. rt. Art. or more, or increases by 20 mm. rt. Art. relative to the original level.
- If there are no respiratory movements, but the PaCO2 value does not reach 60 mm. rt. Art. — the duration of the test can be increased to 10 minutes.
5. 9. The diagnosis of brain death is established when one of the following conditions is met:
- Positive answers were received to questions 5. 1. -5. 7. with two clinical examinations carried out at least 6 hours apart, and the apnea test (point 5. 8.) confirms the diagnosis of brain death.
- Positive answers were received to questions 5. 1. -5. 7. with two clinical examinations carried out at least 2 hours apart. An EEG study demonstrates the absence of electrical activity in the brain, and the apnea test (point 5.8.) confirms the diagnosis of brain death.
- Positive answers were received to questions 5. 1. -5. 7. with two clinical examinations carried out at least 2 hours apart. An instrumental study (one of those listed in paragraphs 3. 2. - 3. 5.) demonstrates the absence of cerebral blood flow and an apnea test (paragraph 5. 8.) confirms the diagnosis of brain death.
- In the case where the answers to not all questions are 5. 1. -5. 7. may be received (for example, due to extensive trauma). The diagnosis of brain death can be established on the basis of two clinical examinations, carried out at least 2 hours apart, giving positive answers to all tests (5.1. -5.8.), which are possible. The results of one of the instrumental studies (item 3. 2.. -. 3. 5.) confirming the absence of cerebral blood flow and a positive test for apnea.
Responsible for diagnosing a person’s death are the doctors who determined brain death at the medical and preventive institution where the patient died.
If the body is accidentally discovered
If an ambulance team finds a victim without signs of life, doctors have no information how long he remains in this condition. In the absence of cadaveric spots, doctors cannot confirm in the field that biological death has occurred. In this case, resuscitation is mandatory.
Resuscitation measures include artificial ventilation of the lungs and closed heart massage. If there is bleeding, it is important to stop it so the victim does not bleed out. Damage to a large artery or head is extremely dangerous. If resuscitation measures are carried out correctly, a person can be brought back to life.
After diagnosis...
Once brain death has been confirmed by all clinical data, doctors have three options. In the first case, they can invite transplantologists to decide on the issue of organ collection for transplantation (this mechanism is regulated by the legislation of a particular country). In the second, talk to your family, explain the essence of the pathology and the irreversibility of brain damage, and then stop artificial ventilation. The third option, the most economically unprofitable and impractical, is to continue maintaining the functioning of the heart and lungs until they decompensate and the patient dies.
***
The problem of brain death with intact cardiac activity is not only of a medical nature. It has a significant moral, ethical and legal aspect. Society as a whole knows that brain death is identical to the death of the patient, but doctors have to make serious efforts, tact and patience when talking with relatives, deciding on transplantation issues and determining the final option of their actions after making a diagnosis.
Unfortunately, cases of distrust in doctors, unjustified suspicions of unwillingness to continue treatment, and accusations of negligence in their duties are still common. Many people still think that with a superficial assessment of the patient’s condition, the doctor will simply turn off the ventilator without making sure that the pathology is irreversible. At the same time, delving into the diagnostic algorithms, one can imagine how long and difficult the path to the final diagnosis is.
How to tell your family
Recently, it has become common to resort to the help of a psychologist in such cases. It will help family members come to terms with their loss.
Making a decision to disconnect a patient from life support is extremely difficult even for experienced doctors. Relatives are always unprepared for such a tragic development of events, so they literally lose their minds. Relatives tend to believe that they can still try to do something. They are often asked to wait at least a few days. If there is accurate evidence of brain death, the doctor must find the right words to explain the current situation to the relatives.
According to the rules of bioethics, if brain death is definitely established, the patient should be disconnected from devices that support life processes. There is no point in expecting him to come back to life if all tests have confirmed the absence of neuronal activity. This will be a humane decision.
Relatives should definitely ask what diagnostic research methods were used. The doctor must show a document confirming the established brain death. Only relatives have the right to decide to disconnect the victim from life-sustaining devices. The doctor’s task is not to succumb to emotions, but to make the right decision based on the specific results of the patient’s examination.
It is important to exclude the human factor and rely only on test results.
How long to keep the victim on life support is decided individually in each case. After a person is disconnected from the devices, Lazarus syndrome may occur. It consists in the fact that the deceased experiences individual muscle twitches. The head may turn involuntarily, the person may bend an arm or leg. It even happens that an already dead person arches. This is the result of contraction of the back muscles. It is important that the doctor warns the patient’s relatives in advance that such manifestations are possible. This does not mean that the victim comes to life.
Additional examinations
Of the additional examinations that may affect the diagnosis, electroencephalography (EEG) and angiography are permitted. EEG is indicated for those patients for whom it is difficult to determine reflexes - in case of injuries or suspected injuries of the cervical spinal column, ruptured eardrums. An EEG is performed after all tests, including apnea. In brain death, it shows the absence of any electrical activity in the nerve tissue. If the indicators are questionable, the study can be repeated or using stimuli (light, pain).
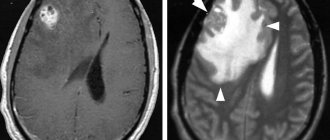
non-collapsed cerebral vessels are normal on angiography
If EEG is indicated in clinically complex cases and does not affect the duration of general observation, then panangiography of the carotid and vertebral arteries is designed to shorten this time as much as possible. It is carried out at the final diagnostic stage and confirms the irreversibility of the cessation of brain activity.
For example, in case of possible intoxication, the patient should be observed for at least three days, but brain death can be determined early if, immediately after the appearance of signs of loss of its functions, the main arteries of the brain are examined twice with an interval of at least half an hour. In the absence of contrasting of the arteries, we can talk about a total and irreversible stop of cerebral blood flow, and further observation becomes impractical.
Video: example of an EEG to confirm brain death
Clinical diagnosis of biological brain death is labor-intensive, requires constant monitoring and maintenance of vital functions, so for many years the search has been underway for another method that would allow us to establish a reliable diagnosis with no less accuracy than the clinic. However, no matter how hard the experts try, none of the proposed methods is comparable in accuracy and reliability to a clinical assessment of the state of the brain. Moreover, other techniques are more complex, less accessible, invasive or not specific enough, and the result is greatly influenced by the experience and knowledge of the doctor.
The desire to speed up the process of ascertaining brain death is largely due to the rapid development of a new branch of medicine - transplantology. Considering the diagnosis of brain death from this position, we can say that the price of a conclusion about brain death may be not one, but several lives - both of the potential donor and of other people in need of organ transplants, therefore haste or non-compliance with the observation algorithm is unacceptable.
When deciding to declare brain death, the doctor must remember the ethical side of the issue and the fact that the life of any person is priceless, therefore strict compliance of his actions with the established rules and instructions is mandatory. A possible mistake increases the already high degree of responsibility, forcing you to repeatedly play it safe and doubt, double-check and weigh every step.
The diagnosis of brain death is established jointly by a resuscitation specialist and a neurologist, and each of them must have at least five years of work experience. If additional examination is necessary, specialists of other profiles are involved. Transplantologists and other persons involved in the collection and transplantation of organs cannot and should not participate in or influence the process of diagnosing brain death.
Consequences
Brain death does not always lead to biological death. Sometimes medical intervention can save a life, if such a condition can be called that. In fact, after brain death, only certain vital functions can be maintained. The consequences of total neuronal death are terrible, this is complete dementia. Any vital indicator is so low that the body cannot cope without the support of devices. Such people are no longer able to continue living a full life. They live like plants and can die at any moment.
Even in order to maintain basic vital functions, continuous administration of medications will be required. Without medical equipment, the patient will not be able to breathe, and his heart will not be able to beat.
In the medical literature there are several descriptions of a case of a person returning to life after death. There is some confusion here. Most likely, such patients “resurrected” after clinical death, rather than biological death. This happens quite often. Clinical death can occur with serious damage, and with proper care, body functions are restored.
Even clinical death is not identical to brain death. It is the death of neurons that leads to the most tragic consequences.
Why does the brain need oxygen?
Gray matter makes up only 2% of body weight, but it uses about 20% of oxygen. Without it, the brain cannot perform even the most basic functions. The brain relies on glucose to stimulate neurons that control everything from conscious functions like planning and thinking to automatic, unconscious processes like heart rate and digestion.
Without oxygen, the cells of this organ cannot metabolize glucose and therefore cannot convert glucose into energy. When your brain is deprived of oxygen, the ultimate cause of brain death is insufficient energy to fuel the cells.
Reanimation
The consequences of brain death are irreversible. Just because a person is unconscious does not mean that he needs to perform resuscitation measures (ventilation, cardiac massage).
Cardiac massage is strictly contraindicated if the victim’s heart is beating, even abnormally. In this case, massage can, on the contrary, interfere with the correct contraction of the heart muscles.
Mouth-to-mouth or mouth-to-nose breathing, as well as chest compressions, are performed only if there is no heartbeat. Such events can save a person's life. If you ensure the supply of oxygen to the body and improve blood circulation, irreversible necrotic changes will not occur. Body functions can be completely restored.
If a pregnant woman is injured, it is important to monitor not only her vital signs, but also the condition of the fetus. The patient must be taken to the hospital as quickly as possible, since the child may die due to injury and stress.
It is extremely important to thoroughly master resuscitation techniques. Any of us can master them and, if necessary, save a person’s life.
Forecasts
Clinical death does not always mean that the patient will definitely die. Sometimes doctors manage to bring a person out of a state of clinical death. The prognosis will be influenced by what circumstance led to such a condition and what resuscitation measures were taken. The main condition is to restore blood circulation in the first 3-5 minutes. Sometimes resuscitation is carried out for up to 20-40 minutes.
Even if partial extinction and death of neurons has occurred, the functions of the medulla can be restored. If biological death or brain death is established, it is impossible to bring the patient back to life, you need to come to terms with this.
The peculiarity of the human brain is that it strives to preserve its functions by any means. If some neurons die, their tasks can be redistributed to other zones. Patients who have suffered a stroke, ischemia, and even serious TBI often return to a full life.
Features and criteria for declaring brain death
In medicine, the concepts of clinical and biological death refer to the entire body, implying the reversibility or irreversibility of changes occurring. Applying this parameter to nervous tissue, we can speak of clinical brain death in the first 5 minutes after breathing stops, although the death of cortical neurons begins already in the third minute. Biological death characterizes a total disorder of brain activity that cannot be reversed by any resuscitation or treatment.
The need to assess the state of the brain usually arises in comatose and similar conditions, when the patient is unconscious, contact with him is impossible, hemodynamics and heart function may be unstable, breathing is usually supported by a device, the pelvic organs are not controlled, there is no movement and sensitivity, reflexes and muscle tone fades away.