It is not always possible to determine the cause of painful attacks without visiting a doctor and special examination.
Various forms of neuralgia pose particular difficulties for diagnosis, because... Often the pain with them can radiate anywhere. One of the types of such lesions is neuralgia of the pterygopalatine ganglion.
What is neuralgia of the pterygopalatine ganglion?
Slader's syndrome is an inflammatory lesion of the pterygopalatine nerve ganglion, predominantly of infectious etiology. It got its name from the name of the American scientist who first described it in 1908.
Other options for the name of Slader's syndrome are neuralgia of the pterygopalatine ganglion, ganglionitis of the pterygopalatine ganglion; ICD-10 code: G52.8 (Lesions of other specified cranial nerves).
In 1962, the International Committee on the Classification of Headaches, along with other “atypical” facial pains, classified the pterygopalatine ganglion syndrome into a special group - “pain of the lower part of the head,” or Horton’s syndrome of the lower type.
Ganglionitis (ganglioneuritis) of the pterygopalatine ganglion
Ganglionitis (ganglioneuritis) of the pterygopalatine ganglion is one of the neurodental syndromes. This symptom complex is characterized by significant variability in clinical manifestations. The node has three main roots: somatic (sensitive) - from the second branch of the trigeminal nerve, parasympathetic - from the facial nerve and sympathetic - from the plexus of the internal carotid artery; the latter also has connections with the ciliary, auricular, upper cervical sympathetic nodes and cranial nerves, especially with the trigeminal and facial.
Etiology and pathogenesis.
The pterygopalatine node is affected by inflammatory processes in the main and maxillary sinuses, the ethmoidal labyrinth, since the node is closest to the upper or lower jaw. Toxic effects from tonsillitis, complicated caries and local trauma can cause the disease. Provoking factors are overwork, lack of sleep, loud noise, excitement, alcohol consumption, smoking.
Clinical picture
. Neuralgia of the pterygopalatine ganglion (Slader syndrome) is characterized by spontaneous sharp pain in the eye, around the orbit, in the root of the nose, upper jaw, and sometimes in the teeth and gums of the lower jaw. Pain can spread to the temple, auricle, back of the head, neck, shoulder blade, shoulder, forearm and even hand. Painful paroxysms are accompanied by pronounced vegetative symptoms, a kind of “vegetative storm” (redness of half the face, swelling of the facial tissues, lacrimation, copious discharge of secretions from one half of the nose). The attack lasts from several minutes to several hours, and sometimes 1-2 days. and more. Often painful paroxysms develop at night. One of the important diagnostic signs of damage to the pterygopalatine ganglion is the cessation of the attack after lubricating the posterior parts of the nasal cavity with a solution of cocaine and adrenaline.
The illness continues for months and even years. After an attack, a number of vegetative symptoms remain mild. The variety of clinical manifestations of damage to the pterygopalatine ganglion is explained by its individual anatomical features and numerous anastomoses with various nerve formations of the face and other areas.
Treatment.
In the acute period, the nasal cavity posterior to the middle turbinate is lubricated with a 3-5% cocaine solution. Novocaine is also used: cotton swabs moistened with a 2% novocaine solution are inserted into the nasal cavity. For severe pain, ganglion blockers (benzohexonium, pentamine) are prescribed. In severe cases, they resort to blocking the node using anesthetics. Treatment must be comprehensive. If the syndrome develops against the background of inflammatory processes in the paranasal sinuses, face, mouth and jaws, then anti-infective therapy (antibiotics, sulfonamides) is necessary. Treatment should be carried out against the background of desensitizing drugs (diphenhydramine, suprastin, pipolfen). A good therapeutic effect is achieved with hydrocortisone injections into the area of the node projection. Pachycarpine, antispasmodics, and antipsychotics are prescribed in combination with antidepressants. If the clinical picture is dominated by symptoms of irritation of the parasympathetic part, then anticholinergic drugs are used (platiphylline, antispasmodic, belladonna preparations, metacin, aprofen).
Endonasal electrophoresis of a 2% novocaine solution, UHF therapy, and diadynamic currents are used. After the acute phenomena have subsided, mud applications at low temperatures (36-37°C) are used on the affected side or in the form of a collar. Perform a light massage of the neck and face muscles. B vitamins and biogenic stimulants (aloe extract, PHYBS, vitreous) are indicated. Elderly and senile people are prescribed anti-sclerotic drugs, as well as drugs that improve cerebral and coronary circulation. In severe forms, they resort to blockade of the node using a 2% trimecaine solution or alcoholization. Node destruction is rarely used. The treatment provided does not always relieve patients from relapses of the disease, but the severity of clinical manifestations is significantly reduced.
Etiology: causes of ganglionitis
Among the causes of the inflammatory process in the pterygopalatine node, several factors are distinguished:
- Infectious diseases. Among them are influenza, pleurisy, dysentery, typhoid, malaria, brucellosis, and syphilis.
- Traumatic defeat. For example, injury to the nose or its mucous membrane by foreign bodies.
- Inflammatory processes in the oral cavity, including carious lesions of the dentition.
- Inflammatory diseases of the ENT organs: purulent otitis, chronic rhinitis, tonsillitis, pharyngitis.
- Tumor formations in the maxillary areas.
- Long-term use of corticosteroid drugs.
- Diabetic disease.
- Viral infection. Often, damage to the pterygopalatine node occurs as a consequence of herpetic disease (herpes zoster) or hepatitis.
Clinical picture: symptoms
The symptomatic picture of ganglionitis (Sluder syndrome) is usually due to the underlying cause of the inflammatory process. It also matters where the initial inflammation is located. There are several typical manifestations of this disease.
When examining a patient, the doctor pays attention to the following symptoms:
- One half of the face has a paler or, on the contrary, redder tint.
- Edema.
- Excessive secretion of liquid secretion from the eyes (lacrimation), nose, mouth (hypersalivation) appears on the side where the lesion occurred.
- The patient may experience shortness of breath and suffocation.
- A detailed history taking reveals changes in the functioning of taste buds, because The pterygopalatine ganglion captures part of the facial nerve. A bitter sensation may appear on the base of the tongue and on the back of it.
- Sometimes the disease is accompanied by fainting states and hypertensive crises.
- Muscle tone decreases.
The disease may also be accompanied by symptoms characteristic of ophthalmological diseases: photophobia, swelling of the eyelid, blepharospasm, conjunctivitis, exophthalmos.
Most often, patients themselves complain of pain. Its peculiarity will be that the pain is wave-like in nature. When characterizing the pain syndrome, the patient may say that he experiences a burning sensation, aching, or sensations similar to pain from a burn or severe cut.
This feeling occurs in the front part of the head (in the eye, in the teeth, in the jaws, in the bridge of the nose, tongue, palatine part of the mouth), in the back of the head, near the ear, in the neck, in the hands. Usually pain bothers a person at night.
How is the problem diagnosed?
Slüder syndrome can be confused with other diseases that have a similar symptomatic picture. In addition, pain often radiates to other nearby organs and parts of the body.
Therefore, for proper further treatment, it is important to accurately differentiate this disease from others. Diagnosing yourself and self-medicating can be extremely dangerous .
First of all, you should contact a general practitioner, who will refer the patient to see a neurologist. The doctor will conduct a detailed survey of the patient, visually assess the patient’s condition, palpate sensitive areas and, based on the collected anamnestic data, make a diagnosis.
Also, to differentiate the disease, the patient may be directed to undergo a series of examinations and tests :
- computer and magnetic resonance imaging;
- Ultrasound;
- cardiogram;
- X-ray examination.
To diagnose inflammation of the pterygopalatine node, the method of application to the posterior parts of the nasal cavity with a solution of dicaine and adrenaline with a concentration of 0.1% is also used.
If the pain stops after such a procedure, this indicates that the pathological process occurs precisely in the pterygopalatine node. There are a number of signs that make it possible to distinguish Slader's syndrome from neuralgia of the trigeminal and glossopharyngeal nerves. In the case of the latter, a painful attack can be caused by some local irritation.
Ganglionitis can be confused with cluster headache . Its distinctive features: has a pulsating character in the temporal zone; there is a sensation as if the eyeball is being squeezed out of the socket. It arises suddenly and ends just as abruptly. Attacks of pain occur in series.
Ganglionitis should also be distinguished from cancer, traumatic injuries, heart disease and gastrointestinal tract diseases. Here, various survey methods will provide great information.
Find out more about the types and forms of neuralgia:
- external cutaneous nerve of the thigh and pelvic;
- inflammation of the brachial and sciatic nerves;
- occipital and postherpetic.
Treatment
In the acute period of the disease, pain relief comes first . For this purpose, various medications are used. Anesthetics are used to lubricate the mucous membrane of the posterior wall of the nasal cavity.
Also, to eliminate pain, intravenous infusion of analgin solution with diphenhydramine and trimecaine is used . Intramuscular injections are made with a solution of droperidol and fentanyl. Novocaine blockade of the pterygopalatine node is performed.
If the cause of ganglionitis of the pterygopalatine node is an infectious-inflammatory disease of other organs, it is treated. The oral and nasopharyngeal cavities are sanitized. Other inflammatory diseases are treated with antibiotics and immunomodulators.
It is most advisable to carry out complex therapy aimed at eliminating not only the pain syndrome, but also the accompanying symptoms.
The patient is prescribed the following types of medications:
- vitamin preparations of group B (thiamine chloride, cyanocobalamin);
- anti-inflammatory drugs and pain relievers;
- NSAIDs;
- local anesthetics to the affected area (lidocaine, novocaine);
- external warming ointments and creams;
- To stabilize the patient's mental state, antidepressants (duloxetine) and tranquilizers are recommended.
Physiotherapeutic procedures have proven themselves well in the treatment of Slader syndrome:
- intranasal electrophoresis;
- diadynamic currents;
- acupuncture;
- UHF;
- ultrasound;
- laser therapy;
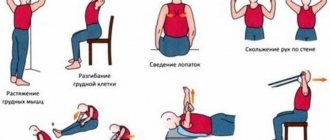
- massage;
- physiotherapy.
The last two points require caution in application, because in some cases may have the opposite effect.
Pterygopalatine ganglion syndrome (Slüder syndrome)
Description
Described in 1908 by the American physician Slyuder. It is known that the pterygopalatine ganglion (ganglion pterygopalatinum) is the formation of the parasympathetic part of the autonomic nervous system. It contains multipolar cells and has three roots:
1) sensitive - nn. pterygopalatini,
2) parasympathetic - n. petrosus mayor, or greater petrosal nerve, carrying secretory fibers to the lacrimal gland, to the glands of the nasal cavity and palate,
3) sympathetic - n.petrosus profundus, a branch of the plexus caroticus internus, containing postganglionic sympathetic nerve fibers from the cervical ganglia.
Orbital branches depart from the node, which penetrate the orbit through the lower orbital fissure and, together with the posterior ethmoidal ones, are directed through small openings in the sutura sphenoethmoidalis to the mucous membrane of the posterior cells of the ethmoidal labyrinth and the sphenoid sinus.
The posterior superior nasal nerves go to the mucous membrane of the posterior sections of the superior and middle nasal concha and nasal passages, the posterior cells of the ethmoid sinus, the mucous membrane of the nasal septum and partly the anterior part of the palate.
The palatine nerves innervate the mucous membrane of the palate, and the lower posterior lateral nasal branches innervate the mucous membrane of the inferior concha, middle and lower nasal passages and the maxillary sinus. Consequently, the branches of the pterygopalatine ganglion innervate the lacrimal gland, the mucous membrane of the hard and soft palate, a larger portion of the nasal mucosa, the posterior cells of the ethmoid bone, the maxillary and main sinuses. The anatomical structure of the pterygopalatine node explains the symptoms of the disease.
The patient appears
sharp shooting pain at the base of the nose, around and behind the eye, in the eye, in the upper and lower jaws, teeth. The pain radiates to the temple, ear, parotid region, especially to the mastoid process. The pain can spread to the neck, shoulder blade, shoulder and forearm, hand and fingertips, and can also be localized in the area of the hard palate and paranasal cavities. But it is most intense in the area of the orbit, root of the nose and mastoid process. The duration of pain ranges from several hours and days to several weeks. At the time of the attack, the patient also complains of a tickling and burning sensation in the nose, attacks of sneezing, runny nose, lacrimation, drooling, dizziness and nausea. There may be asthma-like attacks and taste disturbances.
Objectively noted
severe photophobia, blepharospasm, lacrimation, edema of the upper eyelid, conjunctival hyperemia, mydriasis or miosis, sometimes a short-term increase in intraocular pressure and slight exophthalmos.
The disease can last a long time
- for months and even years. In the interictal period, there is often a dull deep pain in the upper jaw, root of the nose, orbit, swelling of the affected half of the face, increased sweating, hyperemia or paresthesia of the gums, palate, and pharynx. Therefore, some authors believe that disease of the pterygopalatine node is not only neuralgia, but also ganglioneuritis.
Neuralgia of the pterygopalatine node is associated with perifocal infection in the paranasal sinuses and any infectious foci in the oral cavity, purulent otitis, cerebral arachnoiditis, with injuries and foreign bodies in the nose, with turbinate hypertrophy and curvature of the nasal septum, with peritonsillar abscesses, allergies. Irritation of the pterygopalatine node can be caused by general intoxication, viral and rheumatoid infections and maxillary tumors.
You can learn more about the treatment, prevention and restoration of vision from the “Seeing Without Glasses” program from Michael Richardson. The unique method of Natural Recovery will allow you to restore and improve your vision and health up to 100 percent or more. Click here to get rid of diseases forever.
Similar clinical condition
observed in nasociliary nerve syndrome. But when the pterygopalatine node is damaged, there are no anatomical changes in the anterior segment of the eyeball, because its branches do not supply the eyeball, but innervate the nasal cavity and the floor of the orbit. Increased sensitivity of the nasal mucosa is concentrated in the posterior part of the nasal cavity, and not in the anterior one. When the pterygopalatine node is irritated, there are no areas with increased pain sensitivity and no rashes occur.
Differentiate this disease
necessary with other facial neuralgia. Trigeminal neuralgia is characterized by very short paroxysms, shooting pain, spreading along the branches of the trigeminal nerve. The pain is not accompanied by nausea, vomiting and other diencephalic symptoms.
For cervical migraine
pain spreads from the cervical-occipital region to the anterior parts of the head. It is of a permanent nature, intensifies when turning the head, and is combined with radicular syndrome of cervical localization. It occurs more often in middle-aged and elderly people.
For periodic migraine neuralgia
- very intense pain in the frontotemporo-orbital region, strictly one-sided, accompanied by lacrimation, runny nose, and hyperemia of half the face. Lasts from several minutes to several hours. Pain syndrome is a consequence of vasodilation, mainly in the external carotid artery.
Unlike migraine, neuralgia is characterized by periodicity and seasonality of attacks, developing in series several times a day, sometimes at night. There are no cerebral or diencephalic symptoms. Patients rush about in pain, and with migraine they tend to immobility.
Relieves the condition
during an attack of neuralgia, novocaine blockade of the pterygopalatine node with a 2% novocaine solution. The sooner treatment is started, the better. Treatment should be comprehensive and aimed at eliminating the underlying cause of the disease. Prescribe painkillers, anti-infectives, decongestants, corticosteroids, ganglion blockers, anticholinergics, physiotherapeutic procedures (UHF, diathermy, diadynamic currents, etc.), massage of the sore half of the face, nasal electrophoresis with novocaine, B vitamins. It is useful to prescribe anti-sclerotic and vasodilators, t .To. in old age, the disease occurs due to general vascular pathology.
—
Article from the book: Syndromes with simultaneous damage to the organ of vision, oral cavity and dentofacial system | Yartseva N.S., Barer G.M., Gadzhieva N.S.
Prognosis and prevention
Relapses of the disease do not always disappear as a result of treatment, but the clinical picture changes significantly. Many symptoms disappear or appear much less frequently. Treatment must be comprehensive, adequate and timely, only in this case a positive result is possible.
Among preventive measures, there are, first of all, measures aimed at preventing the occurrence of infectious and inflammatory diseases of nearby organs. In this regard, doctors recommend avoiding hypothermia and drafts, which can lead to otitis media, tonsillitis, and pharyngitis.
It is also a good idea to harden the body and increase immunity. In the period between exacerbations, it is important to prevent repeated inflammatory processes.
Since pulpitis and other diseases of the oral cavity often cause damage to the pterygopalatine node, teeth and periodontal diseases should be treated in a timely manner .
It is also worth avoiding, if possible, situations that can lead to trauma to the nasal cavity and its mucous membranes.
An assessment of damage to the pterygopalatine ganglion is possible only after thorough clinical, laboratory and instrumental studies. A correct diagnosis is the basis for successful treatment.
Diagnostics
Certain difficulties in making a diagnosis are explained by multiple QU connections with different structural branches of the nervous system.
In addition, it is necessary to take into account additional factors that can provoke spontaneous occurrence of HCU - stressful situations, alcohol consumption, smoking, overwork and hypothermia, sudden noise exposure.
The key sign of a specific diagnosis of the disease is the cessation of a HCU attack after treatment of the posterior sections of the nasal cavity with a weak solution of tetracaine with epinephrine.
The disease should be differentiated from trigeminal neuralgia, in which attacks are fleeting, their irradiation is not observed, “trigger zones” are present, and local lubrication with an anesthetic does not relieve symptoms.
For certain indications, the organization of collegial consultations with a dentist, rheumatologist, ophthalmologist, and otolaryngologist is encouraged.