Relapsing-remitting multiple sclerosis
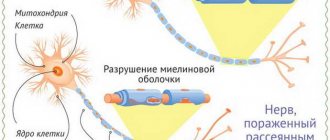
Relapsing-remitting multiple sclerosis (RRMS) is the most common type of multiple sclerosis (MS). This diagnosis is made in approximately 85% of cases [1]. Just like other types of the disease, RRMS occurs when the body's immune system attacks the central nervous system, damaging the protein myelin that protects nerve fibers.
The course of the disease is accompanied by various neurological symptoms, such as [2]:
- increased fatigue;
- gait disturbances;
- visual and oculomotor disorders;
- decreased muscle strength in the limbs;
- disorders of sensitivity, urination, etc.
Symptoms can vary greatly depending on the location of the damaged nerve fibers.
Relapses of RRMS last for at least 24 hours. During the period of relapse, all symptoms intensify, but soon a remission occurs, during which the symptoms partially or completely disappear.
Interesting fact
The reasons for the development of relapsing-remitting multiple sclerosis, like other types of MS, are currently unclear. Most likely, the reasons lie in the combined influence of genetic and environmental factors (smoking, vitamin D deficiency, certain infectious diseases) [3].
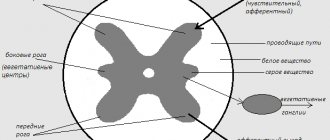
Many different methods are used to diagnose RRMS [4], but there are no specific tests for this type of disease yet. A neurologist will prescribe a comprehensive examination to assess the severity of the disease, determine the type of MS, and prescribe therapy. It will also be necessary to conduct several diagnostic tests, including magnetic resonance imaging (MRI). An MRI will look for areas of damage in the brain and spinal cord that may suggest the presence of MS. In some cases, a collection of cerebrospinal fluid (lumbar puncture) is necessary.
There is currently no cure that can completely and permanently eliminate the symptoms of any type of multiple sclerosis. However, there are various medications that can control the course of the disease. You should also consider staying physically active to help with mobility issues or muscle weakness. An individualized exercise program helps improve physical fitness and quality of life without exacerbation of disease symptoms or relapse [5].
Interesting fact
The basis of therapy is MS course-modifying drugs (MSDs). These drugs affect the pathological process itself - demyelination - and can reduce the frequency or even completely prevent the occurrence of relapses [6].
There are many different medications on the market, but it must be borne in mind that the selection of therapy is strictly individual and is carried out exclusively by a doctor based on the nature of the disease, existing diseases, and also taking into account previously prescribed therapy.
The prognosis for patients with relapsing-remitting multiple sclerosis is usually more favorable than for patients with a progressive form of the disease [7], but the course of the disease must be assessed over time, since damage to the nervous tissue accumulates over time. Approximately two thirds of patients with relapsing-remitting multiple sclerosis develop secondary progressive MS [8]. On average, this occurs 15-20 years after the onset of the disease [9]. It is this progression that is an important factor in predicting the possibility of developing disability [10].
Despite many years of studying multiple sclerosis (MS), this problem remains very relevant. Its medical and social significance is due to the high frequency of the disease, affecting people of young working age with relatively rapid disability with insufficient effectiveness in some cases of existing therapeutic agents.
Thanks to significant progress in understanding the mechanisms of development of the pathological process in MS, as well as biotechnological methods for creating new drugs and the availability of unified criteria for the timely diagnosis of MS, it has become possible to early prescribe specific pathogenetic treatment aimed at both relieving the symptoms of exacerbation and modulating the course of the disease .
Currently, the generally accepted diagnostic criteria for MS are those proposed by W. McDonald et al. in 2001, refined in 2005, and then revised in 2010 [48] (see table).
In early clinical manifestations of the disease, when there is no typical relapsing course, it is important to exclude alternative diagnoses [8].
Various combinations of neurological symptoms and MRI findings can be observed in patients with clinically isolated syndrome (CIS), which is currently defined as a monophasic symptomatology thought to be caused by an inflammatory demyelinating disease. In this case, monophasicity implies the first development of a separate clinical episode with a relatively rapid onset. It is possible to simultaneously detect multiple clinical/paraclinical manifestations, but dissemination over time should not be obvious. In this regard, the modern classification of CIS distinguishes the following options: type 1 – clinically monofocal, at least 1 asymptomatic MRI lesion; type 2 – clinically multifocal, at least 1 asymptomatic MRI lesion; type 3 – clinically monofocal; MRI may be without pathology; no asymptomatic MRI lesions; type 4 – clinically multifocal; MRI may be without pathology; no asymptomatic MRI lesions; type 5 – there are no clinical manifestations of demyelinating disease, but there are changes on MRI that suggest the presence of CIS [42].
Considering the significant difficulties in making a diagnosis of MS in atypical cases, a clinical and morphological study was carried out at the Scientific Center of Neurology of the Russian Academy of Medical Sciences in the pseudotumorous course of MS and acute focal demyelination. 43 patients were observed, in 32 of whom the diagnosis was clarified based on histological examination of surgical material obtained during stereotactic biopsy or surgery. Groups with pseudotumor monofocal process were identified; with a combination of a pseudotumor focus with subclinical multifocal demyelination; with the development of a pseudotumorous course during exacerbation of reliable MS; 11 patients were diagnosed as a result of a comprehensive study and dynamic observation.
It turned out to be possible to identify the following clinical features of the pseudotumor course:
demyelinating process: the age of onset of the disease typical for MS, the same incidence of the disease in men and women, predominantly hemispheric localization of the pseudotumor lesion with a subacute course of the disease. A morphological study of biopsy and surgical material revealed changes in brain tissue characteristic of an acute focal demyelinating process, the main signs of which are the destruction of myelin fibers of the white matter with the removal of their breakdown products by lipophages, proliferation and hypertrophy of astrocytes producing glial fibers, inflammatory perivascular infiltrates consisting from lymphocytes, monocytes and a few plasma cells, hyperemia of small vessels and capillaries, swelling of brain tissue. It has been established that the decay of axons in the focus of demyelination occurs already at the very early stages of the development of demyelinating disease. The data obtained made it possible to clarify the algorithm for examining patients with the pseudotumor type of the pathological process and certain approaches to the tactics of managing these patients. Thus, if ambiguous CT and MRI data are detected at the onset of pseudotumor demyelinating disease, an additional comprehensive examination of the patient is recommended, including high-field MRI of the brain, cervical and thoracic spine, and registration of evoked brain potentials to exclude “dissemination of the pathological process in space.” In the case of the development of a pseudotumor variant of the disease within the framework of CIS with multifocal brain damage or with reliable MS, it is advisable to carry out pulse therapy with methylprednisolone, and in the absence of a response to this treatment, a biopsy is indicated. Despite the fact that stereotactic surgery to obtain a biopsy has important diagnostic value in identifying a pseudotumor lesion, expanding the possibilities of examining these patients makes it possible to avoid it in some cases.
Another atypical symptom of MS, as previously thought, is hearing impairment. During the analysis of cochlear disorders in MS, 70 patients were examined, of whom 35 had complaints of hearing loss; the control group consisted of 18 people.
The clinical features of auditory disorders in MS were a wide range of complaints, which varied from irritation phenomena, such as congestion, tinnitus, hyperacusis, to loss phenomena, up to acute one-sided deafness. A diverse range of auditory complaints was noteworthy: the appearance of hearing disorders on one side or the other, a combination of hearing loss with dizziness, tinnitus, as well as the appearance of hearing disorders at the onset or during exacerbation of the disease. Sometimes patients indicated any hearing impairments only during pointed questioning. A comprehensive audiological examination made it possible to exclude the conductive form of hearing loss in the majority of the examined patients with MS. Thus, according to the results of audiometry, both tonal threshold and in an extended frequency range - high-frequency audiometry, in patients with MS with cochlear complaints on the side of the worse-hearing ear and on the opposite side, as well as in the group of patients without such complaints, an increase in the threshold of sound perception was revealed at all frequencies compared to the control group, however, a more pronounced increase in air conduction thresholds was noted for high frequencies, which is typical for sensorineural hearing loss. In addition, tympanometry, which evaluates the acoustic impedance of the middle ear, obtained results indicating the absence of middle ear pathology and normal functioning of the auditory tube. Finally, with acoustic reflexometry, which is a valuable diagnostic test for the topical diagnosis of hearing disorders (in particular, it makes it possible to distinguish between cochlear and retrocochlear disorders) in MS, a significant increase in the absolute and relative thresholds of the acoustic reflex was recorded, as well as its frequent loss, which is characteristic for retrocochlear lesions. It is important to note that acoustic reflexometry in both patients with complaints of hearing impairment and in patients with MS with dizziness revealed signs of unilateral/bilateral damage to the auditory nerve and auditory centers of the medulla oblongata and pons, which is more typical for patients with cochlear disorders. The data obtained, on the one hand, confirm the sensitivity of acoustic reflexometry in identifying pathology of the auditory nerve in MS, and on the other hand, indicate a high frequency of involvement in the pathological process not only of central structures, but also of retrocochlear neural lesions, even in patients without hearing impairments; At the same time, a significant role of such combined lesions in the development of cochlear disorders in MS is noted. In connection with the presented data, from a practical point of view, it is important to emphasize that when turning to otolaryngologists for patients with complaints of hearing loss when detecting sensorineural hearing loss of unknown origin during differential diagnosis, it is necessary to take into account the possibility of the demyelinating nature of the process, since timely diagnosis of MS and identification of signs of its activity are of fundamental importance for adequate therapy.
In recent years, due to the fairly large selection of drugs that modulate the course of MS and the need for their individual prescription, approaches to the pathogenetic therapy of MS have undergone certain changes. A number of therapeutic algorithms are offered. Escalation (increasing) and induction approaches are discussed: the escalation scheme involves starting treatment with safer drugs and moving on to more aggressive methods if they are ineffective; the induction approach initially implies a more aggressive effect on the immune system, however, the use of this type of therapy may be limited by the possibility of developing a whole range of side effects [17, 24].
One of the groups working in the field of MS treatment, the Multiple Sclerosis Treatment Consensus Group (MSTCG), has proposed an integrated scheme based on the separation of basic and escalation therapy [56]. According to this algorithm, appropriate treatment of an exacerbation is initially necessary, followed by the earliest possible administration of first-line immunomodulators. If disease activity is not effectively controlled, escalation to more intensive therapy is necessary.
Currently, the main first-line drugs include glatiramer acetate and interferons β (IFN β). If treatment is ineffective or poorly tolerated, patients may be transferred from one of these classes of drugs to another or to natalizumab, fingolimod or cladribine. However, under certain circumstances, in particular with an initially highly active course of MS, therapy can be started with one of the last three drugs. According to the MSTCG recommendations, dynamic monitoring of patients is necessary, including both clinical assessment and a number of laboratory and instrumental examinations.
As already mentioned, first-line drugs that modulate the course of MS include IFN β and glatiramer acetate (Copaxone). Currently, the following IFN β drugs are registered in Russia: IFN β-1a for subcutaneous administration (Rebif, Genfaxon); IFN β-1a for intramuscular administration (Avonex, Synnovex); IFN β-1b (betaferon, extavia, ronbetal), which differ in the source of production, chemical structure, as well as in the method and frequency of administration.
The therapeutic effects of IFN β are thought to be related to effects on antigen presentation and inhibition of inflammatory cell proliferation and activation; inhibition of the production of pro-inflammatory cytokines and a change in the cytokine profile towards an anti-inflammatory phenotype; as well as a decrease in the entry of leukocytes into the central nervous system through the blood-brain barrier due to the effect on adhesion molecules, chemokines and matrix metalloproteinases [14, 35, 57]. As a result of the above, damage to the conduction systems of the central nervous system and neurons is reduced. In addition, IFN β induces the synthesis of nerve growth factor by astrocytes [11], and also enhances the secretion of this neurotrophin by endothelial cells during their interaction with T lymphocytes (i.e. at the level of the blood-brain barrier), which also determines its immunomodulatory effect and, possibly, , causes a direct effect on neurons [10].
The mechanisms of action of glatiramer acetate include competitive binding with myelin basic protein to the class II molecule of the major histocompatibility complex involved in the presentation of antigens, as well as activation of the Th2 phenotype of CD4+ T cells that penetrate the blood-brain barrier and secrete anti-inflammatory cytokines (interleukin-4, interleukin-4). 10, interleukin-13, transforming growth factor-β), which leads to suppression of the autoimmune response to multiple myelin antigens [45]. In addition, glatiramer acetate-specific T cells have been shown to express brain-derived neurotrophic factor and transforming growth factor-β [4]. Results obtained in a model of experimental allergic encephalomyelitis suggest that glatiramer acetate promotes neurogenesis [5].
In relapsing-remitting MS, double-blind placebo-controlled trials of betaferon, Rebif, Avonex and Copaxone were conducted, demonstrating their positive effect on the activity of the pathological process, both according to clinical and neuroimaging data [31, 34, 49, 55]. In addition, Rebif and Avonex in relapsing-remitting MS have been shown to slow the progression of neurological deficits on the EDSS scale. When studying the effectiveness of Copaxone and Betaferon, a slowdown in the increase in neurological disorders was also noted, but these changes in these studies were not statistically significant.
In secondary progressive MS, double-blind, placebo-controlled studies of the effectiveness of Rebif and Betaferon were conducted, demonstrating a decrease in the number of exacerbations and a decrease in the severity of immune-inflammatory reactions according to MRI results. Also, when prescribing betaferon, a slowdown in the rate of increase in patient disability (according to the EDSS scale) is shown, regardless of the initial degree of neurological impairment and the presence of exacerbations before or during the study [22]. When treated with Rebif, a lower percentage of patients with progression of symptoms in the presence of exacerbations over the past 2 years was noted (as opposed to patients without exacerbations) [54].
It is important to note that when summarizing the results of long-term immunomodulatory therapy for MS with betaferon, Rebif, Avonex, and Copaxone, data were obtained indicating its effectiveness and safety.
Despite the conflicting data on the role of neutralizing antibodies in IFN β therapy, a decrease in the clinical effectiveness of treatment under their influence cannot be ruled out: a clear negative effect of these antibodies on clinical (frequency of exacerbations) and neuroimaging indicators of MS activity, as well as on the progression of disability, has been shown [25, 29, 53].
In this regard, EFNS guidelines have now been developed for the assessment of antibodies to IFN-β and the clinical application of the measurement of neutralizing antibodies. In particular, tests for neutralizing antibodies should be performed 12 and 24 months after the start of therapy; measurement of neutralizing antibodies should be stopped if they are absent during this period, but studies should be resumed if disease activity increases; if neutralizing antibodies are detected, the study should be repeated after 3-6 months; IFN β therapy should be discontinued in patients with high titers of neutralizing antibodies detected by repeat measurements at 3-6 month intervals [53].
During glatiramer acetate therapy, most patients develop binding antibodies to the drug, which is observed already in the first 3–4 months after the start of treatment [21]. However, these antibodies do not affect the effectiveness of therapy [12].
It is important to note that the frequency of detection of such antibodies differs when treated with different IFN β drugs, in addition, they are characterized by different immunogenicity (titer of neutralizing antibodies produced). According to various researchers, when using Avonex, the lowest incidence of neutralizing antibodies and the lowest immunogenicity were observed compared to other IFN β drugs [28].
It must be emphasized that in recent years a new composition of IFN β-1a (rebif of a new composition) has been developed, the production process of which does not use fetal bovine serum, and the composition does not contain human serum albumin. This formulation improvement resulted in decreased immunogenicity, with the new formulation's Rebif study demonstrating a lower incidence of neutralizing antibodies compared to data from the original formulation. When comparing the safety of the new and original formulations, on the one hand, a slightly higher incidence of influenza-like syndrome was noted, on the other hand, a significant decrease in the frequency of local reactions during treatment with Rebif of the new formulation [26].
In addition, when studying the effectiveness of Rebif of the new composition, a rapidly occurring positive effect was shown in relation to MRI parameters, which reflects the early beneficial effect of the new composition, as well as the original composition, on the activity of the disease [20].
Due to the large selection of first-line drugs that modulate the course of MS, it is quite relevant to compare their clinical effectiveness.
In the course of a comparative analysis of immunomodulatory therapy for MS carried out at the Scientific Center of Neurology of the Russian Academy of Medical Sciences for 3 years of treatment of 400 patients with MS, IFN β-1b (betaferon), IFN β-1a for subcutaneous administration (Rebifom) at a dose of 22 μg or glatiramer acetate showed equally high effectiveness of the studied drugs to reduce the number of exacerbations in both relapsing-remitting and secondary progressive MS. Prevention of the increase in the severity of neurological disorders in relapsing-remitting MS was demonstrated in all three therapeutic groups, and in secondary progressive MS - when prescribing Rebif at a dose of 22 mcg and Copaxone. During glatiramer acetate therapy, a lower incidence of side effects was observed throughout all 3 years of therapy compared with subgroups treated with IFN β [2].
The findings are consistent with the results of recently completed multicenter studies. Thus, when comparing the effectiveness of Rebif and Copaxone in relapsing-remitting MS (REGARD) [41], after 96 weeks of therapy, no differences were found in the primary assessed indicator - the time until the onset of the first exacerbation. Secondary criteria (number and change in volume of active lesions in T2 mode according to MRI, changes in the volume of lesions accumulating contrast agent) also did not differ between the two treatment groups. However, patients treated with IFN β-1a had significantly fewer T1-enhanced lesions and combined unique active lesions compared with patients treated with glatiramer acetate. The small number of exacerbations during the study, in contrast to what was expected, led the authors to speculate that low disease activity in the study population limited the ability to detect clinical superiority of a particular drug. In another study, when analyzing the primary criterion - the risk of exacerbations - over 2 years of therapy, no differences were also found when prescribing betaferon and glatiramer acetate [41].
When discussing issues of therapy that modulates the course of MS, it should be noted that much attention is paid to the early administration of such treatment. Thus, a number of studies have shown the therapeutic effectiveness of betaferon, Rebif, Avonex and glatiramer acetate in CIS [18, 19, 32, 36].
Important from a practical point of view is the possibility of prescribing these drugs in childhood, in connection with which it must be emphasized that in the Russian Federation Rebif is approved for use from 12 years of age, Avonex - from 16 years of age. IFN β-1b drugs (betaferon, extavia, ronbetal) are approved for use with caution in patients under 18 years of age. Glatiramer acetate is approved for use from 18 years of age[].
In 2009, another IFN β-1b, Extavia, was registered and approved for use in Russia, while the active substance of Extavia and Betaferon comes from the same manufacturer, so the drugs are absolutely identical in composition and quality [3]. In the same year, the domestic IFN β - ronbetal was registered, the active substance of which is human recombinant IFN β-1b. The drug is indicated to reduce the frequency and severity of exacerbations in patients with relapsing-remitting MS and to slow the rate of disease progression in patients with secondary progressive MS.
The results obtained during a multicenter prospective randomized comparative clinical trial including patients with relapsing-remitting and secondary progressive (with exacerbations) MS showed comparability of data on the safety and tolerability of the original IFN β-1b drug betaferon and its bioanalogue ronbetal, and also allowed draw a preliminary conclusion about their comparable effectiveness [1]. Thus, over 7.5 months of taking the drugs, the observed adverse events, including deviations in laboratory parameters, in the group receiving ronbetal, corresponded to those for the original drug. The statistically significant difference in the frequency of development of influenza-like syndrome revealed in this study between the groups treated with ronbetal and betaferon (a significantly lower frequency of its development was detected in the group receiving ronbetal) requires clarification in further studies. The obtained data on the reduction in the risk of exacerbations during the use of ronbetal were consistent with the results of multicenter clinical studies on the use of IFN β. During the study, no statistically significant increase in EDSS scores was noted; no differences in average EDSS values between groups were detected either at the beginning of the study or over time. The dynamics of the number and volume of demyelination foci observed in this study according to MRI data during therapy with IFN drugs was similar to the data of international multicenter studies.
In 2010, the following IFN β-1a were registered in Russia: Genfaxon (for subcutaneous use), as well as Synnovex (for intramuscular administration); For patients with relapsing-remitting MS, a number of drugs with other mechanisms of action and routes of administration have been registered: tysabri (natalizumab); Movectro (cladribine); Gilenya (fingolimod).
Natalizumab is a monoclonal antibody and is a selective inhibitor of adhesion molecules. It binds to the α4 subunit of human integrin, which is abundantly expressed on the surface of all leukocytes except neutrophils. In particular, the drug specifically binds to α4β1-integrin, while blocking the interaction with the corresponding receptor, vascular cell adhesion molecule (VCAM-1). In this regard, antibodies to adhesion molecules inhibit one of the main stages of MS pathogenesis – interaction with endothelial cells and migration of lymphocytes across the blood-brain barrier. A further mechanism of action of natalizumab may be due to the cessation of inflammatory reactions in affected tissues by suppressing the interaction of α4-expressing leukocytes with their ligands. Thus, natalizumab can suppress inflammatory activity in affected tissues and further attract immune cells to the site of inflammation. The high efficacy of natalizumab therapy in relapsing-remitting MS has been demonstrated in randomized, placebo-controlled phase III trials. Thus, when using natalizumab in monotherapy, compared with the placebo group, a significant reduction in the average annual frequency of exacerbations, the formation of new or enlargement of existing lesions on T2 MRI and the average number of lesions accumulating contrast agent, as well as a decrease in disease progression were shown [47]. The combination of natalizumab and Avonex was also demonstrated to be significantly more effective than Avonex monotherapy [51].
Currently, the drug tysabri is indicated for monotherapy of relapsing-remitting MS in the following groups of patients: patients with an active course of the disease, despite treatment with IFN β; patients with rapidly progressive severe relapsing-remitting MS. Contraindications to its use are hypersensitivity to natalizumab or any of the excipients; progressive multifocal leukoencephalopathy (PML); increased risk of infection with opportunistic microorganisms, including immunodeficiency states; simultaneous use of IFN β or glatiramer acetate; malignant neoplasms, with the exception of basal cell skin cancer; childhood and adolescence. Natalizumab should not be used during pregnancy unless absolutely necessary; If the patient becomes pregnant while taking Tysabri, therapy should be discontinued; Patients receiving Tysabri should discontinue breast-feeding. The use of tysabri in patients over 65 years of age is not recommended due to the lack of data on its safety in this category of patients. The drug is used as an intravenous infusion once every 4 weeks. When using tysabri, you must be aware of the possibility of developing various side effects. In particular, its use may increase the risk of developing such a dangerous adverse event as PML, and the risk of its development increases with the duration of therapy, especially when treated with the drug for more than 2 years. When prescribing this drug, careful monitoring of patients is necessary, including monitoring of side effects: infections, including PML and infections with opportunistic microorganisms; development of hypersensitivity to drug administration; side effects on liver function, etc. In this regard, special monitoring programs are being developed for individuals receiving tysabri; the drug is prescribed only after appropriate information to the patient, and the doctor and patient should individually consider the balance of benefit and risk when treating with tysabri.
The following two new drugs for the treatment of relapsing-remitting MS, Gilenya (fingolimod) and Movectro (cladribine), are designed to be taken orally. Fingolimod is a sphingosine-1 phosphate receptor modulator. Once phosphorylated, fingolimod acts as a functional antagonist of sphingosine-1 phosphate type 1 receptors, causing their displacement from the outer membrane of lymphocytes to the inner one, which makes T and B lymphocytes unresponsive to signals that stimulate their exit from secondary lymphoid tissue [13, 52 ]. The resulting redistribution of lymphocytes to the lymph nodes and the prevention of their migration from the lymph nodes reduces the flow of autoaggressive lymphocytes into the central nervous system [39, 40, 46]. Due to its lipophilicity, fingolimod penetrates the blood-brain barrier and undergoes phosphorylation in the central nervous system [23]. It has also been shown that fingolimod may have a neuroprotective effect and promotes remyelination in the central nervous system by interacting with sphingosine-1 phosphate receptors on neurons [6, 15, 23, 43].
In two studies conducted, fingolimod was used in two daily doses: 1.25 or 0.5 mg.
One study showed superiority of fingolimod at both doses compared with intramuscular IFN β-1a in terms of efficacy parameters such as exacerbation rates and MRI findings (fewer new or enlarging T2 hyperintense lesions, contrast-enhancing lesions in T1 mode; percentage decrease in brain volume from the initial level). Two fatal infections were reported in the fingolimod 1.25 mg group: disseminated primary varicella zoster
, and encephalitis caused by the herpes simplex virus. Other adverse events in patients receiving fingolimod included nonfatal herpes infections, bradycardia and atrioventricular block, hypertension, macular edema, skin cancer, and elevated liver enzymes [16].
In another study, patients received fingolimod at one of the indicated doses or placebo. The drug in both doses significantly reduced the risk of increasing disability; MRI indicators of disease activity (appearance of new or enlargement of existing lesions in T2 mode, lesions accumulating contrast agent, brain atrophy). Reasons for drug discontinuation and adverse events associated with fingolimod were bradycardia and atrioventricular block at the beginning of treatment, macular edema, elevated liver enzymes and mild arterial hypertension [38].
It should be noted that the registered dose of Gilenya (fingolimod hydrochloride) is 0.5 mg orally once daily; the indication for its use is relapsing-remitting MS to reduce the frequency of clinical exacerbations of the disease and reduce the risk of progression of disability. The drug is contraindicated in case of hypersensitivity to fingolimod or any other component of the drug, pregnancy or during breastfeeding. The effectiveness and safety of Gilenya in children and adolescents under 18 years of age have not been established. There are also a number of conditions for which this drug is prescribed with caution. In this regard, a thorough examination of the patient before prescribing the drug, monitoring the first dose, as well as dynamic monitoring while taking the drug and monitoring for adverse events are necessary.
The mechanism of action of cladribine is associated with the fact that the intracellular accumulation of its active metabolite, 2-chlorodeoxyadenosine triphosphate, leads to disruption of cellular metabolism, inhibition of DNA synthesis and repair, and, accordingly, apoptosis [9]. Cladribine primarily acts on lymphocytes. The accumulation of cladribine nucleotides causes a rapid and long-lasting decrease in the number of CD4+ and CD8+ cells, and also has a rapid but more transient effect on CD19+ B cells with relative sparing of other immune cells [9, 27, 30, 50]. Cladribine also reduces the level of proinflammatory cytokines and chemokines in serum and cerebrospinal fluid, the expression of adhesion molecules, and the migration of mononuclear cells [7, 33, 38, 44].
In a placebo-controlled study, patients with relapsing-remitting MS who received oral cladribine at a dose of 3.5 mg or 5.25 mg per kilogram of body weight showed a significant reduction in the frequency of exacerbations, a higher proportion of patients without exacerbation, and a lower risk of persistent over 3 months of progression of disability, as well as a significant reduction in the number of lesions in the brain according to MRI compared with the placebo group. Adverse events that were more common in the cladribine groups included lymphocytopenia, herpes zoster
[27].
Movectro tablets containing the active substance cladribine (1 tablet – 10.0 mg) are indicated for use in the treatment of relapsing (remitting) MS. Contraindications for prescribing Movectro are hypersensitivity to cladribine and other components of the drug; acute infectious disease or exacerbation of a chronic disease; decreased immunity due to disease or due to the use of immunosuppressants, including cyclosporine, methotrexate, mitoxantrone, natalizumab, or long-term use of glucocorticosteroids; vaccination during the 3 months preceding treatment with an attenuated vaccine (live or attenuated vaccines); pregnancy, lactation period; age under 18 years (insufficient clinical data). Due to the fact that Movectro contains sorbitol, its use is not recommended in patients with fructose intolerance. There are also a number of conditions for which this drug is prescribed with caution.
Movectro therapy is carried out in courses; Each course consists of the use of 1 or 2 tablets during the first 4 or 5 days of a 4-week period (dose calculation is based on the patient's body weight). Treatment with the drug begins with 2 treatment courses, which are called “initial therapy”. The interval between courses of Movectro treatment as part of the “initial therapy” is 4 weeks. 10 months after completion of the “initial therapy”, at the 49th and 53rd weeks, the courses are repeated. These 2 courses are called “re-therapy”. Both before starting therapy and during Movectro therapy, it is necessary to perform certain examinations in order to monitor the patient's condition.
In secondary progressive and relapsing-remitting MS, with rapid progression of the disease and the ineffectiveness of first-line drugs that modify the course of MS, the cytostatic drug mitoxantrone is widely used to reduce the frequency and severity of exacerbations and slow the rate of disease progression. However, when using mitoxantrone, like other cytotoxic drugs, it is necessary to take into account the possibility of side effects, in particular myelosuppression and cardiotoxicity, which requires careful selection of patients and monitoring of relevant indicators. According to the MSTCG publication [56], the maximum cumulative dose is 100 mg/m2 body surface. According to other data, in some cases the total dose should be 80 mg/m2 of body surface. It is recommended that echocardiography be performed before each administration of mitoxantrone. Continuation of the course of the drug is possible only if the patient is sensitive to the treatment and signs of disease activity persist. When prescribing the drug to young women, it is necessary to take into account the possibility of developing prolonged or permanent amenorrhea. In addition, the drug can also affect fertility in men. The use of other immunosuppressants has also been described: azathioprine, cyclophosphamide.
Finally, in some cases, intravenous immunoglobulin is used to reduce the frequency and severity of exacerbations and slow the progression of disability in MS; it has also been shown to reduce the risk of developing a second attack and the appearance of new lesions in patients with CIS when using it.
Thus, in recent years there has been a significant expansion of the range of drugs for the treatment of MS, which is also due to the registration of new drugs with different mechanisms of action. On the one hand, this increases the possibilities of modern therapy that modulates the course of MS, on the other hand, it requires an individual approach to the selection of treatment with a thorough analysis of indications/contraindications and conditions requiring caution, possible side effects; Careful monitoring of the patient's condition during the treatment period is also necessary in order to assess both the effectiveness and safety of the prescribed therapy.
[] www.rlsnet.ru.
Diseases
- 1. General Provisions
1.1.
ANO “MITCLT “Yuninova” offers the Internet user (hereinafter referred to as the “User”) to use its portal “myclinicaltrial.ru” under the conditions set forth in this User Agreement (hereinafter referred to as the “Agreement”). Any development of the portal “myclinicaltrial.ru” is the subject of this Agreement. The Agreement comes into force from the moment the User expresses consent to its terms in the manner provided for in clause 1.2. Agreements. 1.2. By starting to use the portal “myclinicaltrial.ru”/its individual functions, the User is deemed to have accepted the terms of the Agreement in full without any reservations or exceptions. If the User disagrees with any of the provisions of the Agreement, the User does not have the right to use the “myclinicaltrial.ru” portal. If ANO "MITSLT "Yuninova" made any changes to the Agreement in the manner provided for in clause 1.3. Agreements with which the User does not agree, he is obliged to stop using the portal “myclinicaltrial.ru”.
1.3. The use of the portal “myclinicaltrial.ru” is governed by this Agreement. The Agreement may be changed by ANO "MITCLT "Uninova" without any special notice to the user; the new version of the Agreement comes into force from the moment it is posted on the Internet at the address specified in this paragraph, unless otherwise provided by the new version of the Agreement. The current version of the Agreement is located on the page at myclinicaltrial.ru/agreement.
1.4. Any information about clinical trials of a medicinal product for medical use reflected on the portal “myclinicaltrial.ru” does not contain information of an advertising nature.
- 2. User Data
2.1. Using the portal “myclinicaltrial.ru” means the User’s unconditional consent to the automatic transfer by ANO “MICILT “Yuninova”” in the process of using the portal “myclinicaltrial.ru” of cookie data and the provision of ANO “MITCLT “Yuninova” with the IP address, date and time of access to the portal "myclinicaltrial.ru". This consent is given by the User for an indefinite period. This consent may be revoked by the User by sending a corresponding written statement by registered mail with a list of the contents to the address of ANO "MITCLT" Yuninova.
2.2. Cookies, IP address data, dates and times of access to the portal “myclinicaltrial.ru” can be used by ANO “MITCLT “Uninova” for research and statistical purposes, to improve the functioning of the portal “myclinicaltrial.ru”. ANO "MITCLT "Yuninova" has the right to establish that the provision of the portal "myclinicaltrial.ru" is possible only if the User allows the acceptance and receipt of cookies. The structure, content and technical parameters of cookies are set by ANO "MITCLT "Uninova" and may be changed without prior notice to the User.
- 3. Using the portal “myclinicaltrial.ru”
3.1. ANO "MITCLT "Yuninova" has the right to establish restrictions on the use of the portal "myclinicaltrial.ru" for all Users, including the presence/absence of certain functions of the portal, the maximum number of questions that can be sent by the User, the maximum size of the question, the maximum number of requests to the portal “myclinicaltrial.ru”, etc. ANO "MITCLT "Yuninova" has the right to prohibit automatic access to the portal "myclinicaltrial.ru".
3.2. The user is independently responsible to third parties for his actions related to the use of the portal "myclinicaltrial.ru", including if such actions lead to a violation of the rights and legitimate interests of third parties, as well as for compliance with the law when using the portal "myclinicaltrial.ru" "
3.3. When using the portal “myclinicaltrial.ru”, the User does not have the right to upload, send, transmit or in any other way post and/or distribute illegal content; violate the rights of third parties and otherwise violate the law, including international law.
3.4. All objects available through the portal "myclinicaltrial.ru", including design elements, text, graphics, illustrations, videos, computer programs, databases, music, sounds and other objects of intellectual activity, as well as any other content, posted on the portal “myclinicaltrial.ru”, are the objects of the exclusive rights of ANO “MITCLT “Yuninova”, Users and other rights holders. The use of content elements and content of the portal "myclinicaltrial.ru" is possible only within the framework of the functionality offered by the portal "myclinicaltrial.ru". No elements of the content of the portal "myclinicaltrial.ru", as well as any content posted on the portal "myclinicaltrial.ru", can be used in any other way without the prior permission of the copyright holder.
3.5. The portal "myclinicaltrial.ru" may contain links to other sites on the Internet (third party sites). These third parties and their content are not verified by ANO “MITCLT “Uninova” for compliance with any legal requirements. ANO "MITCLT "Yuninova" is not responsible for any information, materials posted on third party sites that the User accesses using the portal "myclinicaltrial.ru", for the availability of such sites or content and the consequences of their use by the User. A link to any site, product, service, or any information of a third party posted on the portal “myclinicaltrial.ru” does not constitute an approval or recommendation of the specified site, product, service, or information by ANO “MITCLT “Uninova”.
- 4. User Content
4.1. The User is solely responsible for compliance of the content posted by the User with the requirements of current legislation, including liability to third parties in cases where the User’s placement of certain content or the content of the content violates the rights and legitimate interests of third parties, including personal non-property rights of authors, other intellectual property rights the rights of third parties, and/or infringes on the intangible benefits belonging to them.
4.2. The User acknowledges and agrees that the ANO "MITCLT "Yuninova" is not obliged to view content of any kind posted and/or distributed by the User through the portal "myclinicaltrial.ru", and also that the ANO "MITSLT "Yuninova" has the right, in its own right, discretion to refuse the User to post and/or distribute content or to delete any content that is available through the portal “myclinicaltrial.ru”. The User acknowledges and agrees that he must independently evaluate all risks associated with the use of the content, including assessing the reliability, completeness or usefulness of this content.
4.3. The User understands and agrees that the technology of operation of the portal “myclinicaltrial.ru” may require copying (reproduction) of the User’s content of ANO “MITCLT “Yuninova”, as well as processing of it by ANO “MITCLT “Yuninova” to meet the technical requirements of the portal “myclinicaltrial.ru” "
- 5. Other provisions
5.1. The user uses the portal “myclinicaltrial.ru” at his own risk, the portal “myclinicaltrial.ru” is provided “as is”. ANO "MITCLT "Yuninova" does not guarantee that the portal "myclinicaltrial.ru" meets the User's requirements; the portal “myclinicaltrial.ru” will be provided continuously, quickly, reliably and without errors; the results that may be obtained using the portal "myclinicaltrial.ru" will be accurate and reliable and can be used for any purpose or in any capacity; the quality of any product, service, information, etc. obtained using the portal “myclinicaltrial.ru” will meet the User’s expectations.
5.2. The User may use any information and/or materials that the User accesses using the portal “myclinicaltrial.ru” at his own peril and risk and is solely responsible for the possible consequences of using this information and/or materials.
5.3. ANO "MITCLT "Yuninova" is not responsible for any types of losses that occur as a result of the User's use of the portal "myclinicaltrial.ru" or individual functions of the portal "myclinicaltrial.ru". Under any circumstances, the liability of ANO "MITSLT "Yuninova" in accordance with Art. 15 of the Civil Code of the Russian Federation is limited to 10,000 (ten thousand) rubles.
5.4. The Agreement constitutes an agreement between the User and ANO "MICILT "Yuninova" regarding the procedure for using the portal "myclinicaltrial.ru" and replaces all previous agreements between the User and ANO "MICILT "Yuninova".
5.5. The Agreement is governed by and construed in accordance with the laws of the Russian Federation. Issues not regulated by the Agreement shall be resolved in accordance with the legislation of the Russian Federation. All possible disputes arising from the relations governed by this Agreement are resolved in the manner established by the current legislation of the Russian Federation. Throughout this Agreement, unless explicitly stated otherwise, the term “legislation” means both the legislation of the Russian Federation and the legislation of the User’s place of residence.
5.6. If for one reason or another one or more provisions of this Agreement are found to be invalid or unenforceable, this will not affect the validity or enforceability of the remaining provisions of the Agreement.
5.7. Inaction on the part of ANO "MITCLT "Yuninova" in the event of a violation by the User of the provisions of the Agreements does not deprive ANO "MITSLT "Yuninova" of the right to take appropriate actions to protect its interests later, and also does not mean a waiver of ANO "MITSLT "Yuninova" from its rights in the event of a violation in the future similar or similar violations.