Home > Cancer treatment in Israel > Treatment of meningioma in Israel
Meningioma is a tumor that develops from the membranes covering both the brain and spinal cord. In terms of frequency, it ranks first among benign intracranial neoplasms – it accounts for 25% of all diagnosed cases. As a rule, the tumor is characterized by a slow growth rate, and it can be localized in different parts of the nervous system due to the fact that the meninges cover both the brain and the spinal cord.
Typically,
patients have one primary focus of meningioma , but in rare cases, tumors form in several parts of the central nervous system
.
Most often, meningiomas occur in women aged 40 to 70 years, but men over 35 years of age also suffer from the pathology. As a rule, the disease is diagnosed accidentally, during a test for another reason, or when the formation significantly increases in size and the symptoms become severe. There are 3 types of meningiomas: benign, atypical and malignant. Benign meningiomas do not invade surrounding tissue, grow slowly and in many cases do not require treatment, but only regular monitoring. Atypical and malignant meningiomas - they account for about 5-10% of the total - are characterized by rapid infiltrative growth. It is malignant types of meningioma that are more common in men.
Malignant tumors are mainly localized in:
- cavernous and parasagittal sinuses;
- pyramid of the temporal bone;
- wings of the sphenoid bone;
- foramen magnum;
- cerebral hemisphere zone;
- tentorial notch;
- cerebellopontine angle.
Malignant meningiomas require immediate medical attention at the first signs of the disease.
To ensure an accurate diagnosis and receive the most effective medical care, you need to choose the right clinic. Israeli clinics are among the leading cancer centers in Europe: the best oncologists and neurosurgeons are gathered here, and all conditions for a comfortable stay are created for patients. Israel also attracts medical tourists due to the affordable cost of medical care combined with the opportunity to undergo a full examination, therapy and rehabilitation in one medical facility. You can evaluate the benefits of our clinic’s offers by sending an online request or contacting us at the phone number indicated on the website.
Consult an Israeli specialist
Causes of the disease
The reasons for the formation of tumors and their transformation into malignant lesions have not been clearly established. However, doctors are aware of the negative impact of certain factors that increase the risk of meningioma. Among them:
- unfavorable family history, in particular, the presence of multiple hemangiomatosis or neurofibromatosis in close relatives;
- being female - the female body produces hormones that contribute to the development of tumors;
- age over forty years;
- exposure to radiation, both in high and low doses. The risk of meningiomas is increased in patients who have previously received radiotherapy for brain tumors.
In the majority of patients, with timely and adequate treatment, which consists of radical removal of the meningioma, their health is completely restored, and relapses are extremely rare. The likelihood of relapse is high in patients with malignant meningiomas and tumors growing in the area of the venous sinuses, which makes their removal difficult.
Meningioma is not a brain tumor because it is formed from its membrane. At the same time, by squeezing brain tissue as it grows, it can cause symptoms characteristic of brain tumors
.
Characteristics of the neoplasm
As with most other benign tumors, meningioma is characterized by:
- the presence of a hard round or horseshoe-shaped capsule in the patient;
- displacement of nearby brain substructures;
- meningioma cells are as similar as possible to healthy ones;
- the tumor grows slowly;
- there is no tendency to form metastases.
In the case of significant spread of arachnoid endoteoioma, the bone tissue is deformed and enlarged. Meningioma of the brain becomes noticeable visually. Most often the tumor is localized in places:
- on the cerebral hemispheres;
- in the cranial fossa (posterior, anterior, middle);
- in the tentorium of the cerebellum;
- in the area of the temples.
The neoplasm is most often fused to the membrane of the brain.
Symptoms and treatment of brain meningioma
In the initial stages, most meningiomas are completely asymptomatic. Signs of the disease appear when the tumor grows, compresses the brain or spinal cord and interferes with normal blood circulation. In such situations, the following may occur:
- pressing headache that worsens at night or in the morning;
- visual disturbances (double or blurry vision);
- memory impairment;
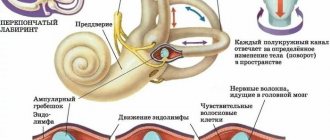
- hearing loss, ringing in the ears;
- loss of smell;
- convulsions;
- weakness or partial paralysis of the limbs;
- change in emotional state (depression, euphoria).
With a certain localization of meningiomas, more specific symptoms are noted:
- in the area of the tubercle of the sella turcica – a sharp deterioration in vision;
- in the temporal lobe – visual and hearing impairment;
- in the area of the tentorium cerebellum – coordination and movement disorders;
- in the convexital area – epileptic seizures.
If you notice one or more neurological symptoms in yourself, your spouse or a relative, do not delay getting tested. Moreover, in our clinic it will take only a few days for a doctor’s consultation, diagnostic measures and preparation of an individual treatment program.
Help is needed? Doctor online. Consultation is free+972-52-651-26-54
Help is needed? Doctor online. Consultation is free+972-52-651-26-54
Discussion
Minimally invasive keyhole approaches
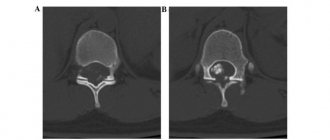
With the development of navigation systems, endoscopes, as well as microsurgical instruments and aspirators, the concept of keyhole surgery is becoming increasingly popular for the removal of a wide range of tumors, including meningiomas [21, 22]. The concept of keyhole surgery is based on the fact that even with a small craniotomy, the significant depth of the surgical wound creates an adequate overview (Fig. 7).
Rice. 7. Schematic representation of the trajectory for the supraorbital trans-eyebrow approach (indicated by arrows) and the corresponding access areas (marked in yellow). The anterior sections of the anterior cranial fossa on the side opposite to the access are a “blind spot”. As keyhole microsurgery has improved, it has become increasingly popular among neurosurgeons, and its use is gradually increasing in comparison with traditional approaches to the anterior and anterolateral parts of the skull base.
Supraorbital trans-eyebrow approach
Classic neurosurgical approaches to the skull base, such as Dandy's macrosurgical frontotemporal and Yasargil's microsurgical pterional, are well described in the literature. Their safety and effectiveness are widely known both from scientific publications and from everyday clinical practice [23, 24]. However, these approaches require extensive manipulation of tissue and bone structures, which can lead to the formation of rough scars, bone defects, atrophy of the temporal muscle, and cause pain when chewing [25]. In view of this, a supraorbital trans-brow approach was developed, which allows approaching intracranial formations with a minimal skin incision, minimal soft tissue trauma and minimal impact on bone structures. Despite the fact that the surgical corridor with the supraorbital trans-eyebrow approach is narrow in both the vertical and horizontal directions, most tumors of the anterior cranial fossa and parasellar region can be easily removed through it [3, 4, 18, 26]. In addition, in experienced hands, this approach increases the efficiency of the operation, reducing intraoperative blood loss and operative time [27].
The technique of the supraorbital trans-eyebrow approach has been improved over the past 20 years. Its safety and effectiveness have been demonstrated in both adults [28] and children [29]. The approach is used for a wide range of pathologies, including aneurysms, cavernomas, meningiomas and optic nerve compression.
As a result of a review of literature data [18, 27, 30-35] on the supraorbital trans-eyebrow approach over the past 20 years, 8 articles were found, represented by large series of publications (a total of 2783 patients, 2508 aneurysms and 577 (19%) tumors).
The main types of tumors were meningiomas, gliomas, and metastases. The main locations of tumors were the anterior cranial fossa, suprasellar region, interpeduncular cistern, anterior and medial parts of the temporal lobe.
Of the 577 tumors removed, data on the radicality of the removal were presented in 238 (41%) cases. Of these, total removal was achieved in 215 (90%) cases, subtotal - in 17 (7%), partial - in 6 (3%).
The most common location of aneurysms clipped from this approach was anterior cerebral–anterior communicating artery aneurysms (31%). In the remaining cases, aneurysms of the bifurcation of the middle cerebral artery (26%), internal carotid artery (20%), basilar artery and superior cerebellar artery (23%) were encountered. Despite cases of intraoperative rupture, no difficulties in controlling bleeding due to access were noted; in 97% of patients, complete exclusion of the aneurysm from the bloodstream was achieved [18, 27, 32-35].
According to the literature, it was established that complications arose when access was performed inappropriately. The most common complications were temporary accumulation of cerebrospinal fluid under the skin flap and decreased sensitivity in the frontal region on the access side - temporary in 1.6% of cases and permanent in 4.3%. These complications occur in approximately 1 in 20 patients. A more serious complication described is damage to the frontal branch of the facial nerve, resulting in the inability to raise the eyebrow. It occurred in almost 3% of cases (see table).
The number and types of complications associated with the supraorbital trans-eyebrow approach, according to the literature
Wound revisions were performed in 52 (2.5%) cases. The exact relationship between revisions and selected access cannot be assessed due to insufficient information regarding the issue of revisions.
The cosmetic outcome is difficult to evaluate impartially, given that patient perception is subjective, as is the aesthetic outcome assessed by an independent observer. However, in 89.3% of cases, the aesthetic result was regarded as excellent, and headache and pain in the area of the postoperative wound were absent or minimal [36], more than 90% of patients were satisfied [37], 92.8–96.9 % of patients considered the cosmetic result to be “quite pleasant” and “excellent” [36]. The aesthetic benefit of this approach is most obvious in patients with high hair growth, for whom a conventional skin incision would leave a noticeable scar on the scalp. The most common complaint was the presence of a “dent” at the burr hole [36].
Access restrictions
Cadaveric studies have greatly increased the understanding of the limitations of the supraorbital approach. They showed that anterior cranial landmarks that define safe zones for skin incision (eg, the position of the supraorbital foramen in relation to the laterally located frontal sinus) vary greatly [38, 39]. In addition, the large frontal sinus limits the size of the trepanation and forces the surgeon to perform the trepanation more laterally, changing the access trajectory [40]. Cadaveric studies have also shown that the supraorbital approach generally provides a good view of the structures of the anterior cranial fossa, while the view of the structures of the middle cranial fossa and cavernous sinus is partially obscured by the lesser wing of the sphenoid bone. The view of deep structures may also be limited by the superior edge of the orbit. Stitching the superior orbital wall provides additional maneuverability at angles of attack, but does not improve visibility of structures [41]. In addition, the view of the anterior parts of the anterior cranial fossa is limited by the roof of the orbit, which makes it impossible to remove mid-located formations of the anterior parts of the anterior cranial fossa. The results of work on cadaveric material showed that the supraorbital approach provides the same working area as the pterional and orbitozygomatic approaches, but with significantly smaller angles of attack compared to standard approaches [42].
In the initial stages of mastering access, it seems complicated to execute, and there appears to be a learning curve. Inadequately performed access for large tumors may be associated with partial removal of the tumor and subsequently with the need for repeated operations through another approach. Practicing the approach on cadavers is often necessary to familiarize the surgeon with anatomical landmarks and viewing angles, which are very different from traditional craniotomies. In addition, anatomical features, such as a prominent superior orbital rim or a large frontal sinus, can significantly complicate access, particularly for complex or giant aneurysms [43].
One of the disadvantages of keyhole surgery is also the need to frequently move the microscope to adequately view the surgical field. Frequent movement of the microscope and changes in focus or scale when manipulating the deep structures of the skull base, especially in the absence of a retractor system, is energy-consuming for the surgeon and limits his work under high magnification. In this regard, all operations were performed using a Mari operating microscope control device [44].
Supraorbital trans-glabellar approach for removal of meningiomas
Meningiomas of the anterior cranial fossa account for approximately 12–22% of all intracranial meningiomas [45–47]. After the pioneering publications of Durante (1884), Cushing and Eisenhardt (1938), various series of scientific papers on the removal of olfactory and suprasellar meningiomas were published. According to the literature [46–64], over the past two decades, olfactory and suprasellar meningiomas have been operated on using various approaches, including bifrontal, unilateral subfrontal, pterional and frontopterional. The maximum radical removal of olfactory meningiomas (85–100%) was achieved using pterional and bifrontal approaches and was accompanied by a low incidence of complications [48–50]. The likelihood of tumor recurrence ranged from 5 to 41% over 10 years and was associated primarily with incomplete resection. Residual tumor fragments in most cases were located at the base of the anterior cranial fossa and the ethmoid labyrinth or sphenoid sinus [49, 50, 57, 61, 65, 66].
Total removal of suprasellar meningiomas is often more difficult, as they can extend along the optic nerves, hypothalamic-pituitary region, anterior circle of Willis and cavernous sinus [51-54]. According to recent publications [46, 47, 51-54, 58-60, 62, 63], the radicality of removal of suprasellar meningiomas ranged from 67 to 100%, visual deficit occurred with a frequency reaching 20%, mortality ranged from 0 to 8. 7%.
A comparative analysis of supraorbital and traditional transcranial approaches for tumors of the anterior cranial fossa and parasellar region is given in a number of sources. The radicality of tumor removal using these approaches was approximately the same and reached 86–100% for olfactory meningiomas and 40–100% for meningiomas of the suprasellar region [4, 11, 17, 19]. Subtotal removal was mainly associated not with inadequate access, but with invasive tumor growth [4, 11, 17, 19]. The decision to choose this approach for removing meningiomas of the suprasellar localization and anterior cranial fossa is recommended to be made taking into account the topographic and anatomical features of the tumor, the experience of the surgeon and the availability of the necessary neurosurgical instruments. Optimal for surgery through the supraorbital approach is the absence of spread of meningioma into the anterior parts of the anterior cranial fossa, especially on the side opposite to the access, and dimensions not exceeding 60 mm [3, 4, 8, 18, 50]. Larger tumors can also be removed through the supraorbital approach, provided that the main volume is located within the surgical corridor (see Fig. 7) [4].
A contraindication for the supraorbital approach is considered to be invasive tumor growth in the ethmoidal labyrinth and sphenoid sinus, since a small craniotomy limits the surgeon’s work when it is necessary to perform plastic surgery of the base of the anterior cranial fossa and remove the tumor from these areas. Tumors with bilateral spread to the anterior parts of the anterior cranial fossa and paranasal sinuses are more suitable for removal through bifrontal, pterional and other traditional approaches to the base of the anterior cranial fossa [48, 50, 56].
Disease detection
To choose the optimal treatment strategy and assess the prognosis, the doctor needs to get the most complete picture of the disease. For this purpose, all patients with suspected meningioma undergo a thorough diagnosis using the most modern equipment.
Before instrumental tests are started, the patient is examined by a neurologist. During the examination, the doctor assesses:
- state of the vestibular apparatus;
- reflexes;
- vision and hearing;
- coordination of movements and other cerebellar functions.
In addition, the doctor will carefully study the medical history and medical documentation provided by the patient, familiarize himself with the data of previously performed medical examinations and test results.
As part of the diagnosis, blood tests are required - general clinical, as well as a special analysis for tumor markers. Most patients are prescribed electroencephalography, a study of the electrical activity of the brain. This is an absolutely safe and painless procedure lasting about half an hour.
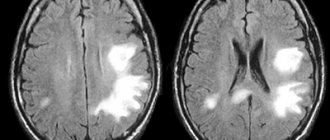
Medical imaging techniques are recognized as the “gold standard” in the diagnosis of meningiomas: computed tomography and magnetic resonance imaging. Both diagnostic procedures are usually performed with contrast enhancement to assess the size and location of the tumor, its location in relation to critical brain structures, and resectability (the possibility of removal during surgery).
| CT scan | creates a layer-by-layer image of brain structures, allowing you to identify deviations from the norm; |
| magnetic resonance imaging | a modern technique used as an alternative to CT to obtain a detailed picture of the affected organ; |
| angiography | The procedure involves the introduction of a special contrast agent into the blood to monitor the blood supply system of the tumor. This method is mainly used before surgery for the most accurate planning of surgeons’ actions; |
| biopsy | study of the morphological characteristics of a tumor based on a sample of tumor tissue. Biopsy and histological analysis help differentiate benign from malignant meningiomas. At the Assuta clinic, when performing a biopsy, the most modern equipment is used, which allows it to avoid affecting vital areas of the brain. |
1.Types of meningiomas
Meningiomas
represent the most common type of intracerebral neoplasms, most of them benign, or rather, in approximately 85 percent of cases.
Only a small part of the total number of meningiomas is malignant: these are anaplastic meningiomas, which are subject to one hundred percent recurrence. Tumors are formed by tissue cells of the soft meninges and can be located: on the surface of the brain (convexital); in the sagittal region, the region of the superior sagittal sinus and the falciform process (parasagittal); at the base of the skull (basal).
The most common type of tumor is convexital meningiomas – they are registered in half of the cases. Parasagittal meningiomas
are much less common: according to some medical sources, their frequency is 10-11%, according to others - up to 30% of the total number of meningiomas.
A must read! Help with treatment and hospitalization!
Effective assistance from Israeli doctors
The effectiveness of treatment of meningioma in the best medical facilities reaches almost 100% due to the work of first-class world-famous neurosurgeons. Thanks to their skill, as well as the most modern and effective treatment methods, Assuta patients quickly return to everyday life, forever forgetting about their terrible diagnosis - meningioma.
The therapeutic course includes several stages:
- consultation with a specialist, examination, medical history;
- detailed diagnostics (laboratory tests, computer and magnetic resonance imaging, electroencephalography);
- drawing up an individual treatment plan.
When planning treatment, the doctor takes into account the characteristics of the tumor (size, location, histological type, proximity to large vessels or vital centers), as well as the general condition of the patient (age, presence of concomitant diseases, severity of symptoms).
Treatment of meningioma without surgery - Cyber and Gamma knife at the Assuta clinic
Surgery is the highest priority method of combating the tumor, since this is the only way to remove it entirely, preventing the development of relapse.
The operation is indicated if the meningioma has already reached an impressive size, but its removal does not pose a danger to the life and health of the patient. For example, it is not always possible to perform resection of meningiomas adjacent to large blood vessels, venous sinuses, brain stem, etc. Assuta specialists recommend treating meningiomas that are difficult to reach or adjacent to critical structures using conservative methods that reduce the risk of complications to almost zero and do not injure healthy tissue.
Using a radio wave cyber knife instead of a traditional scalpel makes the procedure for destroying a tumor absolutely painless. In addition, there is no need for general anesthesia. The proven effectiveness of the cyber knife is 95%, and the course of treatment takes from one day to several months, depending on the size of the tumor and the individual characteristics of the body.
A gamma knife can be used to remove very small tumors. Gamma therapy is a modern non-invasive, gentle method of meningioma removal, practiced in medicine in Israel. It involves targeted irradiation of the lesion from different sides with small doses of radiation, which are focused directly in the area of tumor growth. The accuracy of the gamma knife is amazing - 0.3mm (for the cyber knife - 1.0mm).
After removing the meningioma using any of the above methods, the patient is observed for some time at the Assuta clinic and undergoes repeated checks. If there are residual tumor cells, a stereotactic course of radiation is prescribed, during which they are completely destroyed.
Israeli doctors do not recommend using chemotherapy and external beam radiation therapy to treat meningiomas due to the low effectiveness of these techniques. Chemotherapy is rarely used for inoperable meningiomas that are resistant to radiotherapy.
Treatment of meningioma in the most popular Assuta clinic in Israel is carried out under the close supervision of experienced neurosurgeons - Zvi Ram, Zvi Cohen, Moshe Adani, Dvora Blumenthal.
Types of meningioma
Types of tumors are classified according to several factors:
1. According to histological type, the following types of pathology are distinguished:
- typical: this form of the disease does not pose a threat to life, grows very slowly; removal of brain meningioma is prescribed and, as a rule, relapses are rare;
- atypical: the tumor grows faster and recurs more often;
- hodoid;
- clear cell;
- malignant: anaplastic, rhabdoid, papillary.
Low-quality types of tumor have an unfavorable prognosis: the tumor grows quickly and is difficult to treat. Anaplastic meningosarcomas are capable of penetrating into the brain and often metastasize to other organs.
2. By localization:
- frontal, parietal, temporal and occipital;
- presagittal;
- anterior cranial fossa;
- middle cranial fossa;
- posterior cranial fossa;
- tentorium cerebellum;
- foramen magnum;
- intraventricular and other rare locations.
In 95%, benign formations are diagnosed. Treatment of brain meningioma is planned depending on the type of tumor.
Prices for treatment of brain meningioma at the Assuta clinic
Basic screening program for brain tumors in Israel:
| Description of the procedure | Cost ($) |
| advanced blood tests | 440 |
| field of view | 350 |
| consultation with a neurosurgeon | 550 |
| preoperative preparation (ECG + x-ray of the lungs + consultation with an anesthesiologist) | – |
| navigation MRI | 1350 |
Therapy includes:
| Description of the procedure | Cost ($) |
| surgery and 4 days of hospitalization in the neurosurgery department (1 day in intensive care) | 23900 |
| use of neuro-physiological monitoring | 1450 |
| surgical materials and equipment | 2250 |
| rapid biopsy during surgery and final histopathology of the tumor | 1250 |
After completion of the operation and during the further rehabilitation period, the patient is advised not to leave Israel for fourteen days. During this period, Israeli doctors will develop an individual program of further medical observation and treatment for you.