In recent years, the problem of pregnancy management in multiple sclerosis (MS) has received increasing attention. This is due to several reasons. Firstly, the disease itself, MS, is of great medical and social importance, since it often develops in people of young working age and can quickly lead to disability. Secondly, this disease predominantly affects people of childbearing age, with women much more likely (2-4 times) than men. Thirdly, questions of planning, tactics for managing pregnancy, childbirth and the postpartum period, the possibility of breastfeeding with MS, the likelihood of developing this disease in children are quite reasonably asked by patients in each case. Fourthly, improving diagnostic capabilities and expanding the range of therapeutic approaches (primarily the widely used various drugs that modify the course of MS - DMTs, as well as symptomatic drugs) require constant improvement of knowledge by practicing neurologists. It is important for doctors to be informed about the possibility of prescribing certain diagnostic procedures and medications before, during pregnancy and after childbirth to ensure competent, most effective treatment of patients and at the same time safe management of pregnancy for the mother and child. Finally, fifthly, a comprehensive study of the role of hormonal factors and the causes of changes in the course of the disease during pregnancy can serve to clarify the pathogenetic mechanisms of MS and develop new therapeutic approaches.
This review summarizes data from recent publications concerning the most frequently asked questions regarding pregnancy in MS.
So, at the stage of pregnancy planning
key questions relate to the impact of MS on fertility;
risk of developing MS in children; influence of pregnancy on the course of MS. It is the neurological symptoms of MS that can interfere with the care of a child, his upbringing, concern about burdening a spouse, the possibility of developing MS in children, as has been shown by a number of researchers, that are among the main reasons associated with MS, on the basis of which doubts about childbearing arise [9] . At the stage of pregnancy,
the main problems relate to the possibility of using certain pharmacological drugs, monitoring the course of the disease, as well as labor management tactics.
Finally, in the postpartum period,
questions about breastfeeding, including in relation to the prescription of pathogenetic drugs, require solutions.
The impact of MS on fertility, the use of assisted reproductive technologies
To date, no comprehensive research has been carried out on this issue. According to some authors, epidemiological data suggest that spontaneous fertility may be reduced, since a number of endocrine and sexual disorders can potentially affect reproductive function in patients of both sexes [15]. Other data suggest that fertility does not appear to be significantly affected in patients with MS. However, infertility and MS can occur simultaneously [37].
In this situation, assisted reproductive technologies can be used. However, similar technologies using gonadotropin-releasing hormone (both agonists and antagonists) and gonadotropins can increase both the clinical activity of MS and the activity of demyelination foci according to MRI [18, 40]. Also, an increase in the frequency of exacerbations was noted within 3 months after in vitro fertilization (IVF) compared to the same period 1 year before the procedure [49]. According to the authors, a significant increase in MS activity occurs both with the use of gonadotropin-releasing hormone agonists and in cases where the IVF procedure is not accompanied by pregnancy. Possible mechanisms for such deterioration may include hormone-induced immunological changes: proliferation of immune cells with increased production of cytokines and endothelial growth factor; rapid phase changes in estrogen levels under the influence of gonadotropin-releasing hormone agonists; a break in taking DMTs, as well as a stressful situation due to infertility [37, 50].
Of course, further research is needed to understand this phenomenon, but already at this stage, such information should be provided to interested parties in the case of planning the use of assisted reproductive technologies in order to make an informed decision [50].
Risk of developing MS in children (familial incidence)
To date, evidence from numerous population-based, genealogical and twin studies indicates a hereditary predisposition to MS. Thus, if one of the parents has MS and there were no other patients in the family, then the risk of developing MS in a child throughout life is 3-5% [62]. Moreover, these figures are approximately equal to the average population risk of any other birth defect being detected in a child [25]. If both parents have MS, then the risk of developing MS in a child throughout life is, according to various authors, from 6 [59] to 30% [26]. If both parents are healthy, but the marriage is consanguineous, and one of the relatives had MS, then the risk of developing MS in a child can reach 9% [62].
It should be noted that the observed type of inheritance in MS is characteristic of polygenic diseases that arise as a result of the joint contribution of many independently acting or interacting polymorphic genes [12]. Perhaps further work to identify genetic markers of MS in the future will make it possible to more accurately determine the individual risk of developing the disease in children whose parents suffer from MS, and to individualize their treatment.
Psychological characteristics of pregnant women suffering from multiple sclerosis
According to statistics, the majority of women suffering from multiple sclerosis are of reproductive age. Because of this, the issue of pregnancy with this disease is very acute.
In the middle of the last century, pregnant women suffering from this disease were sent straight to have an abortion. Nowadays, scientists specializing in medical issues have conducted a number of studies and come to the conclusion: multiple sclerosis and pregnancy do not pose a threat to a woman and her unborn baby.
In some cases, they even recommend that people with MS get pregnant, since the psychological component of the issue plays an important role. But for this you need to undergo a full examination by doctors and receive competent advice from a neurologist.
Doctors who do not have full information about modern research will be against conception and may even dissuade a woman from becoming pregnant. A woman needs to be prepared for criticism and condemnation in her address and remember: a contraindication to conceiving, bearing and giving birth to a child is only a very severe form of multiple sclerosis, in which the patient is practically bedridden and is unable to move independently.
The course of MS is worse during nervous disorders and stress than during pregnancy. If a woman has the desire and ability to give birth to a child, she should be given such a chance, but if she is dissuaded from this or condemned for planning this step, then this will lead to depression of her nervous state and a worsening of the course of multiple sclerosis. And if a woman has an abortion under pressure from public opinion, then this is a double blow - to the mental and physical state of the patient. After all, abortion causes both psychological harm and causes hormonal changes, which, however, are not irreversible.
Patients with multiple sclerosis are afraid that their child will inherit the disease. But do not be afraid of this: according to statistics, only three percent of children are susceptible to this disease if one of the parents suffers from this disease. The official opinion of scientists and doctors: multiple sclerosis is not inherited!
The effect of pregnancy on the frequency of MS exacerbations
The fact that the frequency of exacerbations during pregnancy decreases is well known. Thus, during pregnancy in women with MS, the number of exacerbations decreases by approximately half, especially in the third trimester, and, conversely, increases in the first 3-6 months after birth [17, 50]. According to the PRIMS (Pregnancy In Multiple Sclerosis) prospective study, which included 227 patients with MS, the rate of exacerbations before delivery was 0.7 (95% CI 0.6-0.8); in the first trimester of pregnancy - 0.5 (95% CI 0.4-0.6), in the second - 0.6 (95% CI 0.5-0.7), in the third - 0.2 (95% CI 0.2-0.3); in the first trimester after childbirth - 1.2 (95% CI 1.1-1.4), followed by a gradual decrease, while already 3 months after birth there were no significant differences in the frequency of exacerbations with the prenatal period [72]. Despite the increased risk of exacerbations in the first 3 months after birth, 72% of patients did not experience exacerbation of the disease during this period. Three parameters (increased number of exacerbations in the 1 year before pregnancy, increased number of exacerbations during pregnancy, and higher EDSS score at the time of pregnancy) were correlated with the onset of exacerbation in the postpartum period.
How to increase the chances of a normal pregnancy
Pregnant women are monitored according to MS guidelines. In addition to standard blood tests and combined screening in the 1st trimester, determination of thyroid hormones (TSH, free T4, anti-TPO) is recommended at the 6th week. In case of abnormal results, the woman is referred to an endocrinologist to adjust treatment.
A pregnant woman should regularly visit a gynecologist, who will ask a neurologist to assess the course of multiple sclerosis and recommendations on how to act during pregnancy, childbirth, and the postpartum period.
- is required every 3 months or as needed.
- From conception to birth, the woman is prescribed a low maintenance dose of corticoids (Prednisone, Medrol). As a result of the use of which, thickening of the fetal heart septum may be observed, visible on ultrasound (at the 20th week). This is not a serious heart defect and the condition usually returns to normal.
- Each attack is treated with corticosteroids , the therapeutic dose is selected so as not to endanger the fetus.
- It is recommended to eat natural food, plenty of vegetables, fruits, fish, take magnesium supplements, vitamin B6 (pyridoxine), which suppress muscle spasms and spasticity.
- It is advisable to use multivitamin preparations (eg, Pregnavit). But their uncontrolled use increases the risk of increased fetal growth, which can cause various complications during childbirth.
- Adequate rest, quality sleep, and stress reduction are recommended .
- Moderate physical activity is important to improve physical fitness and prepare for childbirth (walking, water exercises, swimming).
At the end of the 3rd trimester, you may experience a frequent urge to urinate due to the baby's pressure on the bladder. Usually this is not directly related to the disease. But if you consider that fecal and urinary incontinence is one of the symptoms of MS, it is worth undergoing additional examination.
Throughout the entire period, the woman usually feels well. Her immune system is artificially suppressed so as not to harm the fetus, which reduces the manifestation of the disease.
Seizures before childbirth are rare. They may occur in women previously treated with first-choice drugs: β-interferon, glatiramer acetate.
The influence of pregnancy on the course of MS and disability
According to a number of authors, a decrease in the risk of developing MS in women who have given birth has been shown compared to nulliparous women [61], which is consistent with the results of A. Ponsonby et al., according to which pregnancy can have a protective effect on the risk of developing the first demyelinating episode [57].
In the case of an established diagnosis of MS, data on the effect of pregnancy on the course of the disease are sparse and ambiguous. According to some data, the risk of progressive disease is significantly lower in women who gave birth after the onset of MS [5, 61]. Other researchers, when analyzing childbirth and secondary progression, did not find their connection [45].
According to S. Ramagopalan et al., pregnancy does not have any delayed effect on disability [58]. On the contrary, M. D'hooghe et al. do not exclude the possibility of a beneficial long-term effect of childbirth on the course of MS [22]. According to B. Weinshenker et al., no associations were identified between disability and the total number of pregnancies, as well as the timing of pregnancy relative to the onset of MS [75]. At the same time, according to P. Verdu et al., the time before the need to use a wheelchair is approximately 50% longer in women who have had at least 1 pregnancy after the development of the disease, compared with non-pregnant patients [70].
Thus, there is currently no clear reliable data on the effect of pregnancy on the course of MS. However, this aspect, according to a number of authors, has a small impact on family planning [50].
Procedure for treating MS
People suffering from MS are prescribed various medications that modify the course of the disease. During an exacerbation of the disease, the patient undergoes a course of hormonal therapy, which affects the foci of inflammation in the body, thereby suppressing them.
After a course of hormonal therapy, a patient with multiple sclerosis is prescribed drugs that block the development of repeated exacerbation - these are the so-called beta-interferons.
Several years ago, drugs were invented in Russia whose monoclonal antibodies attach to aggressive immune cells, thereby blocking their destructive effect. After this, healthy immune cells neutralize them.
Mechanisms of natural immunosuppression during pregnancy in MS
Endocrine immunoregulation during pregnancy
Previous concepts largely attributed the positive effect of pregnancy on MS activity to increased blood levels of circulating hormones such as estrogen, progesterone, or glucocorticoids. These hormones have powerful immunomodulatory properties, including changes in the production of cytokines, suppression of the expression of adhesion molecules and matrix metalloproteinases, reduction in the presentation of antigens, and the migratory ability of T cells [60, 71]. Most of these hormones peak in the third trimester of pregnancy, which coincides with the maximum decrease in MS activity. However, despite the obvious regulatory role of sex hormones in MS, the lack of correlations with the level of at least one specific hormone allows us to make only assumptions regarding the underlying mechanisms [21].
To date, in order to explain the mechanism of remission that occurs during pregnancy in women with MS, there is a theory based on the supposed shift of the pro-inflammatory Th1 response towards the anti-inflammatory Th2 response in the peripheral blood [8, 34, 47]. However, this paradigm is overly simplistic and does not reflect the complex immunomodulation that occurs in the mother and the mother-placenta-fetus system [16, 66]. It is likely that immunomodulatory mechanisms in MS during pregnancy go beyond the anti-inflammatory Th2 effect.
Currently, much attention is paid to regulatory T cells (Treg) and natural killer (NK) cells, as these cells are believed to be responsible for the development of immunosuppression during pregnancy [55]. Moreover, the role of Tregs in the pathogenesis of MS is currently being actively studied [2].
In the decidua during the first trimester of pregnancy, the most abundant immune cells are dNK (decidua natural killer cells) [43, 52]. Compared to peripheral NKs, dNKs are characterized as CD56 bright CD16-CD3- and have low cytotoxic properties [43, 52]. CD56bright CD16- CD3- originate from CD34+ already present in decidual tissue, rather than migrating here from the periphery. dNK secrete cytokines and chemokines (IL8, VEGF, SDF-1, IT-10), which control the process of blastocyst implantation, growth, development and permeability of the trophoblast, neoangiogenesis and placental remodeling [64]. It has been established that in patients with MS, the number of dNK increases by the third trimester of pregnancy compared to the postpartum period, while the total number of peripheral cytotoxic CD56dim (CD3-CD56dimCD16+) decreases [7].
Also, during the first trimester, a local increase in the number of Tregs (CD4+CD25+Foxp+) and a low content of Th17 cells is observed in the decidua [51, 63]. Normally, Tregs have the ability to suppress autoantigen-specific proliferation and effector functions of autoreactive lymphocytes [19]. During pregnancy, they play a key role in the formation of immune tolerance to the fetus. CD4+CD25+Foxp+ ensure blastocyst implantation into decidual tissue and fetal survival in the uterus. Tregs act by suppressing the proliferation and cytokine production of CD4+ and CD8+ cells, cytotoxic NK, B cells and immunoglobulins [48, 56] and inhibit the activity of dendritic cells and macrophages. Studies in mice have shown that in the blood, lymph nodes and thymus, an increase in Tregs occurs as early as day 2 of pregnancy, followed by a gradual decrease starting in mid-pregnancy [68, 76]. A trend towards an increase in circulating Tregs in early pregnancy, reaching a maximum in the second trimester and their gradual decrease in the postpartum period, is also observed in humans [68].
Thus, both hormonal and immunological changes in the maternal-fetal-placental axis likely contribute to immunosuppression during MS pregnancy. However, of course, these mechanisms have not been sufficiently studied to date.
Are there risks of developing MS while pregnant?
The pregnancy period is considered favorable for the development of autoimmune diseases, which include multiple sclerosis.
In an autoimmune disease, the cells responsible for the immune system attack the body for some reason. But during pregnancy their activity weakens. The fetus is a foreign body in the mother's body, so the immune system “switches” to its presence, leaving other autoimmune reactions unattended.
It is known that the disease can first appear after childbirth, with significant fluctuations in hormone levels. But healthy women do not need to be afraid of pregnancy and childbirth as a cause of illness.
If there is a predisposition, the disease may occur due to stress or another disorder, such as a severe viral infection.
On the contrary, in March 2008, Australian scientists released the results of a study according to which women who have given birth are much less likely to develop this autoimmune disorder.
Relieving exacerbations of MS during pregnancy
It is well known that glucocorticosteroids cross the placenta and can affect the fetus. In experimental studies conducted on animals, it was found that corticosteroid hormones lead to intrauterine death with fetal resorption, miscarriages, non-viability of newborns, deformities and growth deficiency [20, 24]. In this case, developmental disorders are more pronounced the shorter the gestational age and the greater the dose of administered hormones [53]. There is evidence indicating an increased risk of placental insufficiency, malnutrition at birth, decreased height and weight, and sometimes fetal death in women with long-term use of corticosteroid hormones during pregnancy [32, 46]. Their use is especially dangerous in the first trimester. In the case of their short-term exposure during the second and third trimesters of pregnancy, no negative effect on the human fetus was detected [32, 46]. Thus, in women at risk of developing premature birth, who are administered dexamethasone in the third trimester in order to stimulate lung maturation in the fetus, healthy children are born, with normal weight and body length. A general blood test of infants reveals leukocytosis, which persists for a short time [28]. The use of methylprednisolone in the first trimester of pregnancy is also unsafe: there are reports of the possible development of immunosuppression in newborns [28]. Since methylprednisolone is metabolized before passing through the placental barrier, its use is preferable to dexamethasone if it is necessary to prescribe glucocorticosteroids during pregnancy.
In general, the main publications of recent years discuss the possibility of using short courses of methylprednisolone in the second and third trimesters of pregnancy in cases of severe exacerbations of MS [28, 32].
According to a therapeutic opinion published in 2014 by experts in the field of MS, the use of intravenous methylprednisolone to treat exacerbations of the disease during pregnancy is associated with potential risks to the fetus and the development of side effects for the mother; It is best to avoid its use, especially in the first trimester of pregnancy, and limit its use during pregnancy to only those exacerbations that have a significant impact on the patient’s daily activities [50].
If pregnancy with multiple sclerosis occurs without preparation
If pregnancy has already taken place without preparation, all that remains is to accept it as a fact.
MRI is not recommended during pregnancy. We will conduct an examination for infections and immune status, and we will monitor the activity of multiple sclerosis using blood tests, electromyography and evoked potential studies.
Taking DMTs when planning and during pregnancy
The currently fairly large selection of DMTs implies the need for their individual prescription, and various treatment regimens are being discussed [3]. When using DMTs at the stage of pregnancy planning, an individual approach is also, of course, necessary. There is a tactic for canceling DMTs when planning pregnancy in advance. Another opinion has been expressed - about the advisability of canceling DMTs not before, but after the onset of pregnancy, which makes it possible to control the disease [4]. In general, it is best to discontinue the use of both DMTs and symptomatic therapy, both during the planning stage (if possible) and during pregnancy, unless the benefit-to-risk ratio favors continued treatment [50]. To date, certain data have already been accumulated on the use of both first and second line DMTs during pregnancy.
Interferon-β (IFN-β)
Animal studies of IFN-β have reported higher rates of spontaneous abortion [28]. However, in these studies, the dose of IFN-β administered was 3-5 times higher than the recommended weekly dose for humans (while 2 times the excess did not contribute to spontaneous miscarriage) [14, 41].
At the same time, recent prospective studies published from 2005 to 2013 showed that after exposure to IFN-β up to 45 days of gestation, the percentage of pregnancies ending in spontaneous abortion corresponded to the percentage in the general population [65]. Also, no association was found between IFN-β use and the incidence of congenital anomalies [13, 14, 23, 65, 69]. However, a number of authors describe cases in which a decrease in body weight and a decrease in fetal length at birth was observed [10, 30, 73]. This is believed to be related to the mechanism of action of this drug. Although IFN-β is a macromolecule [54] that cannot cross the fetoplacental barrier [54], it can indirectly stimulate the production of maternal cytokines, which freely cross the placenta and affect the fetus [54].
A course of IFN-β is not started during pregnancy. If the patient is already receiving drugs from this group, standard practice is to stop the course before the planned pregnancy. It is also possible to continue treatment immediately until pregnancy occurs if it is necessary to avoid a gap between cessation of therapy and the onset of pregnancy [50].
Glatiramer acetate (GA)
Recent studies have shown that after exposure to GA before 6 weeks of gestation, no significant association was found between its use and an increased risk of spontaneous abortion [31, 33, 73]. The risk of spontaneous abortion was comparable to that in the general population [31, 33, 73]. When prescribing GA, there was no significant reduction in body weight or reduction in fetal length at birth [33, 73]. Also, no anomalies or developmental delays were observed in children during a follow-up period of up to 2.1 years [33]. The low risk of teratogenic effects of GA on the fetus is associated with its mechanism of action - like IFN-β, it is a macromolecule [54] that does not penetrate the fetoplacental barrier, and, unlike the latter, does not contribute to the launch of the production of maternal cytokines.
According to the therapeutic opinion of experts in the field of MS published in 2014, the following provisions have been adopted regarding the use of IFN-β and GA during pregnancy in MS.
Sufficient experience has been accumulated, but the number of published data on the effects of IFN-β and GA on pregnancy is limited. Most likely, there is no increase in the risk of spontaneous abortion. Subcutaneous administration of IFN-β does not currently suggest a precise effect on the development of fetal anomalies, but published information on IFN-β for intramuscular administration and GA is more limited on this issue. Overall, the available data are not sufficient to rule out rare adverse effects on the fetus. It is standard practice to discontinue therapy with these drugs before and during pregnancy unless there is a significant risk to the pregnant woman of increased MS activity without appropriate therapy and the benefits of treatment outweigh the potential (albeit uncertain) risks to the fetus.
Natalizumab
Animal experiments have shown that natalizumab penetrates the fetoplacental barrier, which leads to a decrease in the number of platelets and decreased survival of offspring [74].
There have been no large studies in pregnant women. However, in 2013, an article was published reporting on two newborns whose mothers were treated with natalizumab (a total course of 1200 mg) due to severe neurological deficits between 21 and 34 weeks of gestation [67]. . In both cases, live, full-term children were born, with normal weight and body length. At the age of 12 weeks, psychomotor and somatic development corresponded to the age norm. An ultrasound examination of the brain did not reveal any pathology. However, in the immunogram, as at birth, there was an increase in the number of B-lymphocytes and the CD4/CD8 immunoregulatory index compared to healthy children.
A therapeutic opinion from MS experts published in 2014 recommends discontinuation of natalizumab therapy during pregnancy, but the decision should be made on a case-by-case basis based on benefit and risk, bearing in mind the possibility of relapse into highly active MS after discontinuation of therapy.
Fingolimod
When using the drug in experimental studies, reproductive toxicity was identified, including fetal death and organ malformations, mainly patent ductus arteriosus and ventricular septal defects [44]. To date, recommendations have been published, according to which pregnancy should be avoided until the drug is removed from the body - about 2 months after stopping treatment [27, 50].
Intravenous immunoglobulins (IVIG)
In relapsing-remitting MS, a reduction in the frequency of exacerbations has been described when IVIG is prescribed during pregnancy and after childbirth without serious side effects in newborns [6]. Another study of two doses of IVIG in the postnatal period showed a positive therapeutic effect without increasing the risk of exacerbations [35].
According to a therapeutic opinion from MS experts published in 2014, although the use of IVIG is probably safe, it is not currently recommended due to insufficient evidence of effectiveness.
Mitoxantrone
First of all, when prescribing mitoxantrone, it is necessary to take into account the possibility of developing amenorrhea. In addition, mitoxantrone has also been shown to contribute to the development of premature birth in animals, and also leads to retardation of fetal growth and development. Spontaneous abortion and fetal growth restriction have also been observed in women who were given mitoxantrone during pregnancy for the treatment of breast cancer. The drug is not prescribed during pregnancy, given the potential teratogenic effect.
Regarding the effect of DMTs on fertility in men and the pregnancy of the spouse of a patient suffering from MS, at the moment there is very little information on this issue. One study compared pregnancy outcomes from paternal treatment (mainly IFN-β or GA) with outcomes from a maternal cohort with or without DMT. At the same time, the average body weight of newborns from fathers suffering from MS did not differ from the control group. Despite the small number of observations, the data obtained, according to the authors, suggest safe parenthood for patients suffering from MS [38]. Although some men stop treatment with GA or IFN-β before their spouse becomes pregnant, there is limited justification for this approach [50].
Multiple sclerosis, pregnancy and childbirth
Multiple sclerosis (MS) is a fairly widespread dysimmune disease of the central nervous system, which affects mainly young people and almost inevitably leads, at a certain stage of its development, to disability. This disease is chronic, in most cases progressive, unpredictable in course and currently incurable. In recent years, there has been an increase in MS incidence rates, which is associated not only with improvements in diagnostic methods, but also with an absolute increase in the number of cases. The age range of this disease is also expanding (usually 20–40, but cases of onset of the disease at the age of 10 to 55 years have been described). The exclusion of a large number of able-bodied people from active life due to disability, high costs for diagnosis, treatment, rehabilitation and social assistance make the problem of MS socially and economically significant.
The significant and uneven prevalence of the disease on Earth is noteworthy. High-risk areas for MS incidence (more than 100 patients per 100,000 inhabitants) are the Scandinavian countries and Central European countries, Canada. In Russia, southern European countries, Australia and the USA, this disease occurs with a frequency of 30 to 100 cases per 100,000 inhabitants. Women get sick more often than men, representatives of the white race more often than blacks.
The study of MS dates back more than 100 years, and although significant strides have been made in understanding the disease in recent years, many unresolved questions remain. In recent years, the understanding of the very essence of MS has changed as a disease that affects only the myelin sheaths of the conductors of the brain and spinal cord, in which periods of exacerbations are replaced by periods of complete or almost complete clinical well-being. It is now known that already in the early stages of the disease there is damage to the axons themselves, leading to brain atrophy, and therefore it is proposed to consider MS as an autoimmune neurodegenerative, and not just a demyelinating disease. It has been reliably proven that even in the phase of complete clinical remission, the activity of the disease remains, and this is confirmed by the appearance of new foci of demyelination (according to magnetic resonance imaging) and ongoing disorders in the immune system. Thus, MS is not in the full sense of the word a “remitting” disease.
Until recently, the timing of establishing the correct diagnosis of MS in the development of neurological symptoms was not particularly important, since the doctor could not influence the development of the disease to any extent. Treatment of patients consisted only of stopping exacerbations and providing symptomatic therapy. In recent years, the situation has changed radically due to the advent of so-called preventive, or modifying, therapy. These drugs, although they are not able to cure the patient, significantly change the course of MS in many patients, preventing the development of exacerbations and slowing down the development of disability. The activity of research devoted to the morphology, etiology and pathogenesis of MS, and, as a consequence, the development of new therapeutic approaches to its treatment, gives reason to believe that in the not too distant future it will be possible to find methods for secondary clinical prevention and pathogenetic radical treatment of MS.
Multiple sclerosis and pregnancy:
It has long been well known that pregnancy has a beneficial effect on the course of MS—during it, exacerbations of the disease become less frequent.
The reason for this is considered to be hormonal changes during pregnancy, which is accompanied by immunosuppression. However, in the first 3 months. after childbirth, on the contrary, the disease may take on a more aggressive course - exacerbations become more frequent and more severe. This is why women with MS were previously strongly discouraged from having children. Recently, this view has been revised. Long-term observation over a number of years of a large number of sick women before pregnancy and after childbirth turned out that, although in the first months after childbirth the frequency of exacerbations does increase somewhat (the risk of exacerbation in the first 3–6 months after childbirth is 20– 40%), balancing their decrease in the prenatal period, the birth of a child does not affect the long-term prognosis of the disease. Moreover, one study over a 25-year period showed that women who had children during this period later experienced secondary disease progression (compared to nulliparous patients) and were less disabled.
Thus, it was found that pregnancy and childbirth are not a risk factor for exacerbations of MS, and it is even possible that pregnancy has a beneficial effect on the course of the disease. Exacerbations that occur in the first months after childbirth are probably provoked not by hormonal changes, as previously thought, but by the stress of childbirth and significantly increased physical activity after the birth of a child. Women should not be scared of pregnancy. A more significant activation of the disease than childbirth is caused by termination of pregnancy (both artificial and spontaneous) and hysterectomy.
During pregnancy, drug treatment should be avoided if possible. The use of adrenocorticotropic hormone and its synthetic analogs is contraindicated, since these drugs suppress the adrenal glands of the fetus. In case of severe exacerbation in the second and third trimester of pregnancy, the use of prednisolone is allowed.
There are descriptions of the use, even in the early stages of pregnancy, of hormonal “pulse therapy” with methylprednisolone, plasmapheresis and intravenous immunoglobulin to relieve severe exacerbations, with the subsequent birth of healthy children.
During pregnancy and breastfeeding, you should not take drugs that can pass through the placenta or through mother's milk into the baby's body. Such drugs, often used for MS, include: diphenine, carbamazepine, baclofen, azathioprine, cyclophosphamide.
If pregnancy occurs in a patient with MS receiving preventive therapy with beta-interferons or Copaxone, such treatment should be discontinued until the baby is born and breastfeeding is complete. However, there are isolated observations that describe cases of continued treatment with preventive therapy drugs during pregnancy. In all cases, healthy children were born, and monitoring them until the age of 3 did not reveal any deviations from the norm. And yet, during pregnancy and lactation, treatment with modifying drugs should not be continued. After completing the breastfeeding period, it is advisable to start or resume preventive therapy as soon as possible in order to avoid a possible exacerbation. If the patient received mitoxantrone, then a break of 6 months is desirable. before pregnancy (although there is evidence of the birth of healthy children in women who received mitoxantrone at the time of conception).
During pregnancy, a woman should not take benzodiazepines, as they act on the fetus, leading to the development of “floppy baby” syndrome.
The recommended drug for the development of urinary infection during pregnancy is ampicillin. For those patients who have already had episodes of urinary tract infections, its prophylactic use is indicated, since the development of pyelonephritis is very likely.
Methods of delivery for multiple sclerosis:
Depending on the duration of the disease and the existing neurological disorders, childbirth in MS is carried out either naturally or surgically. In general, pregnant women with MS undergo operative delivery approximately 1.5 times more often than other pregnant women.
Childbirth anesthesia in pregnant women with MS:
In standard situations, a cesarean section is performed under one of the types of neuraxial anesthesia (spinal or epidural anesthesia). Previously, it was believed that multiple sclerosis is a contraindication to surgery under neuraxial anesthesia, since it involves the administration of drugs (local anesthetics) directly into the spinal cord, which is part of the nervous system. However, studies in recent years have shown that patients with multiple sclerosis tolerate all types of anesthesia and anesthesia equally well. It has been proven that patients with multiple sclerosis have the same risk of anesthesia complications as relatively healthy people.
When it comes to vaginal birth, research clearly demonstrates that epidural pain relief for labor does not increase the risk of an MS attack in the postpartum period. That is, in pregnant women with multiple sclerosis, epidural anesthesia can quite reasonably be used to relieve pain during natural childbirth, especially since severe pain, which is a constant companion to childbirth, is a proven risk factor for exacerbation of the disease.
In standard situations, a cesarean section is performed under one of the types of neuraxial anesthesia (spinal or epidural anesthesia). Previously, it was believed that MS is a contraindication to surgery under neuraxial anesthesia, since its implementation involves the administration of drugs (local anesthetics) directly into the spinal cord, which is part of the nervous system. However, studies in recent years have shown that patients with MS tolerate all types of anesthesia and anesthesia equally well. It has been proven that patients with MS have the same risk of anesthesia complications as relatively healthy people.
Thus, depending on their health status, pregnant women with MS can equally safely give birth either independently or through a caesarean section. Vaginal childbirth in patients with multiple sclerosis is best performed under epidural anesthesia. The choice of anesthesia for caesarean section is based on generally accepted principles and does not have any fundamental features.
Protective effect of breastfeeding in MS:
Researchers from Stanford University, led by Dr. Annst Langer-Gould, found that breastfeeding delays the exacerbation of MS after pregnancy. Typically, women with MS go into remission during pregnancy, but suffer an unusually high rate of disease exacerbations for 3–4 months. after childbirth.
In the group of women studied, 48% breastfed only for at least 2 months, and 52% did not breastfeed at all or breastfed and began supplementing in the first 2 months. after childbirth. Among women who mixed breastfeeding, the percentage of exacerbations of MS was 87%, while among women who exclusively breastfed for 2 months. exacerbation occurred in only 36%. Interestingly, 60% of women with MS chose not to breastfeed or mixed feed before starting MS medications. It was in this group that started taking medications in the first 2 months. after childbirth, there was the highest % of exacerbations. Researchers suggest that exclusive breastfeeding delays the resumption of ovulation. Lactational amenorrhea can have an anti-inflammatory effect on the body.
Literature:
- T. E. Schmidt, N. N. Yakhno “Multiple sclerosis” // Moscow “Medicine”, 2003, pp. 7–8, 79,138–139;
- A. S. Nikiforov, E. I. Gusev “Private neurology” // Moscow “GEOTAR-Media”, 2008, P. 245;-
- Maurice Victor, Allan H. Ropper, seventh edition of the “Manual of Neurology” // MIA, 2006, P 413;
- Science Daily, 2009, research;
- Article “The whole truth about anesthesia”, 2015.
Symptomatic therapy during pregnancy with MS
According to a therapeutic opinion from MS experts published in 2014, a conservative approach involves stopping all symptomatic therapy before pregnancy; if it continues, it is necessary to use the minimum effective doses of symptomatic drugs for the shortest possible period of time. Drugs for which there is no data on use during pregnancy should be avoided. Pregnant patients with MS should receive folic acid and vitamin D.
Preparing for pregnancy
The drugs used in the treatment of MS pose a danger to the child - they negatively affect the development of the fetus and can lead to serious disorders. If pregnancy occurs by accident, the woman does not know about it and continues to take medications, this can lead to tragic consequences. Therefore, it is important to plan for conception. This is done with the participation of a doctor, preferably during a period of remission.
Preparation involves constant contact with a neurologist. He will determine which medications need to be stopped a month before conception, which ones – two months, and which ones to stop six months before. Often, medication doses are reduced gradually. The doctor monitors the process and the patient’s condition.
Features of pregnancy
During pregnancy, monitoring by a neurologist is also required. It is necessary to regularly examine the neurological status and the state of lymphocytes - these tests are indicated at any time. Starting from the fourth month, it is possible to perform an MRI of the brain without the use of a contrast agent.
Management of childbirth in MS
Numerous studies on the management of childbirth in women with MS, conducted in different countries over the past 50 years, have not revealed any differences from the management of childbirth in healthy women. Both epidural anesthesia and general anesthesia are safe for MS. Neither caesarean section nor epidural anesthesia has a negative effect on the postpartum course of MS. The frequency of application of obstetric forceps or a vacuum extractor does not differ from that in healthy women [28, 29, 36, 46]. When choosing a method of delivery, it is necessary to take into account a complex of factors, including the obstetric situation, as well as the severity of the patient’s neurological deficit.
Breastfeeding in MS, taking DMTs
Some publications suggest an effect of breastfeeding on the incidence of postpartum relapses. Thus, according to B. Beaber et al. [11] and K. Hellwig et al. [39], mixed or artificial feeding leads to a significant increase in the risk of postpartum relapses compared to natural breastfeeding. In women who continued breastfeeding for at least 4 months and had lactational amenorrhea, exacerbations during the 1st year after childbirth were observed in 36% of cases, while among those who did not breastfeed - in 87%. This effect can be explained by changes in hormonal and cytokine status, since mixed or artificial feeding, which leads to early restoration of the menstrual cycle, is pro-inflammatory in nature, while exclusive breastfeeding has an anti-inflammatory effect.
There is another opinion with recommendations for a short course of breastfeeding with its complete cessation by the end of the 1st month after birth and the rapid start of taking DMTs to reduce the risk of exacerbations by the 3rd month [4].
Summarizing the available data, it is likely that at this stage an individual approach to this issue is necessary, taking into account the characteristics of the course of MS before and during pregnancy, and possible concomitant pathology. Of course, further research is needed to conclusively confirm or refute the cause-and-effect relationship between natural feeding and a reduced risk of postpartum relapses in women with MS.
According to a therapeutic opinion from MS experts published in 2014, there is no reliable evidence of either the benefits or harms of breastfeeding for patients with MS. Data on the penetration of DMTs and symptomatic drugs into breast milk and, accordingly, on the effect on newborns are limited. In general, it is recommended not to use DMTs during lactation or to discontinue breastfeeding if continued therapy is necessary. The decision to restart DMT immediately after delivery must be weighed against the potential benefits of breastfeeding.
Monitoring the course of MS during pregnancy
Currently, MRI is generally accepted as the main non-clinical method for monitoring the course of MS. In addition, MRI currently plays a significant role in clarifying the pathogenesis of MS [1]. However, when performing MRI during pregnancy, there are potential risks to the fetus, including the heating effect of radiofrequency pulses, acoustic effects, and teratogenicity. In this regard, in cases where MRI is truly a necessary study, it is recommended to postpone it until the end of the first trimester of pregnancy. However, MRI may be performed if the potential clinical benefit clearly outweighs the risk [50]. The use of intravenous gadolinium-containing contrast agents can be carried out during pregnancy only for extreme indications.
Lumbar puncture or electrophysiological tests are not associated with specific risks to the mother or fetus, but their use should be minimized due to the potential for discomfort in the pregnant woman [50].
In conclusion, once again emphasizing the multifaceted nature of the problem of managing pregnancy in MS, I would like to draw attention to the need for further research in this area, as well as the advisability of creating appropriate registries. Detailing the specific pathways of natural modulation of MS activity during pregnancy may contribute to the development of effective prognostic criteria for the course of MS in the postpartum period. Of course, large ongoing studies regarding the safety of the use of DMTs during pregnancy and lactation are extremely relevant. Finally, certain prospects may be associated with clarifying the role of sex hormones in MS, including their therapeutic potential.
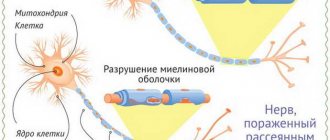
General information about RS
The development of multiple sclerosis in the human body can be viewed by comparing it to an electrical wiring system. Nerve endings have “insulation” similar to electrical wires. Wire insulation is a combination of plastic and rubber. Nerve insulation is myelin, which separates nerve fibers from each other and facilitates the smooth passage of impulses to a specific target. A compromised immune system simply begins to “devour” myelin, leaving nerve endings without insulation. This leads to the fact that the signal transmitted along the nerve endings weakens or simply does not reach the target.
Multiple sclerosis most often occurs in young people aged 15 to 25 years, less often from 25 to 45 years, very rarely after fifty. There are three times more women suffering from it than men.
Statistics show that in each individual country, per hundred thousand people, the number of patients will be different: in Russia - 40, in Holland - 128, and in Norway - 180.
A person suffering from multiple sclerosis experiences symptoms that interfere with normal life. These are various vision problems, impaired coordination of movements, memory and speech disorders. The patient feels constant fatigue and weakness throughout the body and, first of all, in the limbs. In the early stages of the disease, the symptoms are mild - this makes it difficult to diagnose the body and, accordingly, make a diagnosis. If you do not pay attention to minor symptoms, a person can live for several years with the disease without even knowing that he is sick.