Intercostal neuralgia is a disease in which irritation or compression of the intercostal nerves occurs. This can happen for various reasons. The disease is relatively rare, its main manifestation is pain along the affected nerve.
Our expert in this field:
Lashch Natalia Yurievna
Neurologist of the highest category, candidate of medical sciences, associate professor. Laureate of the Moscow City Prize in the field of medicine.
Call the doctor Reviews about the doctor
How are intercostal nerves arranged? What functions do they perform?
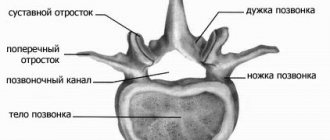
Two nerve roots emerge from the spinal cord: the anterior one is formed by the processes of motor nerve cells, the posterior one - by sensory ones. Then, while still inside the spinal canal of the spine, these roots are connected to form the spinal ganglion. Two spinal nerves depart from it: anterior and posterior.
In the thoracic spinal cord, the anterior branches of the spinal nerves pass into the intercostal nerves. They pass in the spaces between the ribs - each of them is located along the lower edge of the corresponding rib - and, unlike the anterior spinal roots, are mixed, that is, they are responsible for both movement and sensitivity:
- provide movement of the chest muscles involved in the breathing process;
- provide sensitivity to the skin of the chest and upper abdomen.
Clinical anatomy of the spine and spinal cord (Part 2)
Spinal cord
It is located along the length from the foramen magnum to the upper edge of the second (very rarely third) lumbar vertebra. Its average length is 45 cm. In most people, the SM ends at the level of L2, in rare cases reaching the lower edge of the 3rd lumbar vertebra. (Fig. 1.17).
| Rice. 1.17. Spinal cord, spinal nerves and filum terminale. Horizontal bars indicate the percentage of samples that end at the level shown. |
An anterior medial groove runs along the anterior surface of the spinal cord, which in cross section appears to project into the spinal cord to a depth of 3 mm. (Fig. 1.18)
| Rice. 1.18. Cross-section of the spinal canal at the T11 level. 1. Dentate ligament 2. Posterior medial septum 3. Anterior medial fissure 4. Posterior longitudinal ligament 5. Pia mater 6. Dura mater 7. Subdural space 8. Arachnoid membrane 9. Subarachnoid space 10. Ventral nerve root 11. Dorsal root nerve 12. Dorsal root ganglia 13. Anterior meningeal branch of the epidural and subarachnoid space 14. Epinervium (continuation of the dura mater) 15. White branch 16. Gray branch 17. Spinal nerve T11 |
Blood supply to the spinal cord
The spinal cord is supplied by the spinal branches of the vertebral, deep cervical, intercostal and lumbar arteries. (Fig. 1.19)
| Fig.1.19. Arterial support of the spinal cord. 1. Vertebral artery 2. Deep cervical artery 3. Superior intercostal artery 4. Intercostal artery 5. Anterior spinal artery 6. Posterior spinal artery 7. Anterior and posterior radicular arteries 8. Spinal branch of the intercostal artery 9. Artery of Adamkiewicz |
The anterior radicular arteries enter the spinal cord alternately - sometimes on the right, sometimes on the left (usually on the left). The posterior spinal arteries are upward and downward oriented continuations of the posterior radicular arteries. The branches of the posterior spinal arteries are connected by anastomosis with similar branches of the anterior spinal artery, forming numerous choroid plexuses in the pia mater (pial vasculature). (Fig. 1.20 and 1.21)
| Fig.1.20. Arterial support of the spinal cord, anterior view. 1. Intercostal artery 2. Spinal branch of the intercostal artery 3. Anterior and posterior radicular arteries 4. Anterior spinal artery 5. Posterior spinal artery |
| Rice. 1.21 | |
| A. Blood supply to the spinal cord, posterior view. 1. Spinal branch of the intercostal artery 2. Anterior and posterior radicular arteries 3. Posterior spinal artery 4. Anterior spinal artery | B. Cross section of the spinal cord showing the blood supply. 1. Anterior spinal artery 2. Anterior spinal vein 3. Posterior spinal artery 4. Posterior radicular artery 5. Anterior and posterior arteries 6. Spinal branch of the intercostal artery |
The type of blood supply to the spinal cord depends on the level of entry into the spinal canal of the largest diameter radicular (radiculomedullary) artery - the so-called artery of Adamkiewicz. Various anatomical options for blood supply to the spinal cord are possible, including one in which all segments of the spinal cord below Th 2-3 are fed from one artery of Adamkiewicz (option a
, about 21% of all people).
In other cases, the following are possible: b
) an inferior accessory radiculomedullary artery accompanying one of the lumbar or 1st sacral roots,
c
) an upper accessory artery accompanying one of the thoracic roots,
d
) a loose type of supply to the spinal cord (three or more anterior radiculomedullary arteries) .
As in option a
, and in option
c,
the lower half of the spinal cord is supplied by only one artery of Adamkiewicz. Damage to this artery, compression by an epidural hematoma, or persistent constriction (when using adrenaline as an adjuvant) can cause serious and irreversible neurological consequences.
Blood flows from the SM through the tortuous venous plexus (Fig. 1.22), which is also located in the soft membrane and consists of six longitudinally oriented vessels. This plexus communicates with the internal vertebral plexus of the epidural space from which blood flows through the intervertebral veins into the azygos and semi-gyzygos vein systems. (Fig. 1.23)
| Rice. 1.22. Cross section of the thorax showing venous drainage of the vertebrae and spinal cord. | Rice. 1.23. Venous drainage from the vertebrae. |
The entire venous system of the epidural space does not have valves, so it can serve as an additional system for the outflow of venous blood, for example, in pregnant women with aortocaval compression.
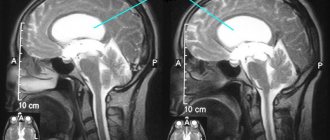
Cerebrospinal fluid
The spinal cord is bathed by CSF, which plays a shock-absorbing role, protecting it from injury. (Fig. 1.36) CSF is an ultrafiltrate of blood (clear, colorless liquid) that is formed by the choroidal plexus in the lateral, third and fourth ventricles of the brain. The rate of CSF production is about 500 ml per day, so even the loss of a significant volume is quickly compensated.
| Rice. 1.36. Circulation of cerebrospinal fluid. Arrows indicate the direction of cerebrospinal fluid flow. 1. Arachnoid granulation 2. Dura mater (outer layer) 3. Dura mater (inner layer) 4. Subdural space o 5. Arachnoid membrane 6. Subarachnoid space 7. Superior sagittal sinus 8. Pia mater 9. Choroid plexus 3 th ventricle 10. Great cerebral vein 11. Cisterna cerebellomedullaris 12. Interventricular canal 13. Intercerebellar capacitance 14. Aqueduct of Sylvius 15. Capacity of the great cerebral vein ( cisterna ambiens) 16. Choroidal plexus of the 4th ventricle 17. Magendie canal |
CSF contains proteins and electrolytes (mainly Na + and Cl -) and at 37 ° C has a specific gravity of 1.003-1.009.
| Physicochemical properties of CSF | |
| pH | 7,3 |
| total volume (adults) | 150 ml |
| specific gravity | 1,003-1,009 |
| CSF pressure (side position) | 60-80 mmHg |
| protein | 18-41 mg/dl |
| glucose | 50-75 mg/dl |
| sodium | 137-153 mmol/l |
| potassium | 2.6-3.3 mmol/l |
| calcium | 1.02-1.34 mmol/l |
| magnesium | 0.9-1.2 mmol/l |
| chloride | 120-130 mmol/l |
Arachnoid (Pachionian) granulations, located in the cerebral venous sinuses, drain most of the CSF. The rate of CSF absorption depends on the pressure in the subarachnoid space. When this pressure exceeds the pressure in the venous sinus, thin tubes in the pachyonic granulations open, allowing CSF to flow into the sinus. After the pressure equalizes, the lumen of the tubes closes. Thus, there is a slow circulation of CSF from the ventricles into the subarachnoid space and further into the venous sinuses. A small portion of CSF is absorbed by the veins of the subarachnoid space and lymphatic vessels, so some local circulation of CSF occurs in the vertebral subarachnoid space. CSF absorption is equivalent to its production, so the total CSF volume is usually in the range of 130-150 ml.
There may be individual differences in the volume of CSF in the lumbosacral parts of the spinal canal, which may influence the distribution of arterial fluid. It is interesting to note that overweight people have lower CSF volume. There is a clear correlation between CSF volume and the effect of SA, in particular, the maximum extent of the block and the rate of its regression.
Spinal roots and spinal nerves
Each nerve is formed by the connection of the anterior and posterior roots of the spinal cord. The dorsal roots have thickenings - the dorsal root ganglia, which contain the nerve cell bodies of the somatic and autonomic sensory nerves. The anterior and dorsal roots separately pass laterally through the arachnoid and dura mater before uniting at the level of the intervertebral foramina to form the mixed spinal nerves. There are 31 pairs of spinal nerves in total: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and one coccygeal. (Fig. 1.24)
| Rice. 1.24. The relationship of the spinal column to the sources of nerve roots from the spinal cord. |
Each nerve is formed by the union of the ventral and dorsal roots, which in turn consists of several processes associated with the spinal cord (Fig. 1.25). Each ventral and dorsal root passes separately through the arachnoid and dura mater, then uniting at or near the intervertebral foramina and thus forming a mixed spinal nerve.
| Fig.1.25. The processes of the dorsal roots and the roots of the spinal nerve. |
Each dorsal root has a thickening, the dorsal root ganglion, which contains the nerve cells of the somatic and autonomic sensory nerves. The dorsal root ganglia are located at varying distances from the spinal cord and may be located lateral to the point where the two roots join.
Once the two roots are connected, the sensory and motor nerve fibers intertwine according to their possible destination. They are organized into a bundle, each containing a different number of nerve fibers.
Each fiber is surrounded by connective tissue, the endonervium, and each bundle is surrounded by the perinervium. The tissue covering the set of bundles, the so-called mixed nerve, is called epinervium (Fig. 1.26). These components of the connective tissues of the nerves are formed from the membranes of the spinal cord.
| Rice. 1.26. 1. Epinervium 2. Fat cell 3. Bundle 4. Perinervium 5. Endonervium 6. Schwann cell membrane 7. Axon 8. Schwann cell nucleus 9. Myelinated nerve fiber |
The spinal cord grows slower than the spinal column, so it is shorter than the spine. As a result, the segments and vertebrae are not in the same horizontal plane. Since the segments of the spinal cord are shorter than the corresponding vertebrae, in the direction from the cervical segments to the sacral segments the distance that the spinal nerve must overcome in order to reach “its” intervertebral foramen gradually increases. At the level of the sacrum, this distance is 10-12 cm. (Fig. 1.27) Therefore, the lower lumbar roots lengthen and bend caudally, forming a cauda equina together with the sacral and coccygeal roots.
| Rice. 1.27. |
Within the subarachnoid space, the roots are covered only by a layer of pia mater. Individual features of the anatomy of the spinal roots may determine the variability of the effects of SA and EA. The size of the nerve roots can vary significantly among different people. In particular, the diameter of the spine L 5 can vary from 2.3 to 7.7 mm. The posterior roots are larger in size compared to the anterior ones, but consist of trabeculae, which are quite easily separated from each other. Due to this, they have a larger contact surface and greater permeability for MA compared to thin anterior roots that do not have a trabecular structure. These anatomical features partly explain the easier achievement of sensory block compared to motor block.
Segmental distribution of spinal nerves
The spinal nerves leaving the spinal cord through the intervertebral foramina immediately divide into anterior and posterior branches. The posterior one innervates the skin and muscles of the back, the anterior one innervates the rest of the body. Each spinal segment provides innervation to a specific area of skin (dermatome), specific muscles (myotome) and bones (osteotome). (Fig. 1.28)
| Rice. 1 28. |
Segmental innervation of joints and muscles is presented in Table 1.
Table 1. Segmental innervation of joints and muscles.
| Shoulder joint | S6-8 |
| Elbow joint | S5-8 |
| Wrist joint | S6-7 |
| Joints of the hand and fingers | C7-8, Th1 |
| Intercostal muscles | Th1-11 |
| Diaphragm | S3-5 |
| Abdominal muscles | Th7-12 |
| Hip flexors | L1-3 |
| Hip extensors | L5, S1 |
| Knee flexors | L5, S1 |
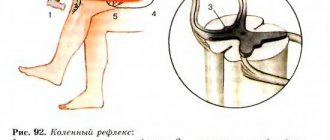
| Knee extensors | L3-4 |
| Foot flexors | L4-5 |
| Foot extensors | S1-2 |
The cutaneous distribution of spinal nerves is shown in Figure 1.29.
| Fig.1.29. Dermatomal distribution of spinal nerves. This figure is derived from several authoritative sources and should be considered as a rough guide only. |
The skin zones of innervation of adjacent segments largely overlap each other.
Autonomic nervous system
Spinal anesthesia can cause widespread blockade of both sympathetic and parasympathetic nerves. This significantly affects the control of blood flow as well as the normal functioning of the gastrointestinal tract (Fig. 1.30). In addition, afferent autonomic visceral nerves are involved in the transmission of pain impulses from the abdominal region and must be blocked if complete analgesia is to be achieved. Finally, blockade of the autonomic support of the endocrine glands can greatly modify the response of these glands to surgical stress.
| Rice. 1.30. Sympathetic efferent nerves. A. Sympathetic ganglia from T6-L2 B. Abdominal ganglion C. Superior mesenteric (mesenteric) ganglion D. Aortorenal ganglion E. Internal mesenteric ganglion F. Pelvic ganglion 1. The end of the celiac nerve 2. Theismic celiac nerve 3. The native nerve 4. First lumbar celiac nerve 5. The sexual nerve 6. The pastry surrounding the gastroduodenal artery 7. Bryushin's plexus 8. The top mesenterial plexus 9. The top of the backward plexus is 10. There is a mesenterial weeds of the thumb plexus 11. Superior hypogastric plexus 12. Inferior hypogastric plexus (pelvic plexus) |
Sympathetic nervous system
Efferent impulses from the central nervous system to blood vessels and internal organs are carried out by sympathetic fibers running as part of the preganglionic and postganglionic nerves. Pre- and postganglionic fibers form synapses within the ganglion. Ganglia are located in the sympathetic chain and large nerve plexuses, such as the cardiac, celiac, and hypogastric.
Preganglionic fibers arise from nerve cells located in the lateral columns of the SC. They leave the SC as part of the anterior nerve roots along the length from Th1 to L2. Immediately behind the intervertebral foramen, preganglionic fibers, which have a thin myelin sheath, leave the spinal nerves and form connecting branches that are part of the sympathetic chain. In its composition, they spread up and down, forming synapses with the corresponding ganglia.
The sympathetic trunk runs along the anterolateral surfaces of the vertebral bodies. (Fig. 1.22 and Fig. 1.31)
| Rice. 1.31. Sympathetic efferent nerves. 1. Superior cervical ganglia 2. Middle cervical ganglia 3. Stellate (cervicothoracic) ganglia 4. Peritoneal ganglia 5. Superior mesenteric ganglia 6. Inferior mesenteric ganglia 7. Superior hypogastric plexus |
In the chest, fibers extend from it to the splanchnic nerves, which penetrate the diaphragm and reach the ganglia in the celiac and aortorenal plexuses.
In the abdominal cavity, the sympathetic trunk forms connections with the celiac, aortic and hypogastric plexuses. The trunk ends on the anterior surface of the sacrum. Unmyelinated postganglionic fibers arise from the ganglia and widely distribute to all organs that have sympathetic innervation. The segmental distribution of visceral sympathetic nerves is presented in Table 2. Table 2. Segmental distribution of visceral sympathetic nerves.
| Head, neck, upper limbs | Th1-5 |
| Heart | Th1-5 |
| Lungs | Th2-4 |
| Esophagus (lower part) | Th5-6 |
| Stomach | Th6-10 |
| Small intestine | Th9-10 |
| Colon | Th9-10 |
| Liver and gallbladder | Th7-9 |
| Pancreas and spleen | Th6-10 |
| Kidneys and ureters | Th10 - L2 |
| Adrenal glands | Th8 - L1 |
| Testicles and ovaries | Th10 – 11 |
| Bladder | Th11 - L2 |
| Prostate | Th11 - L2 |
| Uterus | Th10 - L1 |
Parasympathetic nervous system
The efferent and afferent nerves of the parasympathetic system come from the cranial nerves (mainly the vagus), as well as from the 2nd, 3rd and 4th pairs of sacral nerves. (Fig. 1.32 and Fig. 1.33) The branches of the vagus nerve innervate the heart, lungs, esophagus, and a significant part of the gastrointestinal tract to the transverse colon. The branches of the sacral nerves, running parallel to the sympathetic ones, innervate the large intestine downward from the transverse colon, the bladder, sphincters and reproductive organs.
| Fig.1.32. Schematic diagram of the efferent component of the parasympathetic nervous system to the small and large intestines. 1. Vagus nerve 2. Superior vagal ganglia 3. Inferior vagal ganglia 4. Peritoneal ganglia and plexus 5. Hepatic plexus surrounding the common hepatic artery 6. Plexus surrounding the gastroduodenal artery 7. Superior mesenteric ganglia and plexus 8. Inferior mesenteric ganglia and plexus 9.Superior hypogastric plexus 10.Inferior hypogastric plexus (pelvic plexus) 11.Pelvic ganglia 12.Pelvic splanchnic nerves |
| Figure 1.33. Schematic diagram of the efferent components of the parasympathetic nervous system. 1. Pharyngeal plexus 2. Superior vagal ganglia 3. Inferior vagal ganglia 4. Abdominal ganglia 5. Abdominal plexus 6. Mesenteric ganglia 7. Superior hypogastric plexus 8. Inferior hypogastric plexus |
Unlike other autonomic nerves, the vagus nerve cannot be blocked by EA.
Autonomic (visceral) afferent nerves
Together with the efferent nerves of the sympathetic and parasympathetic systems, afferent fibers are distributed, the cells of which are located in the dorsal root ganglia. (Fig. 1.34 and Fig. 1.35) These fibers are responsible for the afferent arc of visceral reflexes. They are involved in the formation of such sensations as nausea, bladder distension, and uterine contractions. With the participation of these fibers, sensations of certain types of pain are formed, such as intestinal colic and pain during childbirth. They are activated by inflammatory processes (peritonitis) or ischemia.
| Rice. 1.34. Schematic diagram of afferent sympathetic pathways from the heart. 1. Superior cervical ganglia 2. Middle cervical ganglia 3. Stellate ganglia | Rice. 1.35. Afferent parasympathetic nerve pathways from the stomach through the vagus nerve. 1. Superior vagal ganglia 2. Inferior vagal ganglia |
… Previous page
Treatment of intercostal neuralgia
How to treat intercostal neuralgia? Therapy is carried out in two directions:
- It is necessary to alleviate the main symptom of the disease - chest pain.
- At the same time, it is necessary to identify the cause - the disease that led to compression or irritation of the nerve - and treat it.
In the acute stage of the disease, the doctor prescribes bed rest and recommends sleeping on a flat and firm bed. To combat pain, non-steroidal anti-inflammatory drugs are used, and various ointments help. In case of severe pain, a novocaine blockade is performed: the place where the affected nerve is located is injected with an anesthetic solution. There are also special patches with anesthetics.
Vitamins are prescribed to improve the condition of nervous tissue, muscle relaxants to relieve muscle spasms. Prolonged pain leads to a person becoming overly excitable and nervous, in which case sedatives are prescribed. Physiotherapy procedures help: Sollux, electrophoresis, UHF. A neurologist can prescribe massage and acupuncture sessions.
Is it possible to cope with the disease on your own? Over-the-counter pain medications and folk remedies can help relieve pain for a while. But in order to prescribe truly effective treatment for intercostal neuralgia on the right or left, you need to understand what causes it. Improper self-medication can be harmful.
We will call you back
Message sent!
expect a call, we will contact you shortly
The main symptom of intercostal neuralgia is pain. It spreads along the rib, as if encircling the right or left half of the chest, and can be sharp, stabbing, burning, or dull, aching. The pain intensifies during inhalation, because of this the person cannot breathe deeply. Movements, changes in body position, coughing, and sneezing also lead to aggravation.
Painful sensations occur if you press on certain points between two adjacent ribs along their course. This symptom is checked by a neurologist during an examination.
Other possible symptoms of intercostal neuralgia on the right and left (as well as pain, occur in the area of the affected nerve):
- twitching of the chest muscles;
- increased sweating;
- redness or paleness of the skin;
- numbness.
With intercostal neuralgia on the left, a person may complain that his heart and stomach hurt. Pain may radiate under the shoulder blade, to the collarbone area.
Similar chest pains can occur with diseases of the heart, lungs, pleura, and spine. An incorrect diagnosis and lost time can lead to serious consequences.
Heart disease or pinched nerve?
Therefore, intercostal neuralgia causes pain not only in the heart, but also in the lower back, back, and also under the shoulder blade.
With intercostal neuralgia, irritation or compression of the roots of the intercostal nerves occurs at the point where they exit the spine. Also, pain in the heart area can be caused by excessive tone of one or more muscles of the shoulder, back or shoulder blade.
The causes of neuralgia are varied: exposure to heavy metals, certain medications, bacterial toxins, diseases of the nervous system (polyradiculoneuritis, multiple sclerosis, etc.), trauma, various infections (tuberculosis, influenza, etc.), spinal pathology or congenital anomalies (hernias). discs, osteochondrosis, etc.), allergies.
Another cause of intercostal neuralgia can be changes in the spine, which are caused by hormonal disorders in women. The development of the disease can be affected by alcohol abuse, metabolic disorders of B vitamins, and diabetes mellitus. Older people are susceptible to this disease when all of the above reasons affect the background of age-related changes in the blood vessels.
It should be remembered that nerve endings are everywhere, so intercostal neuralgia can imitate, for example, lung diseases, renal colic, pain that occurs with herpes zoster and, most often, cardiac pathologies. Conversely, other diseases are often mistaken for neuralgia with similar symptoms.
How to eliminate pain
Treatment prescribed for intercostal neuralgia must be comprehensive. First, the causes of the disease should be corrected or eliminated. During an exacerbation, bed rest is required for three days. The bed should be firm and level; it is better to place a shield under the mattress.
During attacks, it is necessary to place mustard plasters on the paravertebral area or wrap the chest with a warm scarf. If the pain intensifies, then you should take analgesics (sedalgin, analgin, etc.). It is also recommended to take B vitamins.
To prevent intercostal neuralgia from becoming chronic, it is necessary to reduce physical activity, try to avoid stressful situations and not abuse alcohol.
How to distinguish intercostal neuralgia from heart disease
Pain during angina occurs quickly and also passes quickly (within 2-5 minutes), it can be relieved with nitroglycerin. Heart pain does not change when moving or changing position, when exhaling or taking a deep breath, it is accompanied by an irregular pulse and an increase or decrease in blood pressure.
To clarify the cause of chest pain, magnetic resonance imaging and radiography should be done.
If pain is felt under the left shoulder blade, you will need a cardiogram. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
How to distinguish the signs of intercostal neuralgia from the symptoms of other diseases?
It is especially important to distinguish in time between irritation of the intercostal nerves and angina pectoris, a condition in which the heart muscle does not receive enough oxygen-rich blood. Main differences:
- With intercostal neuralgia, pain persists for a long time. With angina pectoris, they last about 5 minutes and go away if you take nitroglycerin.
- With neuralgia, pain intensifies during deep inspiration, movements, sneezing and coughing, but with angina pectoris this does not happen.
Other dangerous conditions that need to be distinguished from intercostal neuralgia are myocardial infarction and PE ( pulmonary embolism) . Typically, a heart attack occurs after physical exertion or after a person becomes very nervous. The pain is accompanied by signs of dysfunction of the cardiovascular system:
- The man turns pale. Fingertips, nose, lips may become bluish.
- Sticky cold sweat appears.
- Shortness of breath that persists even when the person is resting - lying or sitting.
- Blood pressure drops.
- The fear of death arises.
You should not engage in self-diagnosis - erroneous conclusions are fraught with serious consequences. See your doctor. Get examined at the clinic. In any case where there is a suspicion of a heart attack, it is better to play it safe and immediately call an ambulance.
Plexus of spinal nerves
parts of the scrotum (or labia majora in women). The genital-femoral nerve (LI-LII) pierces the psoas major muscle at the level of the third lumbar vertebra and divides into the genital and femoral branches. The genital branch follows in front of the external iliac artery, enters the inguinal canal (lies behind the spermatic cord in men or the round ligament of the uterus in women). In men, it innervates the levator testis muscle, the skin of the scrotum and its fleshy membrane, and the skin of the superomedial surface of the thigh. In women, this branch innervates the round ligament of the uterus, the skin of the labia majora and the superomedial surface of the thigh (in the area of the outer ring of the femoral canal). The femoral branch passes through the vascular lacuna to the thigh, adjacent to the anterolateral semicircle of the femoral artery, pierces the ethmoidal fascia and innervates the skin in the area of the subcutaneous fissure and under the inguinal ligament.
The lateral cutaneous nerve of the thigh (LI-II) emerges from under the lateral edge of the psoas major muscle (or pierces it), descends along the iliacus muscle towards the inguinal ligament, passes under its lateral part to the thigh, where its terminal branches innervate the skin of the posteroinferior surface of the gluteal area and lateral surface of the thigh (to the level of the knee joint). The obturator nerve (LII-IV) is a large nerve that runs along the medial edge of the psoas major muscle and descends into the pelvic cavity. joins the blood vessels of the same name, and together with them passes through the obturator canal to the thigh, where it is located between the adductor muscles. It has two terminal branches: the anterior one innervates the adductor brevis and longus, the pectineus and gracilis muscles, and gives the cutaneous branch to the skin of the lower sections of the medial surface of the thigh; the posterior branch innervates the obturator externus and adductor magnus muscles, as well as the capsule of the hip joint.
The femoral nerve is the largest branch of the lumbar plexus. It is formed at the level of the V lumbar vertebra on the anterior internal surface of the psoas major muscle from three roots, crosses this muscle, descends along the iliacus muscle to the inguinal ligament, passes under it through the muscle lacuna to the thigh. In the femoral triangle it is located lateral to the femoral vessels, separated from the femoral artery by a deep layer of the lata fascia of the thigh. Below the inguinal ligament it divides into its terminal branches: muscular, anterior cutaneous and saphenous nerve of the thigh. The muscle branches innervate the sartorius, quadriceps and pectineus muscles of the thigh. The anterior cutaneous branches branch in the skin of the anteromedial surface of the thigh. The saphenous nerve - the longest branch of the femoral nerve - goes along with the femoral artery into the adductor canal, exits through its anterior opening together with the descending genicular artery, descends between the adductor major and vastus medialis muscles to the medial surface of the leg, gives off the popliteal branch along the way, innervating the skin of the knee joint area, stretches down next to the great saphenous vein, innervating the skin of the anteromedial surface of the leg and the medial edge of the foot (to the big toe).
Table 3. Nerves of the lumbar plexus.
Treatment of symptoms of intercostal neuralgia on the right and left
The leading symptom of the disease – pain – is helped by painkillers (non-steroidal anti-inflammatory drugs), anesthetic patches, novocaine blockades, and physiotherapy.
But coping with the symptoms does not mean curing the disease. Therefore, treatment should also be aimed at the cause. A thorough diagnosis must first be carried out - this is only possible in a clinical setting.
Take care of yourself, book a consultation now
Message sent!
expect a call, we will contact you shortly
“Intercostal neuralgia” is not one specific diagnosis, but a collective term. It refers to different conditions that lead to damage to the intercostal nerves and, as a result, to chest pain.
Why is it important to understand the cause of this condition in each specific case? This will allow you to prescribe effective treatment that will help you recover or keep your chronic disease under control.
The main causes of intercostal neuralgia
Most often, the following reasons lead to compression and irritation of the intercostal nerves:
- Osteochondrosis. A degenerative disease that primarily affects the intervertebral discs. Their height decreases - the distance between adjacent vertebrae decreases, this leads to compression of the nerve roots.
- Hypothermia, exposure to drafts.
- Intense physical activity, sudden awkward movements.
- Working in an awkward position when your back is constantly under tension.
- Injuries to the chest and thoracic spine, previous surgeries.
- Frequent and severe stress.
- Viral infections. The most common cause is a cold, shingles.
- Chronic spasm of the back muscles. It promotes irritation of nerve receptors.
Most often, intercostal neuralgia occurs in older people, when the causes of the disease are layered with age-related changes in the spine and blood vessels.
What other diseases lead to girdle pain in the chest?
Often people tend to dub “neuralgia” any girdle pain along the ribs. But this symptom may have other causes, including:
- Spondylosis is an inflammatory disease that causes damage to the vertebral bodies and deformation of the spinal column.
- Hormonal spondylopathy is a pathology that develops in older people, for example, in women after menopause. The spine is deformed, and disorders occur in the vessels that supply it.
- Malignant tumors - those that arise in the spine itself or metastases from other parts of the body.
- Ankylosing spondylitis is a chronic inflammatory process that leads to decreased mobility in the spinal column.
- Gastritis and other diseases of internal organs.
How does the treatment of intercostal neuralgia depend on the cause?
With intercostal neuralgia, it is not enough to eliminate the main symptom of the disease - pain. You should always look for and treat the underlying cause. The doctor prescribes therapy individually, depending on the pathological changes detected during examination and examination, and the final diagnosis.
Make an appointment at the Medica24 International Clinic - get a consultation with an experienced neurologist and undergo an examination using our modern equipment. This will help to quickly and accurately establish a diagnosis and prescribe the correct treatment in a timely manner.
Get a consultation with a doctor
Message sent!
expect a call, we will contact you shortly
The main manifestation of intercostal neuralgia – chest pain – can also occur with many other diseases. And figuring out the correct diagnosis is not always easy.
The diagnostic process begins with a visit to a neurologist. The doctor will ask you some questions:
- When did you first experience pain? How did this happen? What preceded this?
- What is the nature of the pain, when does it usually occur, how often, how long does it last?
- Do you have chronic lung or heart diseases? Are you monitoring your blood pressure?
- What infections have you had? Have you had any chest injuries or surgery?
- What other symptoms bother you?
You may be asked to complete a special “pain questionnaire”. The doctor will perform a complete neurological examination to rule out other neurological diseases. You will then be given an examination.
To understand the causes of irritation or compression of the intercostal nerve, the doctor may prescribe x-rays, CT, MRI, and, if necessary, other studies.
Journal of Experimental and Clinical Surgery
In the treatment of patients with umbilical hernias, many surgeons use prosthetic methods of plastic surgery of the hernial orifice, among which the so-called posterior separation hernioplasty is known, when a mesh prosthesis is placed in the layer between the rectus abdominis muscles and the posterior leaves of their aponeurotic vagina [1, 2]. The results of using this technique in comparison with analogues are characterized by a low incidence of early postoperative complications [2].
As posterior separation hernioplasty has been introduced into clinical practice, the number of reports on the high incidence of chronic pain syndrome in the postoperative period has increased [2], the development of which is often caused by damage to the intercostal nerves during separation of the posterior layers of the aponeurotic sheath from the rectus abdominis muscles [3].
To reduce the possible risk of injury to the intercostal nerves during hernia repair for umbilical hernias, it is necessary to take into account the features of their typical and variant anatomy in the periumbilical region of the anterior abdominal wall [4-7], which, however, are not sufficiently covered in the available literature.
In connection with the above, the goal to study the features of the topography of the intercostal nerves in the peri-umbilical region of the anterior abdominal wall.
Materials and methods
The work was performed on 88 unfixed corpses of individuals of both sexes without signs of pathology of the anterior abdominal wall. The study was approved by the ethics committee at Voronezh State Medical University. N.N. Burdenko" of the Ministry of Health of the Russian Federation. A total of 40 corpses of males (45% of observations) who died at the age of 53.8±11.9 years, and 48 corpses of females (55%) who died at the age of 51.9±13.2 years were examined.
Taking into account the goal at the autopsy of each corpse, a topographic-anatomical dissection of the intercostal nerves in the peri-umbilical region of the anterior abdominal wall was carried out with the determination of the level of their penetration into the rectus abdominis muscles along the vertical axis (relative to the lower edge of the costal arch) and the horizontal axis (relative to the outer edge of the rectus abdominis muscle ).
When statistically processing the research results, the arithmetic mean (M) and standard error of the mean (m) were determined. The significance of differences between quantitative variables was determined using the Kruskal-Wallis test. To determine the significance of differences between categorical variables, a 2 × 2 table was used with the determination of the Pearson test (χ2). Differences were considered significant at a confidence level of at least 95% (p≤0.05).
Research results and discussion
According to the results of this study, most often 2 pairs of intercostal nerves were observed in the peri-umbilical region of the anterior abdominal wall (n=52; 60% of observations), somewhat less often - 1 pair of nerves (n=18; 20%). In 10 (11%) cases, 3 pairs of intercostal nerves approached the rectus abdominis muscles, and in 2 (2%) cases, 4 pairs of nerves were encountered. In 6 (7%) cases, an asymmetric number of intercostal nerves was noted: 1 nerve on the right and 2 on the left (n=2); 2 nerves on the right and 1 on the left (n=2); 2 nerves on the right and 3 on the left (n=2).
Next, the number of intercostal nerves in the peri-umbilical region of the anterior abdominal wall in individuals of different sexes was studied (Table 1). It was found that in females, 2 pairs of intercostal nerves were most often found here (71% of observations). In turn, in males, 2 pairs of intercostal nerves were noted in 45% of cases, and 1 pair – in 35%.
Rice. 1. Typical options for the number of intercostal nerves in the peri-umbilical region of the anterior abdominal wall (schematic images): a – 1 pair of nerves, b – 2 pairs of nerves, c – 3 pairs of nerves, d – 4 pairs of nerves.
Designations: 1 – intercostal nerve, 2 – tendon jumper, 3 – linea alba, 4 – rectus abdominis muscle, 5 – lateral abdominal muscles.
Fig. 1. Typical variants of the number of intercostal nerves in the umbilical region of anterior abdominal wall (schematic image): a – 1 pair of nerves, b – 2 pairs of nerves, c – 3 pairs of nerves, d – 4 pairs of nerves.
1 – intercostal nerve, 2 – intersection tendinea, 3 – linea alba, 4 – rectus abdominis,
5 – lateral abdominal muscles.
Rice. 2. Atypical variants of the number of intercostal nerves in the peri-umbilical region of the anterior abdominal wall (schematic images): a – 1 nerve on the right and 2 on the left, b – 2 nerves on the right and 1 on the left, c – 2 nerves on the right and 3 on the left. Designations: 1 – intercostal nerve, 2 – tendon jumper, 3 – linea alba, 4 – rectus abdominis muscle, 5 – lateral abdominal muscles.
Fig. 2. Atypical variants of the number intercostal nerves in the umbilical region of anterior abdominal wall (schematic image): a – 1 nerve on right and 2 – on left, b – 2 nerve on the right and 1 – on left, c – 2 nerve on right and 3 – on left.
1 – intercostal nerve, 2 – intersection tendinea, 3 – linea alba, 4 – rectus abdominis,
5 – lateral abdominal muscles.
Table 1
Number of intercostal nerves depending on gender, abs. (%)
| Floor | Options for the number of nerves | ||||
| 1 pair | Two pairs | 3 pairs | 4 pairs | Asymmetry | |
| Male | 14 (35) | 18 (45) | 3 (15) | 2 (5) | – |
| Female | 4 (8) | 34 (71)* | 4 (8) | – | 6 (13)* |
* – differences between male and female samples are significant at p<0.001
Table 1
Number of intercostal nerves depending on the gender, absolute number (%)
| Gender | Variants number nerves | ||||
| 1 pair | 2 pair | 3 pair | 4 pair | Asymmetry | |
| Male | 14 (35) | 18 (45) | 3 (15) | 2 (5) | – |
| Female | 4 (8) | 34 (71)* | 4 (8) | – | 6 (13)* |
* – differences between the samples of male and female with significant p<0.001
After this, in the peri-umbilical region of the anterior abdominal wall, options for the penetration of intercostal nerves into the rectus abdominis muscles were studied (Fig. 1). In the studied topographic-anatomical material, lateral (n=46; 52% of observations), posterior (n=34; 39%) and combined (n=8; 9%) variants of penetration of the intercostal nerves into the rectus abdominis muscles were found. In the case of the lateral variant, the intercostal nerves entered the thickness of the rectus abdominis muscles through their outer edges. The posterior version differed in that the intercostal nerves crossed the rectus muscles from behind, and then penetrated into their thickness. In each observation with a combined variant, different pairs of intercostal nerves penetrated into the thickness of the rectus abdominis muscles either from their outer edges or from their posterior surface.
Rice. 3. Options for the penetration of intercostal nerves into the thickness of the rectus abdominis muscles (schematic images): a – lateral, b – posterior.
Designations: 1 – transverse abdominal muscle, 2 – external oblique abdominal muscle, 3 – internal oblique abdominal muscle, 4 – intercostal nerve, 5 – rectus abdominis muscle, 6 – linea alba.
Fig. 3. Variants penetration intercostal nerves into the tissue of rectus abdominis
(schematic image): a – lateral, b – posterior.
1 – transverse abdominis muscle, 2 – abdominal external oblique muscle,
3 – abdominal internal oblique muscle, 4 – intercostal nerve, 5 – rectus abdominis,
6 – linea alba.
Then the features of penetration of intercostal nerves into the rectus abdominis muscles were studied depending on the number of pairs of nerves (Table 2). It was found that in persons with 1 pair of intercostal nerves, the lateral variant of penetration of the nerve trunks into the rectus abdominis muscles was significantly more often observed. In observations with 2 pairs of intercostal nerves, as well as with an asymmetric number of nerve trunks, lateral and posterior variants of nerve penetration into the rectus abdominis muscles were equally often observed. In persons with 3 pairs of intercostal nerves, the posterior variant of penetration of intercostal nerves was significantly more often observed. In the presence of 4 pairs of intercostal nerves, a combination of lateral (lower pairs of nerves) and posterior (upper pairs of nerves) variants of nerve penetration into the rectus abdominis muscles was noted.
table 2
Variants of penetration of intercostal nerves into the rectus abdominis muscles, abs. (%)
| Options for the number of nerves | Options for nerve penetration | ||
| Side | Rear | Combined | |
| 1 pair | 16 (78)* | 2 (22) | – |
| Two pairs | 26 (50) | 20 (38) | 6 (12) |
| 3 pairs | – | 10 (100)* | – |
| 4 pairs | – | – | 2 (100)* |
| Asymmetry | 4 (67) | 2 (33) | – |
* – differences between the variants of penetration of intercostal nerves into the rectus abdominis muscles are significant at p<0.005
Table 2
Variants penetration of the intercostal nerves in rectus abdominis, absolute number (%)
| Variants number nerves | Variants penetration of the intercostal nerves | ||
| Lateral | Posterior | Combined | |
| 1 pair | 16 (78)* | 2 (22) | – |
| 2 pair | 26 (50) | 20 (38) | 6 (12) |
| 3 pair | – | 10 (100)* | – |
| 4 pair | – | – | 2 (100)* |
| Asymmetrical number | 4 (67) | 2 (33) | – |
* – differences between the versions of penetration of the intercostal nerves in rectus abdominis significant p<0.005
Next, the characteristics of the penetration of intercostal nerves into the rectus abdominis muscles were studied depending on gender (Table 3). It turned out that in males, the lateral variant of penetration of the intercostal nerves into the rectus abdominis muscles was significantly more often observed (60% of observations). In females, no significant differences were observed between the variants of penetration of intercostal nerves into the rectus abdominis muscles.
Table 3
Variants of penetration of intercostal nerves into the rectus abdominis muscles depending on gender, abs. (%)
| Floor | Options for nerve penetration | ||
| Side | Rear | Combined | |
| Male | 24 (60)* | 8 (20) | 8 (20) |
| Female | 22 (46) | 26 (54) | – |
* – differences between the variants of penetration of intercostal nerves into the rectus abdominis muscles are significant at p<0.005
Table 3
Variants penetration of the intercostal nerves in rectus abdominis depending on the gender, absolute number abs. (%)
| Gender | Variants penetration of the intercostal nerves | ||
| Lateral | Posterior | Combined | |
| Male | 24 (60)* | 8 (20) | 8 (20) |
| Female | 22 (46) | 26 (54) | – |
* – differences between the versions of penetration of the intercostal nerves in rectus abdominis significant p<0.005
At the next stage of work, the level of penetration of intercostal nerves into the thickness of the rectus abdominis muscles along the vertical and horizontal axes was studied. It was found that the distance from the lower edge of the costal arch to the point of penetration of the intercostal nerves into the rectus abdominis muscles decreases with an increase in the total number of nerve trunks (Table 4). It further turned out that the distance from the outer edge of the rectus abdominis muscle to the point of penetration of the terminal branches of the intercostal nerves into the muscle layer is anatomically constant (Table 5).
Table 4
Distance from the lower edge of the costal arch to the point of penetration of the intercostal nerve into the rectus abdominis muscle, cm (M±m)
| Number of nerve pairs | 1 nerve | 2nd nerve | 3rd nerve | 4th nerve |
| 1 | 6,9±0,2 | – | – | – |
| 2 | 5,8±0,2* | 8,5±0,2 | – | – |
| 3 | 4,6±0,2* | 8,0±0,3* | 13,6±0,5 | – |
| 4 | 3,1±0,2** | 7,5±0,2* | 12,4±0,3* | 16,8±0,5 |
* – differences between variants of the number of intercostal nerves are significant at p<0.01; ** – differences between variants of the number of intercostal nerves are significant at p<0.005
Table 4
The distance from the lower edge of the costal arch to the point of penetration of the intercostal nerve in rectus abdominis, cm (M±m)
| Number of pairs nerves | 1 nerve | 2 nerve | 3 nerve | 4 nerve |
| 1 | 6,9±0,2 | – | – | – |
| 2 | 5,8±0,2* | 8,5±0,2 | – | – |
| 3 | 4,6±0,2* | 8,0±0,3* | 13,6±0,5 | – |
| 4 | 3,1±0,2** | 7,5±0,2* | 12,4±0,3* | 16,8±0,5 |
* – difference between number variants of the intercostal nerves significant p<0.01; ** – difference between number variants of the intercostal nerves significant p<0.005
Table 5
Distance from the outer edge of the rectus abdominis muscle to the point of penetration of the intercostal nerve into its thickness, cm (M±m)
| Number of nerve pairs | 1 nerve | 2nd nerve | 3rd nerve | 4th nerve |
| 1 | 1,8±0,2 | – | – | – |
| 2 | 1,6±0,1 | 1,6±0,1 | – | – |
| 3 | 1,7±0,5 | 1,4±0,2 | 1,8±0,5 | – |
| 4 | 3,1±0,5 | 2,4±0,5 | – | – |
Table 5
The distance from the lateral edge of rectus abdominis muscle to the point of penetration of the intercostal nerve in muscle, cm (M±m)
| Number of pairs nerves | 1 nerve | 2 nerve | 3 nerve | 4 nerve |
| 1 | 1,8±0,2 | – | – | – |
| 2 | 1,6±0,1 | 1,6±0,1 | – | – |
| 3 | 1,7±0,5 | 1,4±0,2 | 1,8±0,5 | – |
| 4 | 3,1±0,5 | 2,4±0,5 | – | – |
Next, the level of penetration of intercostal nerves into the thickness of the rectus abdominis muscles along the vertical and horizontal axes was studied, depending on the gender of the person. It was found that the distance from the lower edge of the costal arch to the point of penetration of the intercostal nerves into the rectus abdominis muscles was significantly greater in females (Table 6). At the same time, the distance from the outer edge of the rectus abdominis muscle to the point of penetration of the intercostal nerves into the muscle thickness is much greater in males (Table 7).
Table 6
Distance from the lower edge of the costal arch to the point of penetration of the intercostal nerve into the rectus abdominis muscle, cm (M±m)
| Floor | 1 nerve | 2nd nerve | 3rd nerve | 4th nerve |
| Male | 5,1±0,3 | 7,9±0,3 | 11,7±0,6 | 16,8±0,5 |
| Female | 5,6±0,2* | 8,4±0,3* | 12,5±0,7* | – |
* – differences between male and female samples are significant at p<0.01
Table 6
The distance from the lower edge of the costal arch to the point of penetration of the intercostal nerve in rectus abdominis, cm (M±m)
| Gender | 1 nerve | 2 nerve | 3 nerve | 4 nerve |
| Male | 5,1±0,3 | 7,9±0,3 | 11,7±0,6 | 16,8±0,5 |
| Female | 5,6±0,2* | 8,4±0,3* | 12,5±0,7* | – |
* – differences between the samples of male and female with significant p<0.01
Table 7
Distance from the outer edge of the rectus abdominis muscle to the point of penetration of the intercostal nerve into its thickness, cm (M±m)
| Floor | 1 nerve | 2nd nerve | 3rd nerve | 4th nerve |
| Male | 2,2±0,2* | 1,8±0,1* | 2,7±0,5* | 3,4±0,5 |
| Female | 1,6±0,1 | 1,4±0,1 | 1,3±0,3 | – |
* – differences between male and female samples are significant at p<0.005
Table 7
The distance from the lateral edge of the rectus abdominis muscle to the point of penetration of the intercostal nerve in muscle, cm (M±m)
| Gender | 1 nerve | 2 nerve | 3 nerve | 4 nerve |
| Male | 2,2±0,2* | 1,8±0,1* | 2,7±0,5* | 3,4±0,5 |
| Female | 1,6±0,1 | 1,4±0,1 | 1,3±0,3 | – |
* – differences between the samples of male and female with significant p<0.005
conclusions
- In the peri-umbilical region of the anterior abdominal wall, the number of intercostal nerves varies from 1 to 4 pairs, but most often 2 pairs of nerves are observed (60% of observations).
- In females, 2 pairs of intercostal nerves are significantly more often observed (71%), while in males, no statistically significant differences were found.
- The intercostal nerves penetrate the rectus abdominis muscles most often through their outer edges (52%), somewhat less often - from their posterior surface (39%).
- In males, the lateral variant of penetration of the intercostal nerves into the rectus abdominis muscles is significantly more often observed (60%), while in females no statistically significant differences have been established.
- The levels of penetration of intercostal nerves into the rectus abdominis muscles relative to the lower edge of the costal arch and the outer edge of the rectus abdominis muscle have been established.
Instrumental methods for diagnosing intercostal neuralgia
At the Medica24 International Clinic, you can undergo examination using our own diagnostic equipment, which meets the most modern standards. It will help diagnose the disease at an early stage and take timely measures.
First of all, it is important to carry out a differential diagnosis of intercostal neuralgia with certain diseases of the spine, cardiovascular system, and lungs. To do this, if necessary, the neurologist will refer you for a consultation with a cardiologist or pulmonologist.
You may be prescribed an ECG, Holter monitoring, cardiac ultrasound, X-ray, CT and MRI of the chest, biochemical blood test, and bacteriological studies.