Hemiplegic (Hemiparetic) form of cerebral palsy
Right-sided hemiparesis This form is most common. It is expressed in paresis, or paralysis, which covers one half of the body. The arm usually suffers more than the leg. Most patients have mental disorders, reduced intelligence (moronicity, idiocy), but such children are capable of learning and usually adapt to life in society and to work. Children with hemiparesis master age-related skills later than healthy ones. Therefore, the level of social adaptation, as a rule, is determined not by the degree of motor defect, but by the intellectual capabilities of the child. Clinically characterized by the development of spastic hemiparesis (Wernicke-Mann type gait, but without leg circumduction), delayed mental and speech development. Sometimes it manifests itself as monoparesis. With this form, focal epileptic seizures often occur.
Spastic diplegia (Little's syndrome). Tetraparesis with spasticity in the legs.
The most common type of cerebral palsy (3/4 of all spastic forms) is expressed in spastic paresis of mainly the lower extremities. Favorable prognosis for the possibility of social adaptation. The degree of social adaptation with normal mental development can reach the level of a healthy person. Spastic diplegia is characterized by the early formation of contractures, deformities of the spine and joints. Mostly diagnosed in children born prematurely. Pathology of the cranial nerves is common: convergent strabismus, optic nerve atrophy, hearing impairment, delayed mental and speech development, dysarthria, etc., including those caused by environmental influences on the child (insults, segregation). The patient’s psyche suffers, but not as much as in other forms of cerebral palsy. The prognosis for motor abilities is less favorable than for hemiparesis.
Cerebral palsy (CP) | Children's Orthopedics
The term “cerebral palsy” came into use in the 60s of the 19th century, thanks to the works of the English surgeon Little. He described a special type of cerebral palsy, namely spastic diplegia, which is still called Little's disease.
Cerebral palsy (CP) is a non-progressive brain injury caused by exposure to a number of unfavorable factors in the prenatal, perinatal and early postnatal periods, and is always accompanied by motor and often orthopedic disorders .
The term “cerebral palsy” unites a group of syndromes with different clinical manifestations that arise as a result of underdevelopment of the brain and its damage at various stages of ontogenesis and are characterized by the inability to maintain a normal posture and perform voluntary movements.
The definition of cerebral palsy excludes progressive hereditary diseases of the nervous system, including various metabolic defects, lesions of the spinal cord and peripheral nerves.
At present, it is clear that the term “cerebral palsy” does not reflect the diversity and essence of neurological disorders associated with this disease, however, it is widely used in the world literature, since no other term that comprehensively characterizes these pathological conditions has been proposed to date. Their combination into a nosological group makes it possible to plan organizational measures aimed at early diagnosis and treatment of cerebral palsy, since this problem has not only medical, but also social significance.
Changes in the symptoms of cerebral palsy are associated with the dynamics of morphofunctional relationships in the pathologically developing brain and the increase in orthopedic problems.
The incidence of cerebral palsy is 2-3 cases per 1000 newborns; it affects 1% of premature babies.
ETIOLOGY and PATHOGENESIS
There are many different opinions about the etiology of cerebral palsy, and the disease is considered to be polyetiological. An analysis of the causes leading to the occurrence of cerebral palsy showed that in most cases it is not possible to single out one of them, since there is often a combination of several unfavorable factors both during pregnancy and childbirth.
The etiological factors of the disease are:
- deep prematurity and hydrocephalus;
- malformations of the brain;
- hemorrhages (intraventricular and subepidermal, in the cerebellum);
- hypoxic-ischemic damage to gray matter;
- periventricular leukomalacia;
- hypoglycemic and thromboembolic damage (including secondary vasculitis due to infections);
- bilirubin encephalopathy;
- hypoxia due to respiratory disorders (bronchopulmonary dysplasia);
- electrolyte disturbances;
- traumatic injury to the brain and spinal cord (birth injuries: premature, rapid, protracted labor, tight entanglement of the umbilical cord, asphyxia during childbirth, damage to the cervical spine during childbirth, application of obstetric forceps, etc.);
- intrauterine infection of the fetus (toxoplasmosis, chlamydia, uroplasmosis, herpes virus, rubella, etc.);
- incompatibility of the Rh factor of mother and fetus with development (“Rh conflict”);
- mother's work with toxic agents during pregnancy (paint and varnish production, chlorine-containing substances, etc.);
- toxicosis of pregnancy, infectious, endocrine, chronic somatic diseases (internal organs) of the mother;
- High risk factors for the development of cerebral palsy include various complications during childbirth: weakness of the contractile activity of the uterus during childbirth, rapid labor, cesarean section, prolonged labor, a long anhydrous period, breech presentation of the fetus, a long period of standing of the head in the birth canal, instrumental obstetrics. Most domestic and foreign authors include premature birth , as well as congenital malformations and a child’s birth weight less than 2000 grams, as one of the most predisposing factors to the development of cerebral palsy.
Currently, the causal relationship of cerebral palsy with perinatal problems, especially asphyxia, is considered valid only in cases of a combination of the following factors:
- the presence of severe and prolonged asphyxia during childbirth;
- the presence of clear signs of hypoxic-ischemic encephalopathy in the newborn;
- the possibility of explaining neurological deficits by intrapartum asphyxia;
- exclusion of other diseases that may cause cerebral palsy.
An important pathogenetic mechanism that determines intrauterine brain damage is probably an autoimmune process. As a result of exposure to a number of etiological factors of the prenatal period, causing intrauterine damage to the fetus, destruction of the cellular structures of the brain occurs. Fragments of destruction can enter the circulatory system as substances foreign to the body - brain antigens. They lead to the formation of antibodies. In this way, an autoimmune process develops with subsequent alteration of brain tissue, which can last for several months and even years.
With concomitant cervical injury, as well as with a forced position of the neck (flexion or extension):
- spondylogenic myelopathy develops;
- delayed dystonia develops;
- musculoskeletal problems appear or intensify (in the spine, joints).
CLINICAL PICTURE
Let's consider the existing classifications of clinical variants and forms of cerebral palsy. Based on the type of movement disorders, there are four types of cerebral palsy :
- spastic variant , which is divided into:
- diplegic variant (legs are more affected than arms);
- quadriplegic variant (all four limbs are equally affected);
- hemiplegic variant (unilateral involvement of the limbs with greater involvement of the arms than the legs);
- dyskinetic variant , which is divided into:
- hyperkinetic variant (choreoathetosis);
- dystonic variant;
- atactic variant;
- mixed version.
The most common forms of cerebral palsy are mixed.
Forms of cerebral palsy (Semenova K.A.; 1972):
- spastic diplegia;
- double hemiplegia;
- hyperkinetic form;
- atonic-astatic form;
- hemiplegic (hemiparetic) form.
Clinical syndromes of cerebral palsy (Miller G.; 1992) : •diplegia (hand function is good, legs are more affected, asymmetrical manifestations);
- hemiplegia (the arm is affected more than the leg, the leg is affected more than the arm or to the same extent);
- quadriplegia (tetraparesis);
- dyskinetic (with a predominance of dystonia and athetosis);
- ataxic syndrome (pure ataxia, ataxic diplegia);
- atonic syndrome.
Spastic diplegia (Little's syndrome) is the most common form of cerebral palsy and develops with hypoxic-ischemic brain damage, most often in premature newborns. It is characterized by spastic tetraparesis, the legs are worse than the arms.
Spastic hemiplegia is the second most common form of cerebral palsy: most often the arm is affected more than the leg, and develops when the opposite hemisphere is affected.
Double hemiplegia is the most severe and difficult to treat form of cerebral palsy: spastic tetraparesis (arms worse than legs) is formed with severe damage to both hemispheres.
The dystonic form of cerebral palsy develops when the deep subcortical nuclei are damaged as a result of hemolytic jaundice or asphyxia during childbirth. It can be with a predominance of athetosis (movements are impaired by the type of chorea, athetosis, or a combination of both types, muscle tone is reduced, clinical manifestations from an early age) or dystonia. In the latter case, an increase in muscle tone predominates in all extremities (spasticity and rigidity), back muscles, and pharyngeal muscles. Delayed dystonia is characterized by the onset of symptoms 3-12 months after injury. In dystonic forms of cerebral palsy, involuntary movements occur and control of movements is difficult.
The atactic form is characterized by clinical and etiological heterogeneity, develops with early prenatal damage, and is manifested by impaired coordination and balance. Genetic counseling is necessary to rule out degenerative diseases. With cerebellar hypoplasia and Joubert syndrome, autosomal recessive inheritance often occurs.
The atonic form is also characterized by clinical and etiological heterogeneity and often develops in newborns with early prenatal damage.
Various forms of cerebral palsy are characterized by a variety of disorders, including:
- motor disorders (paresis of varying severity, hyperkinesis);
- disturbances of vestibular function, balance, coordination of movements, kinesthesia (disorder of the sensation of movement, weakening of proprioception from muscles, tendons, joints);
- dysfunctions of the brain (dyspraxia, agnosia, denial of motor defects, sensitivity disorders, speech disorders in the form of aphasia, dysarthria);
- abnormalities of perception - ignoring the affected limbs in 50% of children with hemiplegia;
- cognitive impairment in 65% of children, mental retardation in more than 50%;
- behavioral disorders (impaired motivation, attention deficit, phobias, generalized anxiety, depression, hyperactivity);
- delay in the rate of motor and/or psycho-speech development;
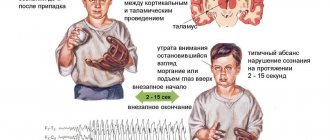
- symptomatic epilepsy (in 50-70% of cases);
- visual impairment (strabismus, nystagmus, amblyopia, cortical loss of visual fields);
- hearing impairment;
- hypertensive-hydrocephalic syndrome;
- diffuse osteoporosis;
- disorders of the cardiovascular and respiratory systems;
- urological disorders (hyperreflexia of the bladder, detrusor-sphincter dyssynergia), developing in 90% of patients;
- orthopedic problems are manifested by shortened limbs and scoliosis in 50% of children suffering from cerebral palsy. Lack of visual, auditory and vestibular afferentation leads to impaired motor control.
Assessment of the patient’s condition must necessarily include the total severity of functional disorders:
- mildly expressed functional disorders: there is the ability to walk independently, fine motor skills are intact, a vocabulary of more than 2 words, IQ exceeds 70 points (patients are able to lead an independent life);
- moderately severe functional disorders : the ability to crawl or walk with support, limited fine motor skills, the ability to pronounce individual words, IQ is 50-70 points (patients need help);
- pronounced functional disorders: lack of ability to move, complete lack of fine motor skills, unintelligible speech, IQ less than 50 points (patients need full care).
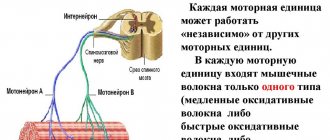
In spastic forms of cerebral palsy, several types (syndromes) of movement disorders are distinguished, leading to the formation of deformities in the joints and spine, which is important to consider when carrying out rehabilitation and corrective treatments:
- Triceps syndrome or dynamic equinus . With the development of equinus, walking on toes is formed, the knee joint is in a state of flexion. Triceps syndrome is formed with the participation of the cervical symmetrical tonic reflex. Most often it occurs with increased tone in m. triceps surae. Increased tone in the gastrocnemius and soleus muscles, possible involvement of the plantar muscles. Plantar flexion of the foot occurs with the participation of m. Triceps surae, m. tibialis posterior, m. plantaris, m. flexor hallucis longus, m. flexor digitorum longus, m. peroneus longus and m. peroneus brevis.
- Adductor spasm or adductor syndrome . This clinical syndrome, the second most common in cerebral palsy, is caused by spastic contracture of the adductor muscles of the thigh (m. adductor magnus, m. adductor longus, m. adductor brevis, m. gracilis - during internal rotation of the thigh), it is also necessary to take into account the activity of the leg flexor muscles ( m. semimembranosus and m. semitendinosus), if the spasm is accompanied by flexion of the knee. Features of movement: the hips are tightly in contact, there is a cross at the level of the hips or knee joints, pronounced frontal instability, it is difficult to move the leg forward when walking, hyperlordosis in the lumbar region, there is always weakness of the outer thigh muscles, the gluteus medius and minimus muscles. As a rule, adductor syndrome is accompanied by hip dysplasia, sometimes with subluxation or dislocation of the femoral head, as well as a positive Trendelenburg sign. The most common is paresis of the gluteal muscles (antagonists of the adductor group).
- Hamstring syndrome . This is the third most common syndrome in cerebral palsy, accompanied by an increase in the tone of the posteromedial group of thigh muscles (m. semimembranosus, m. semitendinosus, long head of m. biceps femoris), which extend the hip joint, flex the lower leg, and carry out internal rotation of the bent knee. Features of gait: the patient stands on legs bent at the knee joints, feet in the equinus position, support on the entire foot is possible, the pelvis is tilted forward or backward. Total kyphosis of the spine is possible.
- Rectus syndrome . This syndrome is a common motor disorder in cerebral palsy. With a straightened fixed knee, the voltage in m. Rectus femoris causes the pelvis to tilt forward and downward. Rectus syndrome is formed when the cervical symmetrical tonic reflex and labyrinthine tonic reflex increase. There are two variants of rectus syndrome. With an increase in the cervical symmetrical tonic reflex, walking on straight legs, hyperlordosis in the lumbar region, and a pronounced forward tilt of the pelvis are characteristic. With an increase in the cervical symmetrical tonic reflex and labyrinthine tonic reflex, walking on bent legs is characteristic, lordosis in the lumbar region is smoothed or normal, and the forward tilt of the pelvis is less pronounced. There is also rectus rotation syndrome, which also has two development options. With an increase in the cervical symmetrical tonic reflex, the patient stands and walks on straight, inwardly rotated legs, feet in equinovarus with pronounced internal rotation, hyperlordosis in the lumbar spine. With an increase in the cervical symmetrical tonic reflex and labyrinthine tonic reflex, he walks with legs bent and rotated inward, the feet in the equinus and equinovarus positions, the torso tilted forward, the lordosis is smoothed or normal.
- Spasticity of the hand.
DIAGNOSIS AND DIFFERENTIAL DIAGNOSIS
The presence of a motor defect and a delay in the development of motor functions in a non-progressive course of the disease, as well as neurological examination data indicating the cerebral genesis of the existing symptoms, are the basis for the diagnosis of cerebral palsy. In some cases, especially during the second year of life, children with cerebral palsy lose some motor functions, which is usually associated with the development of contractures, excessive weight gain or lack of motivation (especially in children who can barely walk). Some diseases (ataxia-telangiectasia, Lesch-Nychen syndrome) may initially manifest as non-progressive movement disorders. The progressive nature of these diseases becomes obvious only after 3-4 years. Particular attention should be paid to differential diagnosis with Segawa's disease (DOPA - sensitive dystonia). Children suffering from this disease develop normally until 6 months, and then dystonic disturbances that fluctuate throughout the day occur, which are usually completely relieved by small doses of levodopa. In hypotonic children (“flaccid child”), spinal amyotrophy or congenital myopathy can be assumed. In these cases, adequate diagnostic methods are electroneuromyographic study and muscle biopsy.
GENERAL PRINCIPLES OF REHABILITATION OF PATIENTS WITH Cerebral Palsy
Rehabilitation measures for cerebral palsy are aimed at correcting the motor defect, developing the patient’s daily independence in terms of self-care, improving motor activity and adaptation when moving, improving communication capabilities, social and emotional development, education and training, adaptation to impaired swallowing, chewing, and correction of motivational factors. violations.
A team of specialists working with children suffering from cerebral palsy should include a neurologist, rehabilitation specialist, kinesiotherapist, physiotherapist, orthopedic surgeon, psychotherapist, occupational therapist, ophthalmologist, otolaryngologist, psychologist, teacher, oligophrenopedagogue, speech therapist, geneticist and social worker.
In the early stages of the disease, neurometabolic and symptomatic therapy is used. In the late period, symptomatic therapy is used (for spasticity - muscle relaxants, phenol and ethanol blockades, administration of botulinum toxin type A, baclofen pump, surgical treatment); for hypotension, anticholinergics are prescribed. Anticonvulsant therapy is also used, sphincter disorders, cognitive and behavioral disorders are corrected.
Orthotics occupy an important place in rehabilitation. A large number of rehabilitation techniques are aimed at stimulating motor activity and enhancing sensory flow, correcting postural attitudes, motor motivational and cognitive disorders. The system of skills development according to Tardieu G. is used; Exercise therapy (taking into account craniocaudal patterns of motor development); Bobath techniques (positions that inhibit pathological reflexes; development of voluntary movements, balance functions; training in postures that promote verticalization), Vojta V., Kobat H., Bortfeld S.A., Tekoryus V.A.; method of dynamic proprioceptive correction (cosmonaut suits); MOVE – development of skills through training; gait training using phasic electrical stimulation. Correction of the emotional-volitional sphere, conductive pedagogy - motivation to action, hippotherapy, mechanotherapy (fixing, training, combined) are also used. All techniques are aimed at stimulating motor activity, sensorimotor connections, tactile sensitivity, training vestibular functions and balance, correcting functional and postural disorders, restoring passive and active range of motion, reciprocal relationships between antagonist muscles.
An important place in the treatment of cerebral palsy is currently occupied by the administration of botulinum toxin type A (Dysport, Botox). The effectiveness of Dysport treatment is 80-95%, the duration of the therapeutic effect is 2-6 months.
Under the influence of botulinum toxin type A, paresis with increased muscle activity turns into paresis with reduced muscle activity. For diffuse movement disorders, local use of botulinum toxin type A is possible. Botulinum toxin type A is used to correct spastic movement disorders: with dynamic (unfixed) contracture with preserved muscle function, if paresis is accompanied by increased muscle activity and the ability to use the function of agonist and antagonist muscles to learn new things is preserved locomotor act.
In patients with cerebral palsy, botulinum toxin type A is indicated for spastic forms of the disease (spastic diplegia, spastic hemiplegia), as well as for its dystonic or mixed forms (a combination of spasticity and dystonia). When spasticity and muscle hypotonia are combined, when using Dysport, diffuse muscle weakness may appear for up to two to three weeks, which is likely due to the effect of saturating the muscle with botulinum toxin type A (systemic side effect).
A relative indication for the use of botulinum toxin type A is diffuse muscle spasticity with psychomotor retardation (cerebral palsy, double hemiplegia): the drug can be used to improve the ability to care for adductor spasm in the legs, or flexor position in the arms, or adductor contracture in the shoulder joints. A relative indication for the use of botulinum toxin type A is the hyperkinetic form of cerebral palsy. In this case, the drug reduces the amplitude and frequency of hyperkinesis, but requires constant administration as the effect decreases.
Botulinum toxin type A is contraindicated in atonic-astatic forms of cerebral palsy.
Double hemiplegia Spastic tetraplegia
One of the most severe forms of cerebral palsy, which is a consequence of brain damage due to intrauterine chronic fetal hypoxia. The cerebral hemispheres or the entire brain are affected. Spastic quadriplegia (quadriparesis, since both the upper and lower limbs are equally severely affected) is diagnosed clinically. Characteristic deformation of the trunk and limbs. In almost half of the cases, movement disorders are accompanied by strabismus, atrophy of the optic nerves, and hearing impairment. pseudobulbar syndrome, epileptic seizures are observed. Such patients subsequently cannot learn to sit, stand and walk; hand defects and lack of motivation exclude self-care and work activity. On the mental side, severe debility, imbecility, and idiocy are noted.
Classification of forms of cerebral palsy K.A. Semenova
1.Spastic diplegia (Little's disease) The most common form (50%). There is a bilateral, sometimes asymmetrical lesion or underdevelopment of the central motor neuron. Motor disorders - tetraparesis (arms and legs are affected), the lower extremities are affected to a much greater extent. The main symptom is increased muscle tone in the extremities with limited strength and range of motion in combination with persistent tonic reflexes. The severity of speech, mental and movement disorders varies widely, this is due to the time and strength of exposure to harmful factors.
2. Double hemiplegia The most severe form of cerebral palsy. Total damage to the brain, primarily to the cerebral hemispheres. Movement disorders are expressed equally in the arms and legs, or the arms are more affected. Clinical manifestations are the predominance of muscle rigidity, which increases under the influence of intense tonic reflexes that persist for many years.
3. Hemiparetic form of cerebral palsy It is characterized by unilateral damage to the same-named (left or right) limbs (arms and legs). There is damage predominantly to one hemisphere, its cortical parts and the nearest subcortical nuclei. Violation of the cortical functions of one of the hemispheres manifests itself in the form of hemiparesis. These children are teachable.
4. Hyperkinetic form of cerebral palsy is observed in 20-25% of patients. This form is associated with lesions of the subcortical parts of the brain. Movement disorders manifest themselves in the form of involuntary violent movements - hyperkinesis. Hyperkinesis occurs involuntarily and intensifies with excitement, as well as with fatigue and attempts to perform any motor act. In 60-70% of cases, children learn to walk independently, but voluntary motor activity, especially fine motor skills, is significantly impaired.
5. Atonic-astatic form of cerebral palsy There is damage to the cerebellum and frontal parts of the brain. Motor pathology: low muscle tone, imbalance of the body at rest and when walking, impaired sense of balance and coordination of movements, tremor, hypermetry (disproportion, excessive movements).
Intelligence varies from ZPR to u.o. varying degrees of severity. When the frontal parts of the brain are damaged, children are less emotional, indifferent to others, have little initiative, can be very aggressive, in 55% of cases (debility or imbecility).