What is syringomyelia?
The spinal cord is an organ of the nervous system; it runs inside the spinal column from the cranial foramen, which communicates with the spinal column, to the first lumbar vertebra. Along its entire length - from the base of the skull to the coccyx, which ends the spinal column - sensory and motor nerves branch off from it. The structure of the spinal cord is the same as that of the brain - its central part, shaped like a butterfly, consists of gray matter with a predominance of nerve cells and a shell of white matter with a predominance of nerve fibers. The disease, in which a cyst-like cavity forms in the spinal cord, affects mainly the gray matter and is called syringomyelia , because the hole in the central spinal canal gives the spinal cord a flute-like appearance (in Greek, “syrinx”). In most cases, the origin of syringomyelia is unknown.
At our Institute, thanks to more than 40 years of research into the cause of Syringomyelia, a minimally invasive surgical technique has been developed for the treatment of idiopathic Syringomyelia: dissection of the filum terminale at the level of the sacrum with the unique Filum System® method (More information can be read below).
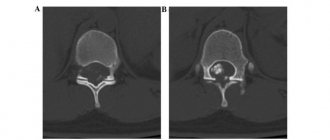
Fig. 1. – A 26-year-old man complains of loss of temperature sensitivity in the left half of the body and head, especially noticeable when taking a shower. The disease appeared a year ago. After surgical intervention - dissection of the terminal filum of the spinal cord - sensitivity was restored immediately after the operation. For 5 years after surgery, syringomyelia is practically asymptomatic.
What does a segment of the spinal cord consist of?
Anatomy of the spinal cord.
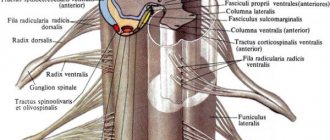
The SM segment is a section of the spinal cord that includes gray matter, a narrow border of white matter and one pair of spinal nerves.
Externally connected with the spinal nerves - this is the area that corresponds to a pair of spinal nerves. Therefore, the number of pairs of spinal nerves is equal to the number of segments - 31 pairs of spinal nerves and 31 segments.
Note! After the narrow border, the rest of the white matter is not included in the segment.
Segment structure:
The gray matter has projections - horns:
- Front horns (short and wide)
- Rear (narrow and long)
- Lateral (8 cervical, all thoracic and upper 2-3 lumbar segments).
Gray matter is heterogeneous in function. Forms nuclei - compact areas, homogeneous in function:
a) Sensitive nuclei – bodies of interneurons. Their axons transmit sensitive information to the brain (they lie in the dorsal horn and in the central part of the lateral horn).
b) Motor nuclei – bodies of motor neurons. Their axons are directed to the muscles (lie in the anterior horn).
c) Autonomic nuclei - bodies of intercalary vegetative neurons (lie along the periphery of the lateral horns, in segments where there are lateral horns).
Are there any undesirable consequences of cutting this ligament?
The filum terminale is formed by the empty membranes of the spinal cord in its lowest section - the lumbosacral. In a human embryo, the vertebral column and spinal cord are the same length, and they are separated by membranes - hard, arachnoid and soft. During normal growth, the adult vertebral column is approximately 20 cm longer than the spinal cord. The membranes that separate the spinal cord from the spinal column in the sacrum and lumbar region, hard, arachnoid and soft, no longer contain the spinal cord and gather into something like a fibrous cord, forming the filum terminale; this end of the spinal cord resembles a sock that we pulled halfway onto our leg, and the empty part of this sock can be cut off without any harm to the leg. In the same way, the filum terminale of the spinal cord can be cut in any part without any consequences (1, 2).
Based on the book: Degenerative-dystrophic lesions of the spine (radiation diagnostics, complications after disectomy)
Rameshvili T.E. , Trufanov G.E., Gaidar B.V., Parfenov V.E.
Spinal column
The spinal column is normally a flexible formation, consisting in the average version of 33-34 vertebrae, connected into a single chain by intervertebral discs, facet joints and powerful ligaments.
The number of vertebrae in adults is not always the same: there are anomalies in the development of the spine associated with both an increase and a decrease in the number of vertebrae. Thus, the 25th vertebra of the embryo in an adult is assimilated by the sacrum, but in some cases it does not fuse with the sacrum, forming the 6th lumbar vertebra and 4 sacral vertebrae (lumbarization - likening the sacral vertebra to the lumbar).
There are also opposite relationships: the sacrum assimilates not only the 25th vertebra but also the 24th, forming 4 lumbar and 6 sacral vertebrae (sacralization). Assimilation can be complete, osseous, incomplete, bilateral or unilateral.
The following vertebrae are distinguished in the spinal column: cervical - 7, thoracic - 12, lumbar - 5, sacral - 5 and coccygeal - 4-5. Moreover, 9-10 of them (sacral - 5, coccygeal - 4-5) are connected motionlessly.
Normally, there is no curvature of the spinal column in the frontal plane. In the sagittal plane, the spinal column has 4 alternating smooth physiological curves in the form of arcs convexly directed anteriorly (cervical and lumbar lordosis) and arcs convexly directed posteriorly (thoracic and sacrococcygeal kyphosis).
The normal anatomical relationships in the spinal column are evidenced by the severity of physiological curves. The physiological curves of the spine are always smooth and are not normally angular, and the spinous processes are at the same distance from each other.
It should be emphasized that the degree of curvature of the spinal column in different parts is not the same and depends on age. Thus, at the time of birth, curves of the spinal column exist, but their severity increases as the child grows.
Vertebra
A vertebra (except for the two upper cervical ones) consists of a body, an arch and processes extending from it. The vertebral bodies are connected by intervertebral discs, and the arches are connected by intervertebral joints. The arches of adjacent vertebrae, joints, transverse and spinous processes are connected by a powerful ligamentous apparatus.
The anatomical complex, consisting of an intervertebral disc, two corresponding intervertebral joints and ligaments located at this level, represents a unique segment of spinal movements - the so-called. spinal motion segment. The mobility of the spine in a single segment is small, but the movements of many segments provide the possibility of significant mobility of the spine as a whole.
The dimensions of the vertebral bodies increase in the caudal direction (from top to bottom), reaching a maximum in the lumbar region.
Normally, the vertebral bodies have the same height in the anterior and posterior sections.
An exception is the fifth lumbar vertebra, the body of which is wedge-shaped: in the ventral section it is higher than in the dorsal section (higher in the front than in the back). In adults, the body has a rectangular shape with rounded corners. In the transitional thoracolumbar spine, a trapezoidal body of one or two vertebrae may be detected with a uniform bevel of the upper and lower surfaces anteriorly. The lumbar vertebra may have a trapezoidal shape with a posterior slope of the upper and lower surfaces. A similar shape to the fifth vertebra is sometimes mistaken for a compression fracture.
The vertebral body consists of spongy substance, the bone beams of which form a complex interweaving, the vast majority of them have a vertical direction and correspond to the main lines of load. The anterior, posterior and lateral surfaces of the body are covered with a thin layer of dense substance perforated by vascular canals.
An arch extends from the superolateral sections of the vertebral body, in which two sections are distinguished: the anterior, paired - pedicle and the posterior - plate (Iamina), located between the articular and spinous processes. The following processes extend from the vertebral arch: paired - upper and lower articular (arcicular) processes, transverse and single - spinous.
The described structure of the vertebra is schematic, since individual vertebrae not only in different sections, but also within the same section of the spinal column may have distinctive anatomical features.
A feature of the structure of the cervical spine is the presence of holes in the transverse processes of the CII-CVI vertebrae. These openings form a canal through which the vertebral artery passes with the sympathetic plexus of the same name. The medial wall of the canal is the middle part of the semilunar processes. This should be taken into account when the deformation of the semilunar processes increases and arthrosis of the uncovertebral joints occurs, which can lead to compression of the vertebral artery and irritation of the sympathetic plexuses.
Intervertebral joints
Intervertebral joints are formed by the lower articular processes of the overlying vertebra and the upper articular processes of the underlying vertebra.
The facet joints in all parts of the spinal column have a similar structure. However, the shape and location of their articular surfaces are not the same. Thus, in the cervical and thoracic vertebrae they are located in an oblique projection, close to the frontal, and in the lumbar vertebrae - to the sagittal. Moreover, if in the cervical and thoracic vertebrae the articular surfaces are flat, then in the lumbar vertebrae they are curved and look like segments of a cylinder.
Despite the fact that the articular processes and their articular surfaces in various parts of the spinal column have unique features, at all levels the articulating articular surfaces are equal to one another, lined with hyaline cartilage and reinforced by a tightly stretched capsule, attached directly to the edge of the articular surfaces. Functionally, all arcuate joints are classified as low-moving.
In addition to the facet joints, the true joints of the spine include:
- paired atlanto-occipital joint connecting the occipital bone with the first cervical vertebra;
- unpaired median atlanto-axial joint connecting vertebrae CI and CII;
- paired sacroiliac joint connecting the sacrum to the iliac bones.
Intervertebral disc
The bodies of adjacent vertebrae from the second cervical to the first sacral are connected by intervertebral discs. The intervertebral disc is cartilaginous tissue and consists of a pulpous nucleus (nucleus pulposus), a fibrous ring (annulus fibrosis) and two hyaline plates.
The nucleus pulposus is a spherical formation with an uneven surface, consists of a gelatinous mass with a high water content - up to 85-90% in the nucleus, its diameter ranges from 1-2.5 cm.
In the intervertebral disc in the cervical region, the nucleus pulposus is displaced slightly anterior to the center, and in the thoracic and lumbar spine it is located on the border of the middle and posterior third of the intervertebral disc.
The nucleus pulposus is characterized by great elasticity and high turgor, which determines the height of the disc. The core is compressed in a disk under pressure of several atmospheres. The main function of the nucleus pulposus is a spring: acting like a buffer, it weakens and evenly distributes the influence of various shocks and shocks over the surfaces of the vertebral bodies.
Thanks to its turgor, the nucleus pulposus exerts constant pressure on the hyaline plates, pushing the vertebral bodies apart. The ligamentous apparatus of the spine and the fibrous ring of the discs counteract the nucleus pulposus, bringing adjacent vertebrae closer together. The height of each disc and the entire spinal column as a whole is not a constant value. It is associated with the dynamic balance of oppositely directed influences of the nucleus pulposus and the ligamentous apparatus and depends on the level of this balance, which corresponds primarily to the state of the nucleus pulposus.
The tissue of the nucleus pulposus is capable of releasing and binding water depending on the load, and therefore at different times of the day the height of a normal intervertebral disc is different.
Thus, in the morning, the height of the disc increases with the restoration of the maximum turgor of the nucleus pulposus and, to a certain extent, overcomes the elasticity of the traction of the ligamentous apparatus after an overnight rest. In the evening, especially after physical activity, the turgor of the nucleus pulposus decreases and adjacent vertebrae come closer together. Thus, a person’s height changes during the day depending on the height of the intervertebral disc.
In an adult, intervertebral discs make up approximately a quarter or even a third of the height of the spinal column. The noted physiological fluctuations in growth during the day can be from 2 to 4 cm. Due to the gradual decrease in turgor of the nucleus pulposus in old age, growth decreases.
The peculiar dynamic counteraction of the influences on the spinal column of the nucleus pulposus and the ligamentous apparatus is the key to understanding a number of degenerative-dystrophic lesions developing in the spine.
The nucleus pulposus is the center around which mutual movement of adjacent vertebrae occurs. When the spine flexes, the core moves posteriorly. When extending anteriorly and when bending sideways - towards the convexity.
The fibrous ring , consisting of connective tissue fibers located around the nucleus pulposus, forms the anterior, posterior and lateral edges of the intervertebral disc. It is attached to the bony marginal edging through Sharpei fibers. The fibers of the annulus fibrosus are also attached to the posterior longitudinal ligament of the spine. The peripheral fibers of the annulus fibrosus make up the strong outer part of the disc, and the fibers located closer to the center of the disc are more loosely located, passing into the capsule of the nucleus pulposus. The anterior section of the fibrous ring is denser and more massive than the posterior one. The anterior part of the fibrous ring is 1.5-2 times larger than the posterior one. The main function of the fibrous ring is to fix adjacent vertebrae, hold the nucleus pulposus inside the disc, and ensure movement in different planes.
The cranial and caudal (upper and lower, respectively, in a standing position) surface of the intervertebral disc is formed by hyaline cartilaginous plates inserted into the limbus (thickening) of the vertebral body. Each of the hyaline plates is equal in size and tightly adjacent to the corresponding end plate of the vertebral body; it connects the nucleus pulposus of the disc with the bony end plate of the vertebral body. Degenerative changes in the intervertebral disc spread to the vertebral body through the endplate.
Ligamentous apparatus of the spinal column
The spinal column is equipped with a complex ligamentous apparatus, which includes: anterior longitudinal ligament, posterior longitudinal ligament, yellow ligaments, intertransverse ligaments, interspinous ligaments, supraspinous ligament, nuchal ligament and others.
The anterior longitudinal ligament covers the anterior and lateral surfaces of the vertebral bodies. It starts from the pharyngeal tubercle of the occipital bone and reaches the 1st sacral vertebra. The anterior longitudinal ligament consists of short and long fibers and bundles, which are firmly fused with the vertebral bodies and loosely connected with the intervertebral discs; above the latter, the ligament is thrown from one vertebral body to another. The anterior longitudinal ligament also serves as the periosteum of the vertebral bodies.
The posterior longitudinal ligament begins from the upper edge of the foramen magnum, lines the posterior surface of the vertebral bodies and reaches the lower part of the sacral canal. It is thicker, but narrower than the anterior longitudinal ligament and richer in elastic fibers. The posterior longitudinal ligament, unlike the anterior one, is firmly fused with the intervertebral discs and loosely fused with the vertebral bodies. Its diameter is not the same: at the level of the discs it is wide and completely covers the posterior surface of the disc, and at the level of the vertebral bodies it looks like a narrow ribbon. On the sides of the midline, the posterior longitudinal ligament passes into a thin membrane that separates the venous plexus of the vertebral bodies from the dura mater and protects the spinal cord from compression.
The ligamentum flavum consists of elastic fibers and connects the vertebral arches; they are especially clearly visualized on MRI in the lumbar spine, about 3 mm thick. The intertransverse, interspinous, and supraspinous ligaments connect the corresponding processes.
The height of the intervertebral discs gradually increases from the second cervical vertebra to the seventh, then a decrease in height is observed to ThIV and reaches a maximum at the level of the LIV-LV disc. The smallest heights are found in the uppermost cervical and upper thoracic intervertebral discs. The height of all intervertebral discs located caudal to the ThIV vertebral body increases uniformly. The presacral disc is very variable both in height and shape; deviations in one direction or another in adults are up to 2 mm.
The height of the anterior and posterior sections of the disc in different parts of the spine is not the same and depends on the physiological bends. Thus, in the cervical and lumbar regions, the anterior part of the intervertebral discs is higher than the posterior one, and in the thoracic region the opposite relationships are observed: in the middle position, the disc has the shape of a wedge, with its apex facing backwards. With flexion, the height of the anterior part of the disc decreases and the wedge-shaped shape disappears, and with extension, the wedge-shaped shape is more pronounced. There is normally no displacement of the vertebral bodies during functional tests in adults.
Spinal canal
The spinal canal is a container for the spinal cord, its roots and vessels; the spinal canal communicates cranially with the cranial cavity, and caudally with the sacral canal. For the exit of the spinal nerves from the spinal canal there are 23 pairs of intervertebral foramina. Some authors divide the spinal canal into a central part (dural canal) and two lateral parts (right and left lateral canals - intervertebral foramina).
In the side walls of the canal there are 23 pairs of intervertebral foramina, through which the roots of the spinal nerves and veins exit the spinal canal and the radicular-spinal arteries enter. The anterior wall of the lateral canal in the thoracic and lumbar regions is formed by the posterolateral surface of the bodies and intervertebral discs, and in the cervical region this wall also includes the uncovertebral joint; posterior wall – the anterior surface of the superior articular process and facet joint, yellow ligaments. The upper and lower walls are represented by cuttings of the legs of the arches. The upper and lower walls are formed by the inferior notch of the pedicle of the overlying vertebra and the superior notch of the pedicle of the underlying vertebra. The diameter of the lateral canal of the intervertebral foramina increases in the caudal direction. In the sacrum, the role of intervertebral foramina is played by four pairs of sacral foramina, which open on the pelvic surface of the sacrum.
The lateral (radicular) canal is limited externally by the pedicle of the overlying vertebra, in front by the vertebral body and intervertebral disc, and behind by the ventral sections of the intervertebral joint. The radicular canal is a semi-cylindrical groove about 2.5 cm long, running from the central canal from top to bottom and anteriorly. The normal anteroposterior size of the canal is at least 5 mm. There is a division of the root canal into zones: the “entry” of the root into the lateral canal, the “middle part” and the “exit zone” of the root from the intervertebral foramen.
The “3rd entrance” to the intervertebral foramen is the lateral recess. The reasons for root compression here are hypertrophy of the superior articular process of the underlying vertebra, congenital features of the development of the joint (shape, size), osteophytes. The serial number of the vertebra to which the superior articular process belongs in this type of compression corresponds to the number of the pinched spinal nerve root.
The “middle zone” is limited in front by the posterior surface of the vertebral body, in the back by the interarticular part of the vertebral arch, the medial sections of this zone are open towards the central canal. The main causes of stenosis in this area are osteophytes at the site of attachment of the ligamentum flavum, as well as spondylolysis with hypertrophy of the articular capsule of the joint.
In the “exit zone” of the spinal nerve root, the underlying intervertebral disc is located in front, and the outer parts of the joint are behind. The causes of compression in this area are spondyloarthrosis and subluxations in the joints, osteophytes in the area of the upper edge of the intervertebral disc.
Spinal cord
The spinal cord begins at the level of the foramen magnum of the occipital bone and ends, according to most authors, at the level of the middle of the body of the LII vertebra (rarely occurring variants are described at the level of LI and the middle of the body of the LIII vertebra). Below this level is the terminal cistern containing the roots of the cauda equina (LII-LV, SI-SV and CoI), which are covered by the same membranes as the spinal cord.
In newborns, the end of the spinal cord is located lower than in adults, at the level of the LIII vertebra. By 3 years of age, the conus spinal cord occupies its usual adult location.
The anterior and posterior roots of the spinal nerves arise from each segment of the spinal cord. The roots are directed to the corresponding intervertebral foramina. Here the dorsal root forms the spinal ganglion (local thickening - ganglion). The anterior and posterior roots join just after the ganglion to form the spinal nerve trunk. The upper pair of spinal nerves leaves the spinal canal at the level between the occipital bone and the CI vertebra, the lower pair - between the SI and SII vertebrae. There are a total of 31 pairs of spinal nerves.
Up to 3 months, the spinal cord roots are located opposite the corresponding vertebrae. Then the spine begins to grow more rapidly compared to the spinal cord. In accordance with this, the roots become longer towards the conus of the spinal cord and are located obliquely downwards towards their intervertebral foramina.
Due to the lag in the growth of the spinal cord in length from the spine, this discrepancy should be taken into account when determining the projection of the segments. In the cervical region, the spinal cord segments are located one vertebra higher than their corresponding vertebra.
There are 8 spinal cord segments in the cervical spine. Between the occipital bone and the CI vertebra there is a segment C0-CI where the CI nerve passes. The spinal nerves corresponding to the underlying vertebra emerge from the intervertebral foramen (for example, the CVI nerves emerge from the intervertebral foramen CV-CVI).
There is a discrepancy between the thoracic spine and the spinal cord. The upper thoracic segments of the spinal cord are located two vertebrae higher than their corresponding vertebrae, and the lower thoracic segments are three. The lumbar segments correspond to the ThX-ThXII vertebrae, and all sacral segments correspond to the ThXII-LI vertebrae.
The continuation of the spinal cord from the level of the LI vertebra is the cauda equina. The spinal roots arise from the dural sac and diverge inferiorly and laterally to the intervertebral foramina. As a rule, they pass near the posterior surface of the intervertebral discs, with the exception of the roots LII and LIII. The spinal root LII emerges from the dural sac above the intervertebral disc, and the spinal root LIII exits below the disc. The roots at the level of the intervertebral discs correspond to the underlying vertebra (for example, the level of the LIV-LV disc corresponds to the LV root). The intervertebral foramen includes roots corresponding to the overlying vertebra (for example, LIV-LV corresponds to the LIV root).
It should be noted that there are several places where the roots can be affected in posterior and posterolateral herniated intervertebral discs: the posterior part of the intervertebral discs and the intervertebral foramen.
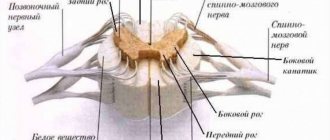
The spinal cord is covered by three meninges: dura mater spinalis, arachnoid (arachnoidea) and pia mater spinalis. The arachnoid and pia mater together are also called leptomeningeal membrane.
The dura mater consists of two layers. At the level of the foramen magnum, the two layers completely separate. The outer layer is tightly adjacent to the bone and is, in fact, periosteum. The inner layer forms the dural sac of the spinal cord. The space between the layers is called epidural (cavitas epiduralis), peridural or extradural.
The epidural space contains loose connective tissue and venous plexuses. Both layers of the dura mater are brought together as the spinal nerve roots pass through the intervertebral foramina. The dural sac ends at the level of the SII-SIII vertebrae. Its caudal part continues as the filum terminale, which is attached to the periosteum of the coccyx.
The arachnoid mater consists of a cell membrane to which a network of trabeculae is attached. The arachnoid membrane is not fixed to the dura mater. The subarachnoid space is filled with circulating cerebrospinal fluid.
The pia mater lines all surfaces of the spinal cord and brain. The trabeculae of the arachnoid membrane are attached to the pia mater.
The upper border of the spinal cord is the line connecting the anterior and posterior segments of the CI vertebral arch. The spinal cord ends, as a rule, at the level LI-LII in the form of a cone, below which there is a cauda equina. The roots of the cauda equina emerge at an angle of 45° from the corresponding intervertebral foramen.
The dimensions of the spinal cord are not the same along its entire length; its thickness is greater in the area of the cervical and lumbar thickening. The sizes vary depending on the part of the spine:
- at the level of the cervical spine - the anteroposterior size of the dural sac is 10-14 mm, the spinal cord is 7-11 mm, the transverse size of the spinal cord is close to 10-14 mm;
- at the level of the thoracic spine - the anteroposterior size of the spinal cord corresponds to 6 mm, the dural sac - 9 mm, with the exception of the level of the ThI-Thll vertebrae, where it is 10-11 mm;
- in the lumbar spine - the sagittal size of the dural sac varies from 12 to 15 mm.
Epidural fatty tissue is more developed in the thoracic and lumbar parts of the spinal canal.
Are there any other effects of spinal cord traction?
Tension of the filum terminale not only provokes syringomyelia , but also generates a flexion reflex in the spinal column, leading to scoliosis . To avoid strain on the spinal cord, it forces the lower part of the brain, the so-called tonsils of the cerebellum, to descend down the foramen magnum, through which the cranium communicates with the spinal column. This causes Arnold-Chiari malformation , a disease described 100 years ago, the cause of which remains unknown.
Number of spinal cord segments. Their skeletopy
Anatomy of the spinal cord, number of segments:
a) Cervical – 8 segments.
b) Thoracic – 12 segments.
c) Lumbar – 5 segments.
d) Sacral – 5 segments.
e) Coccygeal – 1 segment.
Skeletotopy of spinal cord segments according to Shipo’s rule:
- Segments C1-C4 are projected to the level of their vertebra.
- Segments C5-C8 are projected 1 vertebra higher.
- The upper thoracic segments are 2 vertebrae higher. The lower thoracic vertebrae are 3 vertebrae higher.
- Lumbar segments at the level of T11-T12 vertebrae.
- Sacral and 1 coccygeal segment at level - L1.
What happens to a syringomyelic cyst?
In syringomyelia , dissection of the filum terminale of the spinal cord delays the development of the disease. A cyst formed as a result of cell death may remain unchanged, but it may disappear with the spontaneous opening of the space surrounding the spinal cord, or it may move into its central canal, where there is an ependymal canal, through which the central canal of the spinal cord communicates with the cavities of the brain . Syringomyelia symptoms are caused by cell death and the toxic tumor effect of the cyst. Cutting the filum terminale of the spinal cord has two beneficial effects: it delays cell death that was caused by the tension on the spinal cord, and it reduces the toxic tumor effect of the cyst on the spinal cord.
Classification of the spinal cord pathways; patterns of their location in the spinal cord
Conducting pathways are a two-way connection between the SC and the GM. The conduction function occurs after the formation of the brain.
Patterns of location:
1) Ascending pathways:
- Sensitive.
- Occupy the posterior funiculi, and are also located on the periphery of the lateral funiculi of the SC.
— Transmit sensitive information from receptors.
2) Descending pathways:
- Motor.
- Occupy the anterior cords, as well as the central part of the lateral cords of the SC.
- Transmits motor impulses to muscles.
Classification of pathways by function:
— Sensitive
- Motor.
Bibliography
- Dr. Miguel B. Royo Salvador (1996), Siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas, etiología común (PDF). REV NEUROL (Barc); 24 (132): 937-959.
- Dr. Miguel B. Royo Salvador (1996), Platibasia , impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia , la escoliosis , la malformación de Arnold-Chiari , el kinking del tronco cerebral, el retroceso odontoideo, la impresión basilar y la platibasia idiopáticas (PDF). REV NEUROL; 25 (140): 523-530
- M. B. Royo-Salvador, J. Solé-Llenas, J. M. Doménech, and R. González-Adrio, (2005) “Results of the section of the filum terminale in 20 patients with syringomyelia , scoliosis and Chiari malformation .” (PDF). Acta Neurochir (Wien) 147:515–523.
- M. B. Royo-Salvador (1992), “Aportación a la etiología de la siringomielia ,” Tesis doctoral (PDF). Universidad Autónoma de Barcelona.
- M. B. Royo-Salvador (2014), “Filum System® Bibliography” (PDF).
- M. B. Royo-Salvador (2014), “Filum System® Guía Breve.”
What types of receptors are divided into according to localization and according to their perception of irritation? Their localization
A receptor is an anatomical structure that converts external or internal stimuli into a nerve impulse.
Classification of receptors according to their perception of irritation:
1. Distant – vision, hearing, taste;
2. Contact.
By localization:
- Extrareceptors – surface of the skin of the body (tactile, temperature).
- Intrareceptors – internal organs (pain, desire to eat).
- Proprioceptors – ODA (muscle tendons, joint capsules).