The spinal cord is a section of the central nervous system that transmits nerve impulses from the brain to other organs and systems, and in the reverse order. It is also responsible for the normal functioning of the skeletal muscles and takes part in the activities of the following systems:
- respiratory;
- cardiovascular;
- urogenital;
- digestive.
Tumors in the spinal cord or those located nearby can cause irreparable harm to the entire body. Despite the fact that neoplasms in the spinal cord are rarely diagnosed, it is important to have some useful information for timely detection of pathology. The disease may not make itself felt for years, and in the lost time the tumor can affect neighboring organs.
Classification of the disease
Formations in the spinal cord are classified according to various parameters that are important for the diagnosis and further treatment of the tumor. First of all, pathology is divided into the following types:
— Primary
. Neoplasm cells consist of nerve or brain cells.
— Secondary
. It is metastasis of a tumor located elsewhere.
Depending on the anatomical location of the tumor, they are divided into:
Intramedullary
. Intracerebral formations consist of spinal cells and occur in 18-20% of cases of pathologies in the spinal cord. The location of the tumors is inside the spinal cord, they affect its tissues. Intramedullary tumors, in turn, are divided into:
- ependymomas;
- astrocytomas;
- hemangioblastoma;
- oligodendrogliomas;
Extramedullary.
Neoplasms are located outside the brain and make up 80-82% of the total number of tumors. Localized near the spinal cord, their ingrowth is possible. Extramedullary formations are also classified into:
- subdural (intradural): affect the dura mater of the spinal cord and nerve roots;
- epi- or extradural (vertebral): located on both sides of the meninges, they are metastases, non-malignant and malignant tumors.
In relation to the spinal canal, neoplasms are:
- Intravertebral
. Localization - inside the spinal canal. - Extravertebral
. They are characterized by growth from outside the spinal canal. - Extraintravertebral
. Tumors of this type resemble an hourglass. One part is located inside the spinal canal, the other is located outside.
According to the type of spread, types of neoplasms are distinguished:
- craniospinal;
- cervical, thoracic or lumbosacral regions;
- coccygeal and lower sacral segments;
- horse tail.
Based on the type of histology, tumors are divided into the following:
- meningiomas;
- schwanommas;
- neuromas;
- angiomas;
- hemangiomas;
- hemangiopericytomas;
- ependyomas;
- sarcomas;
- oligodendrogliomas;
- medulloblastomas;
- astrocytomas;
- lipomas;
- cholesteatomas;
- demrmoids;
- epidermoids;
- teratomas;
- chondromas;
- chordomas;
- metastases.
Meningiomas are the most common. All types of spinal cord tumors (SCT) are pathological neoplasms - benign or malignant.
Extramedullary type
Such neoplasms, which in medicine are given the name “extramedullary,” are concentrated not inside the spinal component, but in close proximity to it. Simply put, they originate in the structures that surround the SC (developing from the meninges, nerve roots, fatty tissue and other tissues passing nearby).
This category of harmful process is the most common; it develops 4 times more often than true intracerebral pathogenesis, and, fortunately, is more represented by pathologies of benign origin. But this does not mean at all that a non-malignant disease cannot portend anything terrible. In the absence of the necessary treatment, it threatens severe disability due to compression of the spinal cord and its elements, up to the complete loss of the ability to move and self-care. Sudden death cannot be ruled out. This is not to mention the fact that due to such neoplasia, irreversible destruction of the bone and cartilaginous units of the spinal column often occurs. Therefore, both extra- and intramedullary tumors equally require timely diagnosis, as well as the rapid involvement of adequate methods of therapy.
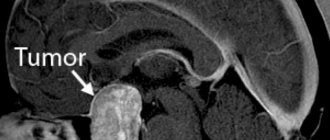
MRI.
Extramedullary OSM can have extradural (31.5%) or intradural (68.5%) localization. The extramedullary-extradural type is distinguished by its large size and the predominance of malignant forms; in turn, the malignant focus progresses at a fairly intensive pace and is predominantly recognized as a secondary (metastatic) formation. The extramedullary-intradural type of pathology, which is also the most common, is characterized by a predominance of primary neuromas (40%) and meningiomas (25%).
- Meningioma (arachnoidendothelioma) is a benign tumor that grows slowly and gradually. Formed from cells of the arachnoid meninges. Diagnosed over the age of 50 years, and in predominant numbers in women (80%). With a high frequency it affects the spinal membrane in the thoracic region. Rarely, but can recur and produce multiple growths, causing transverse damage to the spinal column. Although the size of this neoplasia, which externally resembles a small dense node, rarely increases by more than 1.5 cm, such a tumor even a few millimeters in size can directly put pressure on the nerve structures, provoking a severe neurological clinical picture of symptoms.
- Neuroma (schwannoma) is a round-shaped benign OSM with clear boundaries and a dense structure, which develops as a result of metaplasia of lemmocytes (Schwann cells), namely auxiliary cells of the peripheral nerve fiber involved in the formation of the myelin sheath. Female patients are more likely to experience this disease; people of middle age and older have the greatest predisposition. At first, the disease proceeds latently, and later it is expressed by severe radicular pain, paresis and paralysis of the muscles in the area of innervation, loss of sensitivity according to the conduction type. The neck and thoracic region are common areas that neuromas affect.
Other extramedullary neoplasms with intradural concentration (angiomas, lipomas, metastases, etc.) are much less common.
Causes of spinal cord tumors
The appearance of neoplasms of this type may be preceded by the following risk factors:
- the effects of radiation on the body;
- ultraviolet irradiation;
- poor environmental situation;
- frequent use of a mobile phone;
- being near high-voltage lines;
- exposure to microwave and electromagnetic radiation from household appliances;
- exposure to chemicals or nuclear waste;
- smoking;
- genetic abnormalities;
- consumption of products with nitrates and carcinogens;
- family history of skin, bladder, breast and pancreatic cancer.
The likelihood of developing the disease also increases with age. In addition, doctors identify specific causes of ACM:
- hereditary neurofibromatosis;
- Hippel-Lindau disease.
The appearance of spinal cord tumors, like other types of cancer, is also due to constant stress and lack of emotional balance.
Causes of lumbar spine cancer
To this day, the origin of cancer is not fully understood. However, the following factors have been identified that create a favorable environment for the development of the disease:
- genetics;
- bad habits (smoking, unhealthy diet, etc.);
- negative impact of the external environment (living in places with a high dose of radiation, near testing sites, etc.);
- work in hazardous industries;
- various spinal injuries;
- as a result of the development of AIDS.
Spinal cord tumor symptoms
The complex of symptoms depends on the etiology and severity of the pathogenesis of the disease. At the initial stage of the disease, symptoms are mild. Mostly the patient is unaware of the presence of a dangerous process in the body. Treatment of a spinal cord tumor is most effective if you seek medical help in a timely manner. Therefore, if the following signs appear, it is better to see a specialist:
- pain in the back or neck, usually spreading to other parts of the body;
- loss of sensation in the limbs;
- dysfunction of the musculoskeletal system;
- impaired coordination of movements;
- numbness, both at the site of the tumor and in the extremities, in the head, chest and abdomen;
- paresis;
- disruption of the genitourinary system;
- intestinal dysfunction;
- decreased potency;
- infertility;
- increased intracranial or blood pressure;
- headache;
- increased body temperature;
- loss of body weight.
Even with minor discomfort in the back area, you should consult a doctor. The clinical picture of ASM often resembles osteochondrosis or intervertebral hernia.
In addition, spinal tumors include the following syndromes:
1. Root. Intense pain is observed, which intensifies with coughing and sneezing, bending the head and physical activity.
2. Brown-Sequard. The clinical picture is expressed by sensory disorders, including a decrease in muscle-joint sensitivity and a decrease in temperature and pain perception.
3. Complete transverse lesion. In this case, there are disorders of the pelvic functions and the development of bedsores and paresis.
The size, type and stage of development of cancer pathology play a significant role in the manifestation of certain symptoms. One of the most important signs that should not be ignored is constant back pain, independent of physical activity. Taking painkillers for ASM does not have a long-term effect.
Answers to frequently asked questions
An unfavorable focus can develop both in the lumbar region and sacrum, and in the cervical and thoracic areas of the spine. To this day, doctors cannot yet reliably say what specific causes lead to tumors affecting the lumbar and other segments of the spine. Read on about this and more.
Reasons for development
Despite the etiology that is not completely clear to science, experts suggest that vertebral tumors can form due to:
- genetic predisposition;
- unbalanced diet;
- smoking and alcohol abuse;
- influence of toxic substances on the body;
- exposure to radioactive radiation;
- immunodeficiency and autoimmune pathologies;
- prolonged exposure to the sun, frequent visits to the solarium;
- chronic diseases of the spine and its traumatic injuries;
- prolonged and frequent stress.
ICD codes with interpretation
According to ICD 10, the classification of neoplasms of the vertebral system provides the following codes:
- C41.2 – malignant neoplasm (MN) of the spinal column (except for the sacrum and coccyx, code C41.4),
- D16.6 – benign neoplasm (BN) of the spine;
- D18.0, D18.1 – hemangioma, lymphangioma of any location;
- D32.1 – DN of the spinal cord membranes;
- D33.4 – DN of the substance of the spinal cord;
- D42.1 – tumor of the spinal cord of unknown nature;
- C72.0 – ON of the spinal cord.
The International Classification of Diseases, 10th revision, where pathologies are assigned code values, allows specialists around the world to adhere to uniform treatment, diagnostic and rehabilitation standards, maintain statistical records of morbidity and mortality, and use codes in medical documents (in certificates, disability certificates, etc.).
Diagnostic methods
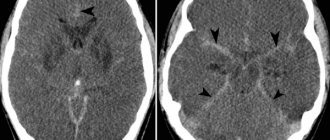
For diagnostic purposes, traditional visualization tools are used for these purposes. Many people are interested in whether a tumor in the spine is visible on an X-ray? Some tumor processes can be seen on X-rays, but to establish the type and stage of the tumor, more informative imaging techniques are used, in particular tomography methods (CT and MRI). Therefore, answering the question whether radiography shows all neoplasms, we answer that no, especially spinal ones. For complete information content, the following fundamental methods are used:
- computed tomography;
- magnetic resonance imaging;
- scintigraphy.
MRI diagnosis of spinal column tumor.
A biopsy, blood and urine tests are always prescribed. Comprehensive diagnostics makes it possible to fully understand the exact etiology, localization, type, stage, nature, extent of pathology, its spread to distant places and the presence of metastases.
Metastatic tumors
What tumors metastasize? Let us answer right away that benign diseases do not give metastases. According to clinical observations, of all malignant diseases in the spine, approximately 96% are secondary tumors, the remaining 4% are primary. This suggests that the dominant number of cases are associated with metastases, that is, cancer cells that have migrated to the spine from the primary lesion, which originally originated in another organ.
The main sources that metastasize to various parts of the spinal column are breast, prostate, thyroid, bladder, kidney and lung cancer. In addition to biopsy procedures and tomographic examination, blood biochemistry for tumor markers will help to identify the presence of cancer, which can be used to determine the location of the primary lesion, its growth, and metastases. To make it clearer, let’s give an example of what blood shows in this case:
- PSA enzyme > 30 units/ml – prostate cancer;
- CA 15-3 > 30 units/ml – breast cancer;
- the hormone calcitonin in men > 8.5 ng/l, in women > 5.1 – damage to the thyroid gland;
- Tu M2-RK from 16 units/ml or more, SCC >2.5 ng/ml – kidney cancer is affected;
- poor CEA values in combination with elevated CA 72-4 and CYFRA 21-1 – damage to lung tissue by cancer cells.
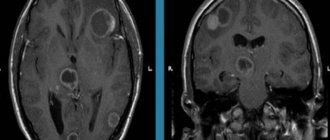
Metastatic tumor.
Thus, as you understand, a tumor may not necessarily initially originate in the spine. It can occur against the background of complications in the form of metastases, which have moved through the bloodstream or lymphatic vessels to the spinal region from completely different organs and systems in the body. At the same time, “maternal” tumors come in different types. Therefore, it is very important to use a differential approach to establish a true diagnosis.
As for primary neoplasms of a malignant nature, they arise in the ridge in isolated cases. In turn, they can also metastasize, but to other bones, liver, lungs, brain, lymph nodes, etc.
Metastases most often affect the lower thoracic and upper lumbar spine. Active malignant cells settled in them put pressure on the spinal cord, nerve endings, intervertebral discs, seriously reduce the density of the bone structure of the vertebral bodies, which is why neurological signs are clearly expressed and the likelihood of sudden compression fractures, spinal cord damage, increases significantly. death of nervous tissue.
Diagnosis of spinal cord tumors
The presence of a modern diagnostic complex in the neurosurgical department of the city clinical hospital named after A.K. Yeramishantsev allows for high-quality tests. Diagnostics helps to identify oncogenes in the patient’s blood with a hereditary predisposition. Progressive technologies and techniques provide the opportunity to:
- prescribe preventive anti-cancer measures;
- detect the first signs of illness;
- promptly begin effective treatment of the tumor.
In our clinic, after examination by a neurologist, the following methods of further monitoring are used to determine the location and spread of tumor formation and its histological type, and to identify disturbances in the patency of the cerebrospinal fluid:
- Magnetic resonance imaging;
- Ultrasound;
- CT scan;
- radionuclide diagnostics;
- spinal puncture and further analysis of the cerebrospinal fluid.
MRI of the spine today is considered the safest and most informative research method. To make the most accurate diagnosis, it is necessary to study samples of tumor tissue.
Tumor near the spine: what is it?
Don’t look for photos on the Internet if you find some raised formation or compaction on your spine! You still cannot make a diagnosis on your own. All this is understandable, you are worried about your health and urgently want to find out what kind of pathology has appeared on your back, is it cancer? However, even an experienced doctor will not always be able to make a diagnosis right away, simply by examining or palpating the painful area. Visually recognizable tumors visible on the back are not always a terrible oncology, but even without a qualified examination there is no guarantee that it is not.
There are a great many variants of diseases that can be concentrated in one place or another along the spine. This may be a complicated degenerative-dystrophic pathogenesis, a non-malignant or cancerous tumor of the spinal system. Or some disease of completely different tissues, for example, subcutaneous fat (lipoma, atheroma, etc.).
For your own good, in order to find out the type, malignancy of the pathogenesis, and receive an effective treatment program from a specialist, you should immediately visit a medical facility and undergo the necessary comprehensive diagnostics. Delay in the presence of cancer can cost a person his life.
Methods of treating the disease
The main treatment for a spinal cord tumor is surgical removal. Operations are prescribed after a complete examination of the patient and an accurate diagnosis. Today, the capabilities of neurosurgeons are significantly increased by the latest medical equipment:
— endoscopy technology provides the opportunity to gain access to tumors in hard-to-reach places;
— thanks to microsurgical instruments, the risk of complications during and after the procedure is reduced.
Our neurosurgery department has modern operating microscopes made in Germany with the highest degree of resolution. Their use allows surgeons to avoid damaging healthy areas.
The recovery period after removal of benign tumors ranges from several months to two years. In 70% of cases, complete recovery is achieved. In the case of intramedullary and low-quality formations, the prospect is not so comforting. Metastatic tumors are usually inoperable.
Further treatment for a spinal cord tumor after surgery includes:
- chemotherapy;
- radiation therapy.
To rehabilitate the patient, physiotherapeutic methods, fixation of the spine from the outside, and learning to walk again are prescribed. It is advisable to carry out social and psychological rehabilitation.
You can make an appointment using the contact number. We will provide a free consultation about the treatment of a spinal cord tumor, approximate prices and answer other questions.
The cost of surgical removal depends on the type of tumor and the nature of the surgical procedure. We guarantee operations at the highest level and at reasonable prices.
Types of benign tumors and their treatment
Known benign formations include:
- hemangioma;
- osteochondroma;
- osteoid osteoma;
- osteoblastoma;
- eosinophilic granuloma;
- aneurysmal bone cysts.
Vertebral hemangioma is one of the harmless vascular tumors of the spine that develops from endothelial cells. The prevalence ranges from 10% to 12.5%. It is formed mainly inside the spongy structure of the vertebra. As a rule, the thoracic (in 1st place) or lumbar regions are affected. Pathology of the cervical spine is the least frequently detected. In most cases, it does not behave aggressively, so treatment mainly consists of physical procedures and diagnostic monitoring. A large vascular conglomerate is subject to minimally invasive surgery using medical cement.
- Osteochondroma is the most common pathology (up to 36%) and is a nodular outgrowth of bone tissue interspersed with calcified cartilage, which is covered on top with a smooth cartilaginous “cap.”
It is located on the surface of the bone, most often on the spinous processes. It mainly appears in children around the age of 10; the period of development of the pathological formation lasts 15-16 years. It is treated by marginal resection of the defective bone along with the exostosis pedicle. The prognosis for recovery is favorable. Osteochondroma of the spine on x-ray. - Osteoid osteoma is a small round bone tumor formed from osteoclasts.
Among all, DN occupies 10%-12%. The articular processes of the vertebrae and their posterior structures, mostly the arches, are usually affected. It mostly affects young males and teenage boys. The most common location is the lumbar region (in 60% of cases). The only method of combating the disease is surgery, which involves excision of the defect with adjacent sclerotic areas of the bone. The outcome of treatment is generally favorable. Osteoid osteoma on MRI. - Osteoblastoma is similar to osteoid osteoma, but is much larger in size.
Its other name is giant cell tumor. This is a very rare form of the disease (among DN - 1%). It is more common in young people; the majority of patients are people under 30 years of age. Men suffer from this disease 2 times more often than women. Severely mutated tissue feels like a foreign body in the spine. Treatment measures are similar to the previous problem. Osteoblastoma on MRI - Eosinophilic granuloma is an infiltrate consisting of macrophages that most often affects the vertebrae. A very rare group of DN with a poor clinical picture. The first symptoms are rapid fatigue, decreased mobility at the site of the lesion, and mild periodic pain during physical activity. Sometimes it can be asymptomatic, but in the absence of appropriate treatment it leads to various deformities of the spinal column, increased painful manifestations, muscle hypertonicity, and stiffness of gait. Therapeutic measures include unloading the spine and the use of painkillers. In advanced cases, intratumoral curettage and surgical decompression of the spinal cord are performed.
- Aneurysmal bone cysts are bone cysts that are cavities in hard tissue filled with blood.
Often appears in the posterior segments of the vertebrae or directly in the vertebral body. The disease can develop after a spinal injury. The most common location is the cervical spine. Therapy consists of excision of the cystic element, curettage of the damaged area, and, if necessary, spinal decompression. Aneurysmal bone cysts
Surgery to remove spinal cord tumors
Neoplasms in the human spinal cord can be benign or malignant. Predominantly, surgery is prescribed for treatment. Surgical intervention is carried out after a complete examination of the patient, using magnetic resonance and computed tomography, as well as ultrasound. You will also need a spinal puncture to analyze the liquor fluid and conduct radionuclide diagnostics. Modern research methods make it possible to accurately determine the size, location and type of tumor in the spinal cord.
How is hemangioma treated?
A hemangioma of the vertebral body, if it is small in size and does not manifest itself aggressively, is not touched, but simply observed, periodically doing an MRI. This disease is benign, so there is no strong cause for concern; a tumor up to 1 cm is not dangerous. Usually it does not cause problems for a person, and if there are no signs of osteoporosis and neurological symptoms, treatment is limited to a maximum of exercise therapy and physiotherapy. But increased parameters of an abnormal vascular bundle inside the bone, which happens in isolated cases, require special surgical intervention. And primarily due to the fact that a vertebra affected by a defective conglomerate becomes fragile from the inside and can break at any time.
Hemangioma
In order to regress the tumor substance, as well as to reduce the neurological signs of the tumor and strengthen the weak vertebra, very productive neurosurgical technology is successfully used today. It's called vertebroplasty. This is a minimally invasive modern tactic that does not require general anesthesia and wide incisions. The essence of the technology is the introduction of bone cement based on polymethyl methacrylate through a percutaneous puncture into the pathological formation. The medicinal mixture is first mixed, after which a polymerization reaction occurs, releasing heat. Then the resulting mass is immediately fed through the working needle. The patient is allowed to go home within 24 hours after the intervention.
Indications for surgery
If the tumor develops rapidly and grows to a large size, surgical intervention is indicated. Metastatic formations, in most cases, are inoperable. In addition, the patient’s age, the presence of chronic diseases and the location of the tumor are taken into account. After preliminary studies, examination by a neurologist and neurosurgeon, surgical procedures are prescribed on an individual basis. The latest endoscopy instruments and microsurgical devices allow us to perform operations in our clinic, even in hard-to-reach areas and with a reduced risk of complications for the patient.
Rehabilitation after removal
After surgery, a patient is required to undergo a rehabilitation program to restore quality of life, prevent the development of complications and relapse of the disease. It is selected individually, based on the clinical case and the method of tumor removal. Therefore, the range of postoperative prescriptions for each individual patient will be different. It is worth noting that regardless of the type of surgical procedure involved, exercise therapy and physical therapy sessions are always recommended.
Recovery process.
It is extremely important for such complex patients to undergo both surgery and postoperative recovery in the conditions of the best medical center. Israeli, Czech and German clinics are highly professional in solving oncological spinal problems. I would especially like to highlight the Czech Republic, where the level of orthopedics, traumatology, oncology of the spinal system and rehabilitation management of cancer patients is similar to Israel and Germany, and the cost of equivalent high-tech care is two times lower.
But that’s not all, on the territory of the Czech Republic there are the best sanatoriums for spinal oncology, which, without exaggeration, have no equal in the whole world. Among the world-famous spa areas, where the most successful highly specialized sanatoriums operate, Karlovy Vary, Frantiskovy Lazne, Janske Lazne are especially popular. Today, the medical company Artusmed has earned high trust among domestic patients, which professionally and conscientiously helps organize treatment in the Czech Republic, a state where only modern and only promising methods of antitumor therapy of the spine have been mastered and practiced at an advanced level.
Rehabilitation and recovery prognosis
After removal of a malignant tumor, the patient must undergo a rehabilitation program, which is aimed at restoring the body, as well as preventing a possible relapse.
Such a program is selected individually in each individual case and includes physical therapy, physiotherapy, observation by a neurologist, etc. Regarding the prognosis of recovery, it is worth noting that the outcome of the disease depends almost 100% on the stage at which it was diagnosed. So, if the tumor was detected at the initial stage of development, then the chances of a successful cure are 90%. However, if the active manifestation of symptoms of lumbar spine cancer has already begun, then in this case doctors are powerless.